Translate this page into:
Prevalence of fatigue in patients with multiple sclerosis and its effect on the quality of life
Address for correspondence: Dr. Anupam Gupta, Department of Neurological Rehabilitation, National Institute of Mental Health and Neuro Sciences, Bangalore - 560 029, Karnataka, India. E-mail: drgupta159@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This prospective study was carried out to observe the prevalence of fatigue in patients with multiple sclerosis (MS) and its effect on quality-of-life (QoL).
Study Design and Setting:
Prospective observational study in a University Tertiary Research Hospital in India.
Patients and Methods:
A total of 31 patients (25 females) with definite MS according to McDonald's criteria presented in out-patient/admitted in the Department of Neurology (between February 2010 and December 2011) were included in the study. Disease severity was evaluated using the Kurtzke's expanded disability status scale (EDSS). Fatigue was assessed using Krupp's fatigue severity scale (FSS). QoL was assessed by the World Health Organization QoL-BREF questionnaire.
Results:
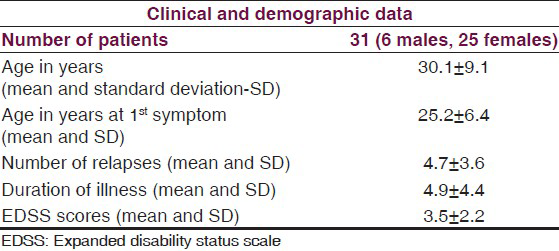
The mean age of patients was 30.1 ± 9.1 years. The mean age at first symptom was 25.23 ± 6.4 years. The mean number of relapses was 4.7 ± 3.6 in the patients. The mean duration of illness was 4.9 ± 4.4 years. The mean EDSS score was 3.5 ± 2.2. Mean fatigue score was 38.7 ± 18.5 (cut-off value 36 in FSS). The prevalence of fatigue in patients with MS was 58.1% (18/31). MS patients with fatigue were significantly more impaired (P < 0.05) on all QoL domains (i.e., physical, psychosocial, social, and environment) than MS patients without fatigue.
Conclusion:
Prevalence of fatigue was found to be high in the MS patients in the study. All four domains of QoL were significantly more impaired in the group with fatigue than in those without fatigue.
Keywords
Fatigue
multiple sclerosis
quality of life
Background
Fatigue is a complex and common symptom present in a wide range of neurological conditions including multiple sclerosis (MS). In fact, it is reported to be one of the three most frequent disabling symptoms in MS with as many as 90% of patients reporting fatigue.[1234] It often severely interferes with patient's work, family, and social life. Clinically, patients with MS report fatigue as exhaustion, lack of energy, increased somnolence or worsening of symptoms and weakness exacerbated by activity and heat (Uthoff phenomenon).[3]
Certain factors such as neurological impairment, spasticity, motor weakness, nocturia, pain, depression, sleep disturbances, and heat sensitivity correlate consistently with fatigue and considered secondary causes of fatigue in MS.[12]
Quality-of-life (QoL) is defined as individual perception of their position in life in the context of the culture and value systems in which they live and in relation to their goals expectations, standards and concerns. Several studies have reported that QoL is worse in patients with MS as compared to healthy controls with a higher prevalence of depression and fatigue.[567891011121314]
Although there is a plethora of literature regarding the effect of MS related fatigue on the QoL in the western countries, but no case series has been published with Indian population of patients with MS as per our knowledge. The objective of this prospective study was to observe the prevalence of fatigue in Indian patients with MS and also to see its effect on various domains of QoL.
Patients and Methods
This prospective observational study was performed with 31 patients with MS (25 females), who visited the out-patient facility or admitted in the Department of Neurology of the University Tertiary Research Hospital between February 2010 and December 2011. Internal ethics committee approval was taken for the study. Informed consent was taken from all patients for participation. Patients with definite MS according to the McDonald's (2005),[15] criteria were included in the study irrespective of age and gender. Patients were excluded from the study if they had an acute relapse in the preceding 2 months, having systemic infection, received pulse methylprednisolone during the past 4 weeks and already receiving medication to reduce fatigue.
All patients who agreed to participate in the study were evaluated with a questionnaire, which included personal data, Kurtzke's expanded disability status scale (EDSS),[16] and Krupp's fatigue severity scale (FSS).[17] History of medication use such as antidepressants, sedatives and anti-hypertensives, which may have contributed to fatigue, was recorded. The QoL was assessed using World Health Organization (WHO) QOL-BREF questionnaire.[18] Patient related information such as filling of proformas, history, and clinical examination of patients was carried out by a Neurologist.
