Translate this page into:
Single photon emission computed tomography scanning: A predictor of outcome in vegetative state of head injury
Address for correspondence: Dr.PK Pralaya Nayak, 82, Royal Garden, Patia, Bhubaneswar-751 031, India. E-mail: drmichaelpn@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Neurotrauma is one of the most important causes of death and disability. Some of the severely head injured patients, failed to show significant improvement despite aggressive neurosurgical management and ended up in a vegetative state.
Aims:
To assess the outcome at six months and one year using Glasgow outcome scale (GOS), in this prospective study on patients with severe head injury, who remained vegetative at one month.
Materials and Methods:
This prospective study was carried out in the department of Neurosurgery, All India Institute of Medical Sciences (AIIMS), New Delhi, over a period of a year and a half (March 2002 through July 2003). Materials and Methods: In patients with severe head injury (GCS < 8), post resuscitation, neurological assessment was done with Glasgow coma scale (GCS), pupillary light reflex, doll's eye movement and cold caloric test in all cases. Fifty patients, who remained vegetative post injury according to the criteria of Jennett and Plum, at one month, were considered for the study. Brain SPECT (Single Photon Emission Computed T omography) Scanning was carried out in selected cases. Statistical analysis: Data analysis was done by Pearson's chi-square test on computer software SPSS, Version 10 (California, USA).
Results:
Patients with preserved brainstem reflex and with no perfusion defect on SPECT scan had statistically significant favorable outcome. More than 40% of vegetative patients regained consciousness by the end of one year, of whom 24% had favorable outcome in the form of moderate disability and good recovery.
Conclusion:
SPECT is better than computed tomography/magnetic resonance imaging (CT/MRI) as it assesses the cerebral perfusion and functional injury rather than detecting the lesions only. Further study with a control group is necessary to establish the role of SPECT in head injury.
Keywords
Glasgow outcome scale
severe head injury
single photon emission computed tomography
vegetative state
Introduction
Neurotrauma is one of the most important causes of death and disability in our country, involving all age groups due to increase in road-traffic accidents. Some of the severely head-injured patients failed to show significant improvement despite aggressive neurosurgical intervention, intensive care management and ultimately ended up in a vegetative state. In the past, efforts have been made to study the factors involved in adverse outcome following head injury and to predict the long-term outcome.
Jennett and Plum did not specify the minimum duration of posttraumatic vegetative state to be considered persistent.[1] However, serial observations have shown that severely head-injured patients are rarely capable of comprehending simple commands within one year, if they have not done so by six months.[2]
This prospective study was designed to study the outcome at one year, in patients who remained vegetative at one month post injury and to assess if any factors had a bearing on the outcome.
Materials and Methods
This prospective study was carried out in the department of Neurosurgery, All India Institute of Medical Sciences (AIIMS), New Delhi, over a period of a year and a half (March 2002 through July 2003). All the severe head injury patients admitted in our department, were intubated in casualty to secure the airway. Patients of severe head injury (GCS ≤ 8) post resuscitation, after initial neurological evaluation along with CT scan of brain, were admitted to the intensive care unit (ICU). The neurological assessment was done with Glasgow coma scale (GCS), pupillary light reflex, doll's eye movement and cold caloric test in all cases.[3]
Patients who remained vegetative post injury at one month were considered for the study. The criteria for vegetative state were:[4]
-
Spontaneous respiration and heart beat
-
No life support machinery
-
Body functions normally
-
Sleep awake cycles
-
Swallowing but not safely and sufficiently (hence on tube feeding)
-
No intellectual activities
-
No rational response
-
No cognitive function
-
No sentience
Those patients who improved after treatment to motor response M6 or died within one month were excluded from the study. None of these patients were having poly trauma. Fifty vegetative patients were included in our study. Brain SPECT was carried out over a period of one to two months post injury. In some cases SPECT was not possible, because some patients were restless or due to medical grounds.
Magnetic resonance imaging brain
Flair T1W sagittal and fast spin echo T2W high-resolution axial images of brain were obtained on a dedicated phased array head coil using 1.5 Tesla high-gradient systems (Magnetom, Sonata, Germany) and correlated with T2 flair coronal images.
