Translate this page into:
Comparison of Recovery Profiles of Patients Undergoing Endoscopic Lumbar Discectomy under Desflurane, Propofol, or Sevoflurane Anesthesia: A Randomized, Prospective, Clinical, Comparative Study
Rudrashish Haldar, MD, PDCC Department of Anaesthesiology, Sanjay Gandhi Postgraduate Institute of Medical Sciences Lucknow, Uttar Pradesh India rudrashish@yahoo.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Agents like propofol, sevoflurane, and desflurane having rapid revival of psychomotor and cognitive functions translating into reliable anesthetic recovery are chosen for day care procedures. This prospective randomized comparative study was undertaken to compare the psychomotor and cognitive functions of patients undergoing discectomy under different anesthetic strategies.
Methods Seventy-five adult American Society of Anesthesiologists grade I and II patients being operated for endoscopic lumbar discectomy under different anesthetic regimens were enrolled and were subjected to Trieger Dot Test (TDT), Digit Symbol Substitution Test (DSST), and Mini-Mental State Examination (MMSE) preoperatively at specified intervals postoperatively. There emergence and early recovery times, complications, and satisfaction levels were also noted.
Results No difference was found in the postoperative TDT and DSST and MMSE scores among the groups at all the time points (15 minutes, 3 minutes, 1 hour, 2 hours, 3 hours, and 4 hours). TDT and DSST demonstrated a tendency to return to baseline by 2nd and 3rd hour postoperatively. Emergence and early recovery times were earlier in the inhalation groups (p 0.005 and 0.007, respectively). Time required to attain a Modified Aldrete Score of 9, complications, and observed side effects were similar among the groups.
Conclusion Patients in the three groups had similar impairments in their psychomotor and cognitive functions which recovered at comparable time periods postoperatively. Emergence and early recovery were, however, faster in the desflurane group.
Keywords
cognitive functions
day care
lumbar discectomy
Mini-Mental State Examination
postoperative period
Introduction
Endoscopic lumbar discectomy (for disc herniation/extrusion/sequestration, and spinal stenosis) is often performed as an outpatient procedure reducing in-hospital stays, complications, and expediting discharge.1 2 Choice and the appropriate application of anesthetic techniques determines the residual effects of drugs which determines the rapidity of revival of the psychomotor and cognitive functions eventually determining the quality of postanesthetic recovery.
Psychomotor recovery following anesthesia requires integration of motor and sensory functions determining coordination, occupational, and driving skills.3 Cognitive functions are mental processes including attention, orientation, memory, executive functions, language, social cognition, and visuospatial skills. Psychomotor and cognitive well-being which are criteria for recovery from anesthesia have been previously tested using Trieger Dot Test (TDT) and Digit Symbol Substitution Test (DSST).4 5 Mini-Mental State Examination (MMSE) is used widely for assessing the cognitive functions with high sensitivity and specificity.6
Previous studies have demonstrated conflicting results, where some authors reporting better cognitive scores with intravenous agent like propofol while others suggesting better scores with inhalational agents.7 8 9 Propofol, sevoflurane, and desflurane are three drugs suited for day care practice. Although few investigations have explored the effects of either of the two anesthetic agents on psychomotor recovery and cognitive functions in the postoperative period,9 10 11 12 but none of them have compared the effect of these three agents on recovery of cognitive and psychomotor functions simultaneously.
With this consideration in the background, we designed this study with hypothesis of whether any differences exist in the psychomotor and cognitive recovery profiles of patients undergoing similar day care surgeries (endoscopic discectomies) under inhalational or intravenous anesthetic regimens. The primary objective of the study was comparing the cognitive and psychomotor recovery using TDT, DSST, and the MMSE in patients undergoing discectomies under three different anesthetic regimens. Secondary objectives were to measure the emergence and early recovery times, time needed by the patients to attain a Modified Aldrete Score (MAS) of 9 (required for satisfactory discharge from postanesthesia care unit [PACU]), patients' satisfaction levels, and incidences of postoperative complications like headache, giddiness, nausea, vomiting, or pain at the injection sites.
Materials and Methods
Study Design
The present prospective randomized trial was undertaken in a super specialty tertiary care teaching hospital in North India from April 26, 2019 to August 31, 2020. The trial was registered with the Clinical Trial Registry of India (CTRI/2019/04/018478, registered on April 8, 2019). Seventy-nine patients based on consecutive sampling were enrolled in this study (Fig. 1; CONSORT Statement). The inclusion criteria were adult patients (18–65 years) of either gender belonging to the American Society of Anesthesiologist (ASA) grade I and II, having education level of minimum 8th standard, and having single or double level disease necessitating decompression/discectomy without instrumentation.

-
Fig. 1 CONSORT Statement.
Fig. 1 CONSORT Statement.
Patient refusal, inability to read, speak, or communicate, baseline MMSE ≤ 24, patients having psychiatric illnesses/behavioral impairment, consuming antipsychotic drugs, morbid obesity or suffering from significant liver, cardiovascular, lung, kidney, known allergy to the agents studied, or past history of malignant hyperthermia, and chronic drug/alcohol usage were excluded from the study.
