Translate this page into:
Electroencephalography as a Diagnostic Aid in a Girl with Neuroregression and Stereotypies
Hansashree Padmanabha, MBBS, MD, DM Department of Neurology, National Institute of Mental Health and Neurosciences, Near Diary Circle Hosur Road, Bengaluru, 560029, Karnataka India hansa777@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Private Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Electroencephalography (EEG) in Rett’s syndrome is usually abnormal, even in the absence of clinical seizures, and it varies depending on the clinical stage of disease. The authors describe the developmental EEG pattern in a 3-year-old girl with Rett’s syndrome and highlight the importance of routinely performing EEG in a girl child presenting with language regression and stereotypies.
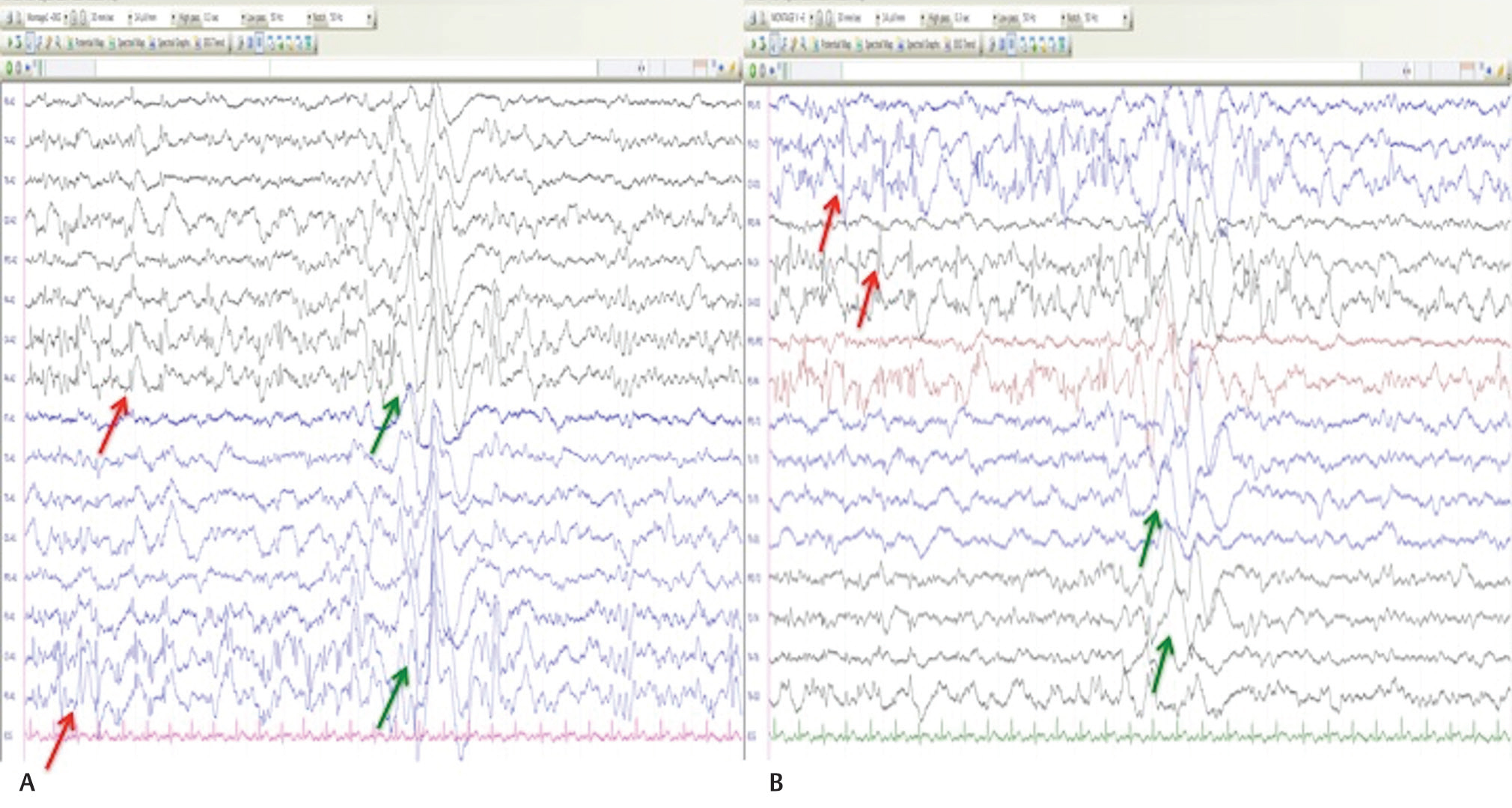
A 3-year-old girl, firstborn of nonconsanguineous couple, presented with regression of language milestones from 1½ years of age. In addition, she had loss of purposeful hand skills, repeated hand mouthing, teeth grinding, and occasional hyperventilating episodes. Family history was noncontributory. On examination, the child was alert, active with preserved eye contact; had near-continuous hand flapping, and hand squeezing movements with a head circumference of 41 cm (Z score, <−3; World Health Organization [WHO]). A clinical possibility of Rett’s syndrome was considered. On investigating, EEG during sleep showed frequent, bilateral, independent, centroparietal spikes, and spike-wave discharges with bursts of synchronous slow waves and paucity of sleep markers. Brainstem auditory evoked response was normal. MRI brain showed diffuse cerebral atrophy. The genetic analysis detected a heterozygous nonsense pathogenic variant, a premature termination codon in exon-3 of the methyl-CpG-binding protein-2 gene (p.Arg282Ter) confirming the diagnosis.
A characteristic developmental EEG pattern has been described in Rett’s syndrome, which usually correlates with the clinical staging of the disease as proposed by Hagberg and Witt-Engerstrom.1 In stage 1 (early onset stagnation), EEG would usually be normal with the onset of posterior dominant occipital slowing during wakefulness. Stage 2 (rapid destructive stage) is characterized by centrotemporal spikes or sharp-wave discharges in both awake and sleep record. Tactile stimuli and stereotypic hand movements have been reported to precipitate the centrotemporal spikes during stage 2 (Fig. 1). In stage 3 (pseudostationary stage), during wakefulness, there is further background slowing with appearance of multifocal spike or sharp-wave discharges and generalized spike-slow waves with absence of sleep markers in sleep record. At stage-4 (late motor deterioration stage), there will be rhythmic theta slowing in the frontal or the frontocentral regions in addition to stage-3 abnormalities.2 To conclude, characteristic EEG patterns clubbed with clinical features, in short of genetics, acts as a useful diagnostic tool for diagnosing Rett’s syndrome in children.
-
Fig. 1 Electroencephalogram at sleep during stage 2 of clinical disease; (A) monopolar Montage showing frequent, bilateral, independent, centro-parietal spikes of 1 to 2 Hz, 50–100 μV in C3, P3, C4, P4 (red arrow), and spike-wave discharges with bursts of synchronous slow waves (green arrow) and paucity of sleep markers; (B) bipolar Montage showing similar findings.
Fig. 1 Electroencephalogram at sleep during stage 2 of clinical disease; (A) monopolar Montage showing frequent, bilateral, independent, centro-parietal spikes of 1 to 2 Hz, 50–100 μV in C3, P3, C4, P4 (red arrow), and spike-wave discharges with bursts of synchronous slow waves (green arrow) and paucity of sleep markers; (B) bipolar Montage showing similar findings.
Conflicts of interest
None declared.
References
- Rett syndrome: a suggested staging system for describing impairment profile with increasing age towards adolescence. Am J Med Genet Suppl. 1986;1:47-59.
- [Google Scholar]