Brain spect
SPECT was performed in a silent room with eyes open and ears unplugged, 45 min after intravenous injection of 555-925 MBq (15-25 mCi) 99mTc-ECD (BARC, Mumbai). Acquisition was done on a dual-headed rotating scintillation gamma camera (Elscint, Varicam) with the patient in supine position, headrest attached, smallest permissible radius of rotation was used with 128 × 128 matrix of acquisition, 360°rotation, 120 projections, 25 sec per projection, acquired in low-energy high-resolution parallel hole collimator. Final data was displayed using 10-graded color scale. Total tracer count in units was measured in color coding; white denotes maximum tracer uptake and blue/black minimum. The cerebellum was used as reference site (100% maximum value). Any decrease in cerebral perfusion in the cortex or basal ganglia below 70% or below 50% in the medial temporal lobe was considered abnormal. This method has been described earlier.[5] Cerebellar lesions were considered, if difference in uptake between the two lobes was more than 10%. If the cerebellum showed decreased radiotracer uptake then the occipital lobe was used as reference. Two independent observers interpreted the SPECT images.
After being discharged from the hospital patients were followed up in the Neurosurgery outpatients department (OPD) and the outcome was assessed at six months and one year using Glasgow outcome scale (GOS), according to the five-point scale developed by Jennett and Bond in 1975.[6]
-
Death
-
Persistent vegetative state (cortex structurally intact but not functioning)
-
Severely disabled (conscious but disabled)
-
Moderately disabled (disabled but independent, hemiparesis, ataxia, intellectual and memory deficit, personality changes)
-
Good recovery (minor neurological and psychological deficit)
Death, persistent vegetative state (PVS) and severely disabled states are considered as unfavorable outcomes, similarly, moderate disability and good recovery are known as favorable outcomes.
Statistic
Statistical data analysis was done by Pearson's chi-square test on computer software SPSS, Version 10 (California, USA).
Results
Fifty patients were included in the study out of which 44 patients were male and six patients were female. The age group was between 6 to 60 years with a mean age of 34.22±15.4 years. The commonest mode of injury was road traffic accident in 38 (76%) patients, followed by fall from height (nine, 18%). Assault was the cause of injury in two (4%) cases and one patient was caught in the machine.
As all the patients were intubated and to overcome the fallacy of eye opening, best motor response was considered for outcome prediction. Out of 50 patients 18 patients were M1-M2, 14 were M3-M4 and 18 patients were M5 at presentation.
CT scan of brain
CT scan revealed EDH(Extra dural haematoma) in one patient (2%), SDH(Intra dural haematoma) in four patients (8%), contusion in 25 patients (50%) out of which it was one to two in number in two patients (8%) and multiple in 23 patients (72%). Combined lesions were noticed in 16 patients (32%). The remaining four patients (8%) had no lesion detected on CT. Contusions were recorded in temporal lobes in 11 patients (27%), frontal lobes in six patients (14%) and in multiple lobes in 22 patients (54%) and were cerebellar in two patients (5%). Contusions were present unilaterally in 30 patients (73%) and bilaterally in 10 patients (27%). Midline shift was noticed in 19 patients (38%) and newer lesions were detected on repeat CT in four patients (8%).
Magnetic resonance imaging brain
Thirty-seven patients underwent MRI study, which revealed normal study in seven patients (18.9%). Abnormalities in the form of gliosis and postoperative changes along with hydrocephalus were noted in nine patients (24.3%). A few contusions in the lobes were found in four patients (10.8%) and multiple small contusions in the upper brainstem, splenium of corpus callosum, grey white junction and cerebellar peduncles suggestive of diffuse axonal injury were noted in 17 patients (46%).
Five remained M1-M2, 10 M3-M4 and 35 improved to M5 at the end of one month. Patients who remained with M1 and M2 motor response, PVS was observed in 11 patients (61%) and death in three patients (17%). So an unfavorable outcome was noted in 16 patients (89%). Twelve patients (86%) had an unfavorable outcome with M3 to M4 response, out of which PVS was observed in five patients, six were severely disabled and one died. Among the patients who had the best motor response, M5, five patients (28%) remained vegetative and three died (17%), the rest were severely disabled and a good outcome was noted in seven patients (39%). Favorable outcome was observed in patients with good GCS (P value < 0.03).