Ethics
Following prior approval from the Institute Ethics Committee (2018–197-MD-EXP-5 dated March 8, 2019) the eligible patients were elaborately informed regarding the study protocol and its likely harms and benefits. Following this, the patients who consented were recruited after obtaining their written and informed consent. They were also informed that they can withdraw themselves anytime from the study if they wish to. The research participants were accorded the highest ethical standards as per the Declaration of Helsinki (2013).
Minimum Sample Size Calculation
To compare the mean score of cognitive tests among three study groups, with minimum two-sided 95% confidence interval and power of 80% of the study, assuming at effect size of 0.4 (for mean difference), the minimum sample size required was 22 patients in each group. Finally, we recruited 25 patients in each group after compensating for the drop outs (Software G*Power version 3.1.9.2).
Randomization, Group Allocation, and Intervention
According to the sequence of a computer-generated random numbers placed in sealed envelopes after using unique identification code, the enrolled patients were allocated randomly into three groups, that is, desflurane (D), propofol (P), and sevoflurane (S) (1:1:1 allocation), and accordingly the respective agent was utilized during maintenance of anesthesia.
The night before surgery, before administering any premedicants, the patients who were enrolled were apprised of their inclusion in the trial and explained in detail, the manner of conducting tests of their cognitive and psychomotor functions by anesthesiologist 1. First, the patients underwent the DSST where there were different symbols for each digit from 1 to 9 and there were 30 numbers arranged randomly in a prescribed format which needed to be memorized and filled in the blank space within 90 seconds. Each correct response was awarded one mark and wrong response or a digit left blank was awarded zero marks with maximum obtainable score being 30. To avoid bias due to practice influence, a new arrangement of 30 digits was administered to the patients each time.
Thereafter, the patients were asked to attempt the TDT where the patients had to connect 41 dots arranged in a geometric pattern by a fine-tipped pencil in 40 seconds or less. On missing a dot, number of millimeters the line was away from the respective dot perpendicularly was assigned an equivalent numerical score and the total score was obtained by adding all the numerical values obtained.
Then, the patients were administered the MMSE where the patients' responses to 30 different questions were recorded and maximum score obtainable was 30. All the tests were performed three times and their mean values were taken as the baseline value.
Next morning all the patients were received by anesthesiologist 2 in the operating room who after checking the identity and consent, attached the standard monitors. Sealed envelopes with computer-generated randomization codes were opened just prior to induction to randomly allocate patients to receive either sevoflurane (group S), desflurane (group D), or propofol (group P).
Standardized induction and tracheal intubation were accomplished using injection fentanyl (1 mcg/kg), injection thiopentone sodium (3–5 mg/kg), and injection vecuronium (0.1 mg/kg) when a train of four (TOF) count of 0 was achieved. Maintenance of anesthesia was done with oxygen and air (FiO2 0.5 each) and the respective anesthetic agent depending on the allocated group of the patients by anesthesiologist 2. Group S received sevoflurane 0.6 to 2.4% (inspired) and group D received desflurane 2 to 8% (inspired) beginning immediately after induction. In group P, infusion of propofol (50–200 μg/kg/min) was started immediately after the bolus induction dose. Muscle relaxation was maintained by vecuronium infusion at the rate of 0.8 to 1.7 mcg/kg/min in all the groups. Intraoperative bispectral index was targeted to be maintained between 40 and 60 by titrating the respective anesthetic agents. Infusion of fentanyl (1.5 mcg/kg/h) for providing analgesia intraoperatively, continued during the procedure.
The patients were now turned prone and surgery commenced. A single surgeon operated on all the cases. Vital parameters were monitored continuously and recorded every 10 minutes. Mean arterial pressure (MAP) drop below 25% of preinduction value was treated initially with fluid boluses (100 mL), and if unresponsive, then with injection mephentermine 6 mg bolus. Bradycardia (heart rate < 40 beats per minute [bpm]) was corrected with atropine 0.5 mg intravenously. In case of persistent MAP > 25% of the preinduction baseline values and/or heart rate > 90 bpm suggestive of inadequate analgesia, 0.5 μg/kg of fentanyl was administered. Normocapnia was maintained (35–40 mm Hg) by adjustment of ventilatory parameters and normothermia (35.5–36.5°C) was maintained with warming blankets, covering the exposed parts of the body and infusions of warm saline. Normal saline was used for intraoperative fluid therapy which was directed by the hourly maintenance requirements and losses.
At the culmination of surgery, intravenous paracetamol (15 mg/kg) and diclofenac sodium (1 mg/kg) was administered for pain management and injection ondansetron (4 mg) for antiemetic prophylaxis. Around 30 minutes before skin closure, vecuronium infusion was stopped. When the last skin suture was applied, anesthetic drug delivery was stopped. Duration of anesthesia and surgery, fluid requirements, and the vital parameters intraoperatively which were noted in the anesthetic charts of the patients were recorded.