Investigations
Patients underwent a complete hemogram and peripheral smear, random blood sugar, renal and liver function tests, thyroid function tests apart from imaging when necessary. Other medical conditions causing fatigue were ruled out when clinically indicated.
Evaluation of disease severity
Disease severity in patients was evaluated using the Kurtzke's EDSS.[1619] The scale provides a score between 0 (very little disability with a normal neurological examination) to a maximum of 10 (death due to MS). The first levels 1-4.5 refer to people with a high degree of ambulatory ability and the subsequent levels 5-9.5 refer to the loss of ambulatory ability. In addition, it also provides eight subscale measurements called functional system (FS) scores. These systems include pyramidal, cerebellar, brainstem, sensory, bowel and bladder, visual, cerebral, and others. The FS are scored on a scale of 0 (low level of problems) to 5 (high level of problems) to reflect the level of disability observed clinically. The gait and FS scores determine the total EDSS scores.
Evaluation of fatigue
Fatigue severity was assessed using Krupp FSS, which consists of nine items each rated on a seven point scale, which has five equidistant anchor points: Strongly disagree (1), rare (2,3), sometimes (4), frequently (5,6), and strongly agree (7). The score is obtained by computing the average of the nine items with higher scores indicating increasing fatigue severity. Patients having a total FSS score of 36 and above were categorized as having fatigue and those who have a score <36 were categorized as not having fatigue.[17]
Evaluation of QoL
The QoL of patients was assessed using the WHO QOL-BREF questionnaire. This contains a total of 26 questions, which measure the QoL in four domains: Physical health, psychological, environmental, and social relationships. The mean score of items within each domain is used to calculate the domain score. These raw scores are then converted to the final transformed scores on a 0-100 scale.[18]
Statistical analysis
Statistical analysis was performed using the SPSS 15.0 software. Descriptive statistics included frequency, means, and standard deviation for quantitative variables such as age, age at first symptoms, number of episodes, EDSS and FSS scores and duration of illness. All quantitative measures were treated with parametric statistical analysis such as Student's t-test like; FSS, WHO QoL domain scores in patients with MS with and without fatigue. Qualitative measures such as correlation between FSS scores and various domains of WHO QoL were analyzed using Chi-square test.
Results
Study included 31 patients and their clinical and demographic data given in Table 1.
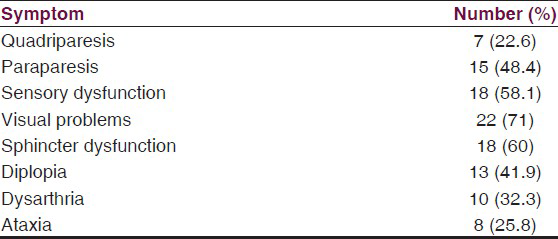
Their clinical presentation has been given in the Table 2.
Profile of fatigue in patients with MS
The mean fatigue score was 38.7 ± 18.5, which is above the cut off value of 36 in the FSS. The prevalence of fatigue in patients with MS was 58.1% (18/31).
Comparison of parameters between patients of MS with and without fatigue
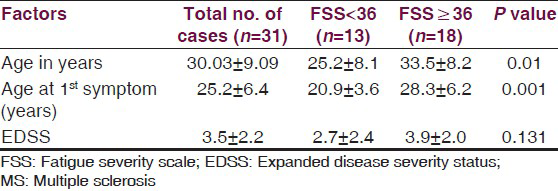
The mean age and age at 1st symptom was significantly greater in the group of MS patients with fatigue as compared to those without fatigue (P = 0.01 and 0.001 respectively) [Table 3].
QoL
All four domains of QoL; physical health, psychological, environmental, and social relationships were significantly more impaired in the group of patients with fatigue than in those without fatigue as mentioned in Table 4.

Discussion
Fatigue is a common symptom in a wide range of clinical conditions. It is one of the key factors that affect the QoL in general. Many factors such as sleep, depression, and disability contribute to fatigue.[5] Very few studies in India have been conducted in patients with MS and these aspects have not been addressed by most of the authors. The aim of this study was to estimate the prevalence of fatigue in patients with MS and its effect on QoL of these patients.
In our study, patients of MS with and without fatigue were compared and it was found that the severity of fatigue correlated with poorer QoL in all domains. The observation highlights the importance of initiating management of fatigue in these patients as it will help not only in improving the symptom, but also will provide a global higher QoL.