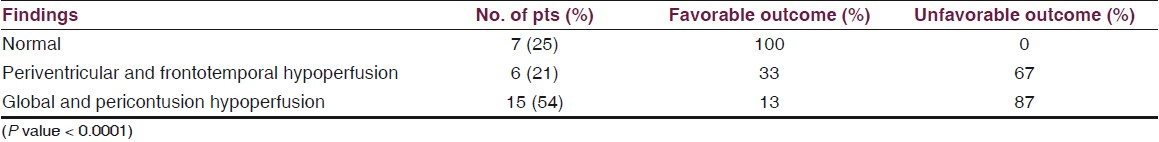
It was possible to perform the SPECT study in 28 patients. Normal cerebral perfusion was observed in seven patients (25%). Out of nine patients with posttraumatic hydrocephalus on CT, gross abnormalities of perfusion around the periventricular region and bilateral temporal and frontal lobes were observed in six patients (21%). In 15 patients (54%), marked hypoperfusion either in the temporal or frontal lobes, subcortical reduction in blood flow and increased perfusion defect was noted in the pericontusion area, which were bigger than the size of the contusions seen on CT scan.
Seventeen (81%) had poor outcome with perfusion defect and four patients (19%) died. Six patients became severely disabled and seven patients (47%) remained vegetative with gross perfusion abnormalities in global as well as in affected lobes. Only four (19%) had good outcome in that the patient remained moderately disabled. In seven patients (25%) where SPECT study was normal, all showed favorable outcome (P value < 0.0001) [Table 1].
In the other 22 patients in whom SPECT could not be performed, outcome were assessed with other factors, like pupillary reaction (P value= 0.94), doll's eye movement (P value < 0.014), cold caloric test (P value < 0.0001), lesions in CT scan (P value < 0.39) and diffuse axonal injury as compared to focal pathology in MRI (P value < 0.001).
In a series of 50 cases in our study, seven (14%) vegetative patients died by the end of one year, out of which five deaths occurred prior to six months. Twenty-one (42%) patients remained vegetative and 10 (20%) improved to a severe disabled state. An overall unfavorable outcome was noted at the end of one year in 38 (76%) cases and favorable outcome in 12 (24%) patients. More than 40% vegetative patients regained consciousness by the end of one year [Table 2].

Discussion
For practical purposes it is essential to have a limited number of exclusive outcome categories.[6] Accordingly, posttraumatic PVS patients are distinguished from other survivors of severe head injury who are capable of giving a consistently understandable response to those around them either by word or by gesture.[5] The favorable clinical signs are eye-opening, pupillary reactivity, spontaneous eye movement, intact occulovestibular reflexes and motor responses such as localization. Negative signs such as absent eye-opening, non-reactive pupils, absent occulovestibular reflexes and no motor response are prognosticating signs of poor recovery and associated with 85– 91% mortality.[7]
SPECT has proven to be a useful method in demonstrating the distribution of regional cerebral blood flow (rCBF).[89] Oder et al.,observed four patients with good recovery, in whom SPECT was carried out and none of them had global hypoperfusion.[10] In four patients there was only a moderate ventricular dilatation, while one patient showed marked left temporal hypoperfusion. In two patients SPECT showed marked hydrocephalus with one-sided fronto-temporal hypoperfusion, however, the patients had a good recovery. The global reduction of blood flow is reported in PVS patients. Those patients also had decreased metabolic demands of the cerebral cortex, which is termed “apallic”.[11] Gross periventricular and fronto-temporal perfusion defect was noted in four patients with posttraumatic hydrocephalus who remained severely disabled. Seven (47%) patients remained vegetative with global as well as pericontusion perfusion defect. In our study 17 (81%) patients had poor outcome with SPECT abnormalities. Overall, SPECT can predict the outcome better and patients with gross perfusion defect had an unfavorable outcome (P value < 0.0001).