After dressing and positioning the patients supine, neuromuscular blockade was reversed when a TOF count of 3 was obtained and the patients were extubated. Time of emergence (time between cessation of anesthetics and spontaneous eye opening/following verbal commands) and time of early recovery (patient awake, alert, hemodynamically stable, maintaining his own airway) was noted by anesthesiologist 2. The patients were then transferred to the PACU and all three tests were again performed at 15 minutes, 30 minutes, 1 hour, 2 hours, 3 hours, and 4 hours of shifting by anesthesiologist 1.
MAS was charted every 15 minutes and time for achievement of a score of 9 was noted. Twenty-four hours thereafter during the postanesthesia rounds, any side effects like nausea, vomiting, giddiness, and injection site pain were noted. The patients also rated their satisfaction levels on a four-point scale.
Statistical Analysis
Data was expressed in mean ± standard deviation (for normally distributed continuous variables) and median (interquartile range) (nonnormal continuous variables). Numbers and percentages were used for categorical variables. To compare the means among three independent groups, one-way analysis of variance (ANOVA) was used, whereas for medians, Kruskal–Wallis H test was used. In case p-value was reported significant, multiple comparisons (using Bonferroni corrections) were employed. Doses of thiopentone, fentanyl, intraoperative fluids, blood loss, duration of surgery and anesthesia, and postoperative cognitive and psychomotor tests, emergence times, and early recovery times were compared by ANOVA (repeated measures). Proportions between the groups comparison were done by arranging data in contingency tables and analyzed using Fisher's exact test. A p-value of < 0.05 was considered as statistically significant. Statistical analyses were conducted using software “Statistical Package for Social Sciences, Version-23” (SPSS-23, IBM, Chicago, United States).
Results
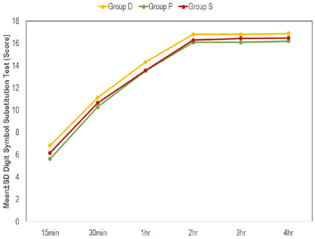
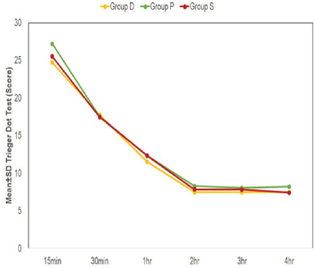
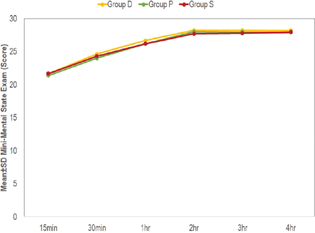
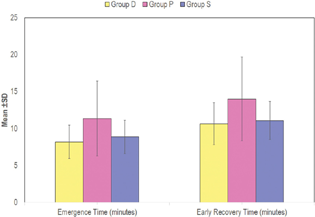
In this study, a total of 75 patients were analyzed with 25 patients in each group. Mean and median age of the study patients were 38.20 and 38.5 years with 61.3% being males. Demographic parameters (ASA status, height, weight, and body mass index) were similar among the groups. Likewise, induction doses of thiopentone, fentanyl consumption, blood loss, fluid intake, durations of surgery, and anesthesia were comparable (Table 1). Intraoperative vital parameters like systolic blood pressures, diastolic blood pressures, heart rates, temperature, oxygen saturations, and end-tidal carbon dioxide levels were also comparable (Table 2). No difference was observed among the postoperative values of DSST, TDT, and MMSE among the subjects (Table 3). Significant impairment in the tests persists up to 2 hours and beyond which they tend to recover toward the baseline values (Figs. 2,3,4). Emergence and early recovery times were faster in the inhalational anesthesia groups compared with the intravenous group (p 0.005 and 0.007, respectively) (Fig. 5). However, time needed to achieve a MAS of 9 was identical (Table 4). Similar incidences of side effects were seen and majority of the patients rated their satisfaction levels with anesthesia delivery as “good” (68, 76, and 64%, respectively) (Table 5).
|
Variables |
Group 1 (D) |
Group 2 (P) |
Group 3 (S) |
p-Value |
|---|---|---|---|---|
|
Age (y) |
36.52 ± 16.30 (39, 25–50) |
40.16 ± 13.35 (39, 25–52) |
37.76 ± 12.89 (38, 26–51) |
0.658b |
|
Sex (male)a |
15 (60) |
16 (64) |
15 (60) |
0.946 |
|
ASA grade Ia |
21 (84) |
21 (84) |
24 (96) |
0.321 |
|
ASA grade IIa |
4 (16) |
4 (16) |
1 (4) |
|
|
Height (cm) |
161.52 ± 5.71 |
160.48 ± 4.81 |
161.56 ± 6.33 |
0.747 |
|
Weight (kg) |
63.12 ± 6.72 |
62.80 ± 9.79 |
62.32 ± 9.97 |
0.951 |
|
BMI (kg/m2) |
24.21 ± 2.57 |
24.44 ± 3.08 |
23.72 ± 2.54 |
0.639 |
|
B/L Digit Symbol Substitution Test |
16.92 ± 2.77 |
16.24 ± 2.92 |
16.64 ± 2.86 |
0.699 |
|
B/L Trieger Dot Test |
7.44 ± 3.34 |
8.04 ± 3.62 |
7.36 ± 3.93 |
0.771 |
|
B/L Mini–Mental State Examination |
28.28 ± 1.79 |
28.08 ± 1.82 |
28.08 ± 1.89 |
0.906 |
|
Dose of thiopentone (mg) |
306.00 ± 29.12 |
305.00 ± 72.89 |
296.00 ± 40.62 |
0.748 |
|
Dose of fentanyl (mcg) |
152.00 ± 44.44 |
190.00 ± 88.98 |
174.00 ± 63.11 |
0.147 |
|
Total fluids (L) |
2.54 ± 0.56 |
2.60 ± 0.39 |
2.56 ± 0.63 |
0.934 |
|
Blood loss (mL) |
156.80 ± 106.21 [154, 128–174] |
174.17 ± 84.80 [164, 131–189] |
181.60 ± 119.71 [172, 133–197] |
0.214b |
|
Duration of surgery |
174.20 ± 39.63 |
179.80 ± 39.62 |
176.00 ± 38.73 |
0.876 |
|
Duration of anesthesia |
209.60 ± 41.96 |
222.20 ± 48.13 |
213.80 ± 42.21 |
0.593 |
Abbreviations: ANOVA, analysis of variance; ASA, American Society of Anesthesiologists; BMI, body mass index; B/L, baseline; IQR, interquartile range; SD, standard deviation.
Note: Percentages are given within parenthesis. For skewed data, median (IQR) also given with mean ± SD. For normal continuous data, mean ± SD, one-way ANOVA test used. p < 0.05 significant.
|
Preinduction |
30 min |
1 h |
2 h |
3 h |
4 h |
5 h |
|
|---|---|---|---|---|---|---|---|
|
SBP |
|||||||
|
Group D (n = 25) |
126.44 ± 9.69 |
117.28 ± 11.29 |
114.52 ± 9.64 |
116.64 ± 8.08 |
117.9 ± 9.4 (n = 24) |
117.42 ± 10.81 (n = 19) |
121.08 ± 15.55 (n = 12) |
|
Group P (n = 25) |
126.48 ± 15.98 |
116.44 ± 14.66 |
113.96 ± 11.2 |
115.16 ± 9.03 |
119.48 ± 8.01 |
123.67 ± 13.22 (n = 15) |
116.64 ± 12.44 (n = 11) |
|
Group S (n = 25) |
122.48 ± 11.64 |
115.44 ± 12.34 |
114.6 ± 10.47 |
113.96 ± 12.73 |
117.91 ± 9.86 (n = 22) |
118.67 ± 9.8 (n = 18) |
112.75 ± 9.99 (n = 12) |
|
p-Value |
0.446 |
0.879 |
0.973 |
0.647 |
0.792 |
0.256 |
0.298 |
|
DBP |
|||||||
|
Group D (n = 25) |
77.16 ± 7.61 |
70.88 ± 6.68 |
60.24 ± 6.46 |
71.16 ± 7.24 |
71.71 ± 6.29 (n = 24) |
73.47 ± 4.77 (n = 19) |
75.67 ± 11.79 (n = 12) |
|
Group P (n = 25) |
78.68 ± 9.60 |
72.24 ± 10 |
69.72 ± 7.74 |
71.28 ± 9.34 |
74.76 ± 7.42 |
77.40 ± 10.79 (n = 15) |
72.73 ± 10.50 (n = 11) |
|
Group S (n = 25) |
76.68 ± 7.34 |
72.20 ± 9.53 |
69.52 ± 13.09 |
73.48 ± 10.11 |
73.50 ± 7.07 (n = 22) |
73.67 ± 7.51 (n = 18) |
69.83 ± 4.57 (n = 12) |
|
p-Value |
0.674 |
0.827 |
0.984 |
0.591 |
0.311 |
0.286 |
0.204 |
|
HR |
|||||||
|
Group D (n = 25) |
80.72 ± 9.25 |
75.56 ± 9.33 |
74.32 ± 7.68 |
75.48 ± 7.13 |
76.00 ± 7.14 |
76.11 ± 9.42 |
73.83 ± 8.84 |
|
Group P (n = 25) |
81.44 ± 10.87 |
77.60 ± 10.49 |
75.40 ± 9.91 |
76.88 ± 8.51 |
77.00 ± 9.20 |
82.93 ± 10.75 |
79.82 ± 7.92 |
|
Group S (n = 25) |
79.20 ± 10.10 |
76.92 ± 10.33 |
73.40 ± 8.19 |
74.52 ± 8.45 |
76.81 ± 8.18 |
78.39 ± 7.71 |
73.75 ± 6.77 |
|
p-Value |
0.727 |
0.767 |
0.716 |
0.584 |
0.896 |
0.111 |
0.107 |
|
Temperature |
|||||||
|
Group D (n = 25) |
36.14 ± 0.24 |
36.10 ± 0.29 |
36.08 ± 0.31 |
36.09 ± 0.29 |
36.06 ± 0.19 |
36.10 ± 0.30 |
36.21 ± 0.36 |
|
Group P (n = 25) |
36.17 ± 0.38 |
36.17 ± 0.39 |
36.11 ± 0.35 |
36.16 ± 0.37 |
36.18 ± 0.42 |
36.28 ± 0.37 |
36.44 ± 0.36 |
|
Group S (n = 25) |
36.10 ± 0.33 |
36.06 ± 0.25 |
36.05 ± 0.33 |
36.06 ± 0.34 |
36.11 ± 0.31 |
36.06 ± 0.31 |
36.13 ± 0.33 |
|
p-Value |
0.781 |
0.470 |
0.653 |
0.533 |
0.415 |
0.127 |
0.209 |
|
SPO2 |
|||||||
|
Group D (n = 25) |
99.84 ± 0.55 |
99.84 ± 0.47 |
99.84 ± 0.55 |
99.84 ± 0.55 |
99.88 ± 0.45 |
99.89 ± 0.32 |
100.00 ± 00 |
|
Group P (n = 25) |
99.88 ± 0.44 |
99.88 ± 0.44 |
99.88 ± 0.44 |