In the past, using two-dimensional xenon flow technique a consistent relationship was reported between reduced mean hemispheric CBF (Cerebral perfusion pressure) and final outcome in severe head injuries.[12] Using PET and SPECT scanning in 16 head injury patients, Baumann et al.,compared the glucose metabolism and perfusion defect in the neocortex and basal ganglia.[13] Facco et al.,compared SPECT and CT findings in the same area in six head injury cases.[14] Six patients with abnormal CT showed no perfusion defect while 12 (50%) patients with severe perfusion defect had no lesion in CT scan.
Though the cold caloric test and MRI are good predictors of outcome of severe head injury in general, when considered with other parameters no statistical significance was noted (P value 0.18 and 0.14 respectively), like in comparison with SPECT.
Prat and Maldonado, in a retrospective study of 160 patients, reported a mortality rate of 50% and 25% patients remained in a persistent vegetative state or were severely disabled.[15] At the end of one year 38 patients (76%) in our study had an unfavorable outcome. In a retrospective study of 134 closed head injury patients who were in coma for longer than one month, Sazbon and Groswasser reported subsequent recovery of consciousness in 54%, mostly during the second and third months.[16] Analysis of the international coma data bank 1373 patients with severe head injury had revealed that 140 were vegetative one month after trauma. Fifty-nine of the vegetative patients (42%) regained consciousness within one year.[17]
Conclusion
Prognosis in vegetative patients is not as poor as believed earlier. Good neurological assessment and meticulous follow-up are necessary in vegetative patients. More than 40% of the vegetative patients improved by the end of one year, of whom 25% had good outcome. SPECT is better than CT/MRI as it assess the cerebral perfusion and functional injury rather than detecting the lesions only. Further study with a control group is necessary to establish the role of SPECT in head injury.
Source of Support: Nil
Conflict of Interest: None declared.
References
- Persistent vegetative state after brain damage: A syndrome in search of a name. Lancet. 1972;1:734-7.
- [Google Scholar]
- BAEP and vestibulooccular reflex in severe head injury: A prospective study. Acta Neurochir. 1987;87:40-3.
- [Google Scholar]
- Persistent vegetative state: An introduction to duty of care issues with reference to a UK cases.A paper given by Dr. Andrew Fergusson. Centre for Bioethics and Public Policy; 2000:1-4.
- [Google Scholar]
- SPECT brain perfusion abnormalities in mild or moderate traumatic brain injury. Clin Nucl Med. 1998;23:309-17.
- [Google Scholar]
- Assessment of outcome after severe brain damage: A practical scale. Lancet. 1975;3:480-4.
- [Google Scholar]
- Severe head injury, clinical assessment and outcome. Physical Ther. 1983;63:1946-51.
- [Google Scholar]
- Technetium99m d, 1 HMPAO: A new radiopharmacuetical for SPECT imaging of regional cerebral perfusion. J Nucl Med. 1987;28:191-202.
- [Google Scholar]
- HMPAO-SPECT in persistent vegetative state after head injury: Prognostic indicator of the likelihood of recovery. Intensive Care Med. 1991;17:149-53.
- [Google Scholar]
- The prognostic value of cerebral blood flow measurement in patients with the apallic syndrome. J Neurol Sci. 1972;16:373-82.
- [Google Scholar]
- Relationship of early cerebral blood flow and metabolism in acute head injury. J Neurosurg. 1990;72:176-82.
- [Google Scholar]
- Persistent vegetative state: Evaluation of brain metabolism and brain perfusion with PET and SPECT. Nucl Med Comm. 2003;24:643-9.
- [Google Scholar]
- Assessment of brain perfusion in coma and comparison between SPECT and CT. Neurol Res. 1998;5:40-3.
- [Google Scholar]
- Prognostic factors in post-traumatic severe diffuse brain injury. Acta Neurochir. 1998;140:1257-61.
- [Google Scholar]
- Outcome in 134 patients with prolonged post-traumatic unawareness: Parameters determining late recovery of consciousness. J Neurosurg. 1990;72:75-80.
- [Google Scholar]
- Vegetative state after closed head injury: A TCDB report. Arch Neurol. 1991;48:580-5.
- [Google Scholar]