100.00 ± 00 |
99.96 ± 0.20 |
99.87 ± 0.52 |
99.82 ± 0.6 |
|
Group S (n = 25) |
99.64 ± 0.91 |
99.68 ± 0.85 |
99.80 ± 0.65 |
99.92 ± 0.40 |
99.82 ± 0.59 |
99.89 ± 0.47 |
100 ± 00 |
|
p-Value |
0.439 |
0.483 |
0.878 |
0.363 |
0.532 |
0.981 |
0.346 |
|
ETCO2 |
|||||||
|
Group D (n = 25) |
33.04 ± 1.62 |
33.00 ± 2.04 |
32.52 ± 2.43 |
32.79 ± 1.35 |
33.11 ± 2.85 |
32.33 ± 1.44 |
|
|
Group P (n = 25) |
32.88 ± 2.01 |
33.04 ± 1.59 |
32.76 ± 1.64 |
32.24 ± 1.56 |
32.67 ± 1.95 |
33.00 ± 2.10 |
|
|
Group S (n = 25) |
33.64 ± 2.20 |
33.20 ± 1.53 |
32.84 ± 1.70 |
32.95 ± 1.68 |
33.00 ± 0.91 |
32.75 ± 1.06 |
|
|
p-Value |
0.355 |
0.911 |
0.835 |
0.246 |
0.823 |
0.592 |
|
Abbreviations: ANOVA, analysis of variance; DBP, diastolic blood pressure; ETCO2, end-tidal carbon dioxide level; HR, heart rate; SBP, systolic blood pressure; SD, standard deviation; SPO2, oxygen saturation.
Note: Mean ± SD, one-way ANOVA test used to compare means among the three study groups. p < 0.05 significant.
|
DSST |
||||||
|---|---|---|---|---|---|---|
|
15 min |
30 min |
1 h |
2 h |
3 h |
4 h |
|
|
Group D (n = 25) |
6.84 ± 5.32 |
11.12 ± 5.01 |
14.32 ± 3.50 |
16.80 ± 2.71 |
16.80 ± 2.89 |
16.88 ± 2.74 |
|
Group P (n = 25) |
5.64 ± 5.28 |
10.28 ± 4.50 |
13.52 ± 3.43 |
16.08 ± 2.63 |
16.08 ± 2.68 |
16.20 ± 2.57 |
|
Group S (n = 25) |
6.16 ± 5.14 |
10.64 ± 4.99 |
13.56 ± 3.65 |
16.28 ± 2.32 |
16.44 ± 2.42 |
16.48 ± 2.73 |
|
p-Value |
0.721 |
0.829 |
0.666 |
0.592 |
0.636 |
0.667 |
|
TDT |
||||||
|
15 min |
30 min |
1 h |
2 h |
3 h |
4 h |
|
|
Group D (n = 25) |
24.72 ± 10.66 |
17.76 ± 8.61 |
11.52 ± 4.74 |
7.48 ± 2.65 |
7.48 ± 3.42 |
7.48 ± 3.34 |
|
Group P (n = 25) |
27.20 ± 11.11 |
17.56 ± 6.47 |
12.32 ± 4.54 |
8.28 ± 2.57 |
8.04 ± 3.03 |
8.20 ± 3.64 |
|
Group S (n = 25) |
25.52 ± 11.24 |
17.48 ± 8.76 |
12.32 ± 5.74 |
7.84 ± 3.14 |
7.80 ± 3.59 |
7.40 ± 3.86 |
|
p-Value |
0.719 |
0.992 |
0.811 |
0.602 |
0.840 |
0.692 |
|
MMSE |
||||||
|
15 min |
30 min |
1 h |
2 h |
3 h |
4 h |
|
|
Group D (n = 25) |
21.64 ± 2.16 |
24.64 ± 2.45 |
26.68 ± 2.39 |
28.24 ± 1.59 |
28.24 ± 1.56 |
28.20 ± 1.68 |
|
Group P (n = 25) |
21.40 ± 2.08 |
24.00 ± 1.94 |
26.20 ± 2.04 |
28.04 ± 1.62 |
27.96 ± 1.67 |
27.92 ± 1.66 |
|
Group S (n = 25) |
21.68 ± 2.50 |
24.32 ± 2.53 |
26.20 ± 2.43 |
27.72 ± 1.77 |
27.80 ± 1.50 |
27.96 ± 1.88 |
|
p-Value |
0.893 |
0.623 |
0.696 |
0.539 |
0.610 |
0.828 |
Abbreviations: ANOVA, analysis of variance; DSST, Digit Symbol Substitution Test; MMSE, Mini-Mental State Examination; SD, standard deviation; TDT, Trieger Dot Test.
Note: Mean ± SD, one-way ANOVA test used to compare means among three study groups. p < 0.05 significant.
|
Parameters |
Group D (n = 25) |
Group P (n = 25) |
Group S (n = 25) |
p-Value |
|---|---|---|---|---|
|
Emergence time (min) |
8.18 ± 2.26 |
11.35 ± 5.08 |
8.88 ± 2.25 |
0.005a |
|
Early recovery time (min) |
10.63 ± 2.85 |
13.99 ± 5.67 |
11.08 ± 2.58 |
0.007a |
|
Time taken to achieve MAS of 9 (min) |
148.20 ± 38.81 |
143.60 ± 31.04 |
148.20 ± 39.76 |
0.878 |
Abbreviations: ANOVA, analysis of variance; MAS, Modified Aldrete Score; SD, standard deviation.
Note: Mean ± SD, one-way ANOVA test used to compare means among three study groups. Bonferroni correction methods used for multiple comparisons.
|
A: Comparison of side effects observed within the groups |
||||||
|---|---|---|---|---|---|---|
|
Giddiness |
Headache |
Nausea |
Vomiting |
Pain at injection site |
p-Value |
|
|
Group D (n = 25) |
1 (4%) |
1 (4) |
4 (16%) |
3 (12%) |
0 (0%) |
0.651 |
|
Group P (n = 25) |
1 (4%) |
0 |
1 (4%) |
1 (4%) |
0 (0%) |
|
|
Group S (n = 25) |
0 (0%) |
1 (4%) |
2 (8%) |
2 (8%) |
0 (0%) |
|
|
B: Comparison of ratings of the quality of anesthesia delivery by the patients |
||||||
|
Excellent |
Good |
Fair |
Poor |
p -Value |
||
|
Group D (n = 25) |
8 (32%) |
17 (68%) |
0 (0%) |
0 (0%) |
0.568 |
|
|
Group P (n = 25) |
5 (20%) |
19 (76%) |
1 (4%) |
0 (0%) |
||
|
Group S (n = 25) |
7 (28%) |
16 (64%) |
2 (8%) |
0 (%) |
||
Note: Data expressed in numbers and percentage, Fisher's exact test used. p < 0.05 significant.
-
Fig. 2 Intragroup change in Digit Symbol Substitution Test (as compared with baseline) at different time intervals.
Fig. 2 Intragroup change in Digit Symbol Substitution Test (as compared with baseline) at different time intervals.
-
Fig. 3 Intragroup change in Trieger Dot Test scores (as compared with baseline) at different time intervals.
Fig. 3 Intragroup change in Trieger Dot Test scores (as compared with baseline) at different time intervals.
-
Fig. 4 Intragroup change in Mini–Mental State Examination scores (as compared with baseline) at different time intervals.
Fig. 4 Intragroup change in Mini–Mental State Examination scores (as compared with baseline) at different time intervals.
-
Fig. 5 Comparison of emergence times and early recovery time in between the groups.
Fig. 5 Comparison of emergence times and early recovery time in between the groups.
Discussion
For day care surgeries, agents like desflurane, sevoflurane, and propofol having short duration and least effect on cognitive and psychomotor functions ensuring reliable recovery are preferred.13 Propofol has been implicated in the development of cognitive defects resulting from hippocampal neuroapoptosis and expression of inflammatory cytokines.14 Similarly, isoflurane, which is an isomer of desflurane, is presumed to cause neurotoxicity due to neuroinflammation, caspase activation, and apoptosis.15 In our randomized prospective study, we compared the cognitive and psychomotor recovery profiles of 75 patients undergoing discectomy under general anesthesia maintained with either desflurane or propofol or sevoflurane by administering them DSST, TDT, and MMSE tests at specified time points postoperatively and comparing it with their preoperative performances by a blinded anesthesiologist.
TDT and DSST are commonly used pencil-and-paper psychomotor tests. TDT is easy, inexpensive, and is free of practice effects.16 DSST involves memory processing, cognitive functions, psychomotor function, recognition of sensory (visual) information, mental concentration, fine muscular coordination, and ability to alter eye fixation.17 18 Recovery from anesthesia is indicated through recovery of psychomotor function when assessed using these tests.19 MMSE (Folstein test) is used widely for assessing the cognitive functions with high sensitivity and specificity.20 Preoperative values of psychomotor and cognitive profiles of our study patients were similar.
No difference was found in the TDT and DSST scores in the postrecovery period of 15 minutes, 30 minutes, 1st hour, 2nd hour, 3rd hour, and 4th hour in our study. Similar study in subjects undergoing elective day care procedures and assessing their cognitive and ambulatory functions using TDT and DSST observed that there were no intergroup differences in TDT and DSST scores in the observed time periods. Performances in both groups were impaired for around 2 hours, after which the performances recovered to baseline levels. Similar levels of impairment at each time interval was observed between the two groups.10 A study on recovery profiles of patients undergoing nasal surgical procedures using sevoflurane and propofol assessing the psychomotor recovery by TDT and DSST at 15, 30, and 45 minutes found that at 45 minutes, readings of the patients differed significantly.21 The discordance observed in their study compared with ours might be due to the variance in the type of surgery and the patient profile (18–35 years). Additionally, they had used cisatracurium in their anesthetic protocol which has a faster metabolism and might be attributing to the difference.
MMSE scores in the postrecovery period in the different groups were found to be similar (p > 0.05). Chen et al reported similarity between the desflurane and sevoflurane groups in terms of MMSE with significantly lower values in the first postoperative hour than the baseline values. Overall, 85% of patients regained initial values by the 3rd hour and all patients returned to the initial MMSE values by 24 hours.22 We also observed that lowered MMSE values in first postoperative hour and most of our patients returned to initial values by 3rd hour postoperatively. In patients undergoing laparoscopic cholecystectomy with preoperative MMSE scores > 23 in both groups (propofol and sevoflurane) it was observed that postoperatively no difference in MMSE scores at 4 hours was seen which was similar to our study.9
Emergence and early recovery when compared in our study showed that compared with sevoflurane (8.88 ± 2.25 minutes) and propofol (11.35 ± 5.08 minutes), patients in the desflurane group (8.18 ± 2.26 minutes) had lesser emergence times and early recovery times. This was in concordance with a previous study in patients undergoing urological cystoscopic surgery resulting in patients receiving desflurane having faster emergence times than sevoflurane.23 Likewise, in children undergoing spinal dysraphism surgery, shorter emergence time was observed in the desflurane group (2.75 [0.85–12] minutes) compared with sevoflurane (8 [2.5–14] minutes).24 Tian et al comparing the effects of propofol and sevoflurane on perioperative inflammatory response, pulmonary function, and cognitive function in lung cancer patients observed that times for extubation, eye opening, and response in the propofol group were significantly shorter.25 However, in elective supratentorial craniotomies, times to respond to verbal commands were significantly prolonged with sevoflurane (8.0 ± 2.9 minutes) compared with propofol (5.3 ± 2.9 minutes) and desflurane (5.2 ± 2.6 minutes) (p = 0.003).26 The difference observed in their study might be due to the nature of surgery (intracranial) and due to use of nitrous oxide along with anesthetic agent in their study.
The present study demonstrated that the mean time taken to achieve MAS of 9 was similar in all the three groups. Ergönenç et al studied the recovery times from sevoflurane and desflurane anesthesia and the time required to reach an MAS of 8. They found that the mean time to reach MAS of 8 was significantly higher than in sevoflurane compared with the desflurane group.27 The difference may be attributed to the duration of recording (up to 1 hour only) and the endpoints (MAS of 8 vs. MAS of 9).
Among adverse effects a higher incidence of postoperative nausea and vomiting was reported in the sevoflurane and desflurane groups. Similar findings were reported previously where postoperative nausea and vomiting was less in the propofol group compared with the inhalational group.10 28 Satisfaction levels reported by the patients were identical with majority rating the quality of the anesthesia administered to them as “good' as observed earlier.10
The strengths of the study were it being adequately powered and enrolling required number of patients. The nature of surgery, type of anesthesia, resources, and practice of assessment of the cognitive testing surgery remained uniform. The limitations also deserve mention. The psychomotor and cognitive tests (TDT, DSST, and MMSE) employed paper-and-pencil tests which are influenced by practice effect with a tendency to improve with repeated testing. Though we tried to provide different patterns, practice effect cannot be completely ruled out. Preoperative assessments of cognitive functions were done 12 to 24 hours prior where pain and preoperative anxiety might confound baseline values. Double blinding was not possible for obvious reasons. Earlier achievement of MAS 9 by few minutes in the propofol group has doubtful clinical significance. Parameters like early motor activity, ambulation, oral intake, voiding, etc. are important to estimate the surgical recovery but these were not assessed in our study. Finally, the study was terminated in the early part of the recovery period and long-term outcome assessment and follow-up of the patients were not performed.
Conclusion
To summarize, the psychomotor and cognitive functions of patients undergoing lumbar discectomy under desflurane or propofol or sevoflurane anesthesia remain similar in the early postoperative period with similar incidences of side effects. The emergence times and early recovery times, however, was observed to be longer in the propofol group with similar time periods required to attain a MAS of 9 and similar incidences of complications.
Conflict of Interest
None declared.
Funding None.
References
- Day case lumbar discectomy–viable option in the UK? Br J Neurosurg. 2014;28(3):320-323.
- [Google Scholar]
- Development of an outpatient protocol for lumbar discectomy: our institutional experience. World Neurosurg. 2014;82(5):897-901.
- [Google Scholar]
- Psychomotor recovery of dexmedetomidine compared with propofol after sedation during spinal anesthesia: a randomized control trial. J Anaesthesiol Clin Pharmacol. 2019;35(2):236-241.
- [Google Scholar]
- Measuring recovery from anesthesia–a simple test. Anesth Analg. 1969;48(1):136-140.
- [Google Scholar]
- Recovery and neurological examination after remifentanil-desflurane or fentanyl-desflurane anaesthesia for carotid artery surgery. Br J Anaesth. 2001;86(1):44-49.
- [Google Scholar]
- Consequences of not recognizing delirium superimposed on dementia in hospitalized elderly individuals. J Gerontol Nurs. 2000;26(1):30-40.
- [Google Scholar]
- Effect of anesthetic agents on cognitive function and peripheral inflammatory biomarkers in young patients undergoing surgery for spine disorders. Asian J Neurosurg. 2019;14(4):1095-1105.
- [Google Scholar]
- Postoperative cognitive dysfunction after inhalational anesthesia in elderly patients undergoing major surgery: the influence of anesthetic technique, cerebral injury and systemic inflammation. BMC Anesthesiol. 2015;15:154.
- [Google Scholar]
- Comparative evaluation of the effects of propofol and sevoflurane on cognitive function and memory in patients undergoing laparoscopic cholecystectomy: a randomised prospective study. Indian J Anaesth. 2015;59(3):150-155.
- [Google Scholar]
- Comparison of cognitive, ambulatory, and psychomotor recovery profiles after day care anesthesia with propofol and sevoflurane. J Anesth. 2014;28(6):833-838.
- [Google Scholar]
- Recovery profile of patients undergoing nasal surgical procedures: a comparison between sevoflurane and propofol. Indian J Otolaryngol Head Neck Surg. 2008;60(2):123-127.
- [Google Scholar]
- Comparison between sevoflurane and desflurane on emergence and recovery characteristics of children undergoing surgery for spinal dysraphism. Indian J Anaesth. 2015;59(8):482-487.
- [Google Scholar]
- A comparative study of the use of sevoflurane and propofol in ambulatory surgery [in German] Anaesthesist. 1996;45(01):S57-S62.
- [Google Scholar]
- Long-term action of propofol on cognitive function and hippocampal neuroapoptosis in neonatal rats. Int J Clin Exp Med. 2015;8(7):10696-10704.
- [Google Scholar]
- The effects of isoflurane and desflurane on cognitive function in humans. Anesth Analg. 2012;114(2):410-415.
- [Google Scholar]
- Recovery of psychomotor function after total intravenous anesthesia with remifentanil-propofol or fentanyl-propofol. J Anesth. 2012;26(1):34-38.
- [Google Scholar]
- Analgesic and sedative effects of intranasal dexmedetomidine in third molar surgery under local anaesthesia. Br J Anaesth. 2011;107(3):430-437.
- [Google Scholar]
- The efficacy, side effects, and recovery characteristics of dexmedetomidine versus propofol when used for intraoperative sedation. Anesth Analg. 2002;95(2):461-466.
- [Google Scholar]
- Time course of psychomotor recovery after intravenous dexmedetomidine infusion as a part of balanced anaesthetic technique: a randomised, double-blind study. Indian J Anaesth. 2019;63(8):623-628.
- [Google Scholar]
- Consequences of not recognizing delirium superimposed on dementia in hospitalized elderly individuals. J Gerontol Nurs. 2000;26(1):30-40.
- [Google Scholar]
- Recovery profile of patients undergoing nasal surgical procedures: a comparison between sevoflurane and propofol. Indian J Otolaryngol Head Neck Surg. 2008;60(2):123-127.
- [Google Scholar]
- The recovery of cognitive function after general anesthesia in elderly patients: a comparison of desflurane and sevoflurane. Anesth Analg. 2001;93(6):1489-1494.
- [Google Scholar]
- Desflurane allows for a faster emergence when compared to sevoflurane without affecting the baseline cognitive recovery time. Front Med (Lausanne). 2015;2:75.
- [Google Scholar]
- Comparison between sevoflurane and desflurane on emergence and recovery characteristics of children undergoing surgery for spinal dysraphism. Indian J Anaesth. 2015;59(8):482-487.
- [Google Scholar]
- Effects of propofol or sevoflurane anesthesia on the perioperative inflammatory response, pulmonary function and cognitive function in patients receiving lung cancer resection. Eur Rev Med Pharmacol Sci. 2017;21(23):5515-5522.
- [Google Scholar]
- Comparative evaluation of propofol, sevoflurane and desflurane for neuroanaesthesia: a prospective randomised study in patients undergoing elective supratentorial craniotomy. Indian J Anaesth. 2015;59(5):287-294.
- [Google Scholar]
- The recovery time of sevoflurane and desflurane and the effects of anesthesia on mental and psychomotor functions and pain. Anesth Essays Res. 2014;8(3):367-371.
- [Google Scholar]
- The impact of isoflurane, desflurane, or sevoflurane on the frequency and severity of postoperative nausea and vomiting after lumbar disc surgery. J Clin Anesth. 2007;19(3):180-185.
- [Google Scholar]