Fatigue prevalence was high (58.1%) in our study. Even higher prevalence has been reported in the previous studies with much greater sample size like North American Research Committee on Multiple Sclerosis survey.[4] This survey observed that MS patients with fatigue tended to be older and had more disability according to Patient Determined Disease Scale (PDDS) as compare MS patients without fatigue. However, duration of illness tended to be comparable in the two groups. Respondents with severe fatigue also had significantly higher mobility impairment as measured by PDDS scores compared with respondents with mild/moderate fatigue. Similar significant correlation between fatigue and mobility impairment was reported in another study by Schwartz et al.[20] However, Krupp et al.,[3] found insignificant correlation between EDSS and fatigue scores.
Attempts have been made to identify factors contributing to fatigue in MS. Corpus callosal atrophy,[21] cortical atrophy of the parietal lobe with dysfunctions in higher-order aspects of motor control,[22] regional atrophy of supratentorial brain parenchyma involving the cerebral cortex, nearby white matter and the caudate head areas,[23] significant white matter atrophy in the posterior part of the corpus callosum and significant grey matter atrophy of the left superior frontal sulcus, left pre-central gyrus, posterior cingulate cortex, right thalamus, and left middle frontal gyrus have been some of the structural derangement in the brain found to be correlating with fatigue in MS.[2425]
The causes of primary fatigue in MS include down regulation of gamma-aminobutyric acid activity as a compensatory mechanism due to conduction failure in demyelinated pyramidal tract fibers.[2627] Conduction block,[2829] and activity dependent conduction block are also considered to be the mechanisms responsible for fatigue in MS patients.[30] Cytokine mechanism with increased level of tumor necrosis factor-α levels and interferon-γ levels are found in fatigued MS patients compared to non-fatigued patients and considered to be responsible for fatigue.[31]
These tests were not done or reported in the present study.
In a previous longitudinal study with MS patients, authors examined the symptom cluster of fatigue, pain, and depression as a correlate of reduced QoL. Cluster analysis revealed the presence of three subgroups differing in experiences of the three symptoms. The sub-group with the lowest scores on all three symptoms had the highest QoL, whereas the sub-group with the highest scores on the symptoms had the worst QoL. This observation supports the concept of fatigue, pain and depression as a symptom cluster, which correlates with reduced QoL in patients with MS.[32] Another case-control study in women with relapsing-remitting multiple sclerosis (RRMS) found that pain and pain intensity were significantly more in the RRMS group as compared to controls. However, fatigue and depression intensity was not significantly different between the groups. It was observed that increased fatigue intensity was a predictor for decreased physical QoL in all women, regardless of group.[33]
Ghaem and Borhani Haghighi (2008) in their study found 87.2% of patients with MS had poor sleep. Significant high positive correlation was observed between the quality of mental and physical health composite scores. There was a significant negative correlation between the quality of physical score and age, fatigue score, EDSS score and Pittsburgh Sleep Quality Index (PSQI). Linear regression analysis showed that PSQI score, EDSS, and fatigue score were predictors in the model between the quality of physical score and covariates. Linear regression model showed that fatigue score and PSQI were predictors in the model between the quality of mental score and covariates.[34]
The explanation could be that the three symptoms are often co-occurring and possibly synergistic in persons with MS and are etiologically linked through cytokine induced manifestations of sickness behavior with diffuse axonal damage across different regions of the central nervous system.[313536] Researchers have identified fatigue, depression, and pain as a symptom cluster, which is associated with reduced physical activity and QoL in persons with MS.[3738] Another study reported decreased QoL in all domains with physical functioning being the most affected in patients with MS.[19] The results of this study corroborate the notion that fatigue, increased lower limb tone, poor gait, and greater disability are independent factors that negatively affect the QoL especially physical functioning domain in patients with MS. Fatigue negatively affects both the physical and the mental components of the QoL irrespective of the duration of the disease or the degree of disability.
Conclusions
The prevalence of fatigue was found to be high in patients with MS in the present study. All four domains of QoL; physical health, psychological, environmental, and social relationships were significantly more impaired in the group of patients with fatigue than in those without fatigue. The treatment of fatigue therefore will not only help alleviating fatigue, but also improve QoL of these patients.
Limitations of the study
The study had a relatively small sample size. A follow-up study could have not only thrown light on the impact of fatigue on other co-morbidities, but also effectiveness of treatment in improving QoL and functional abilities of these patients.
Future directions
Fatigue is a symptom with multiple contributory factors such as poor sleep, depression, disability, and autonomic dysfunction. Larger studies will be necessary to find out, which of these abnormalities are the major contributors to fatigue in MS. This may have potential therapeutic implications in the form of early recognition and treatment of these comorbidities. Correlation of fatigue with radiological/imaging abnormalities in these patients can also be attempted.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- The impact of fatigue on patients with multiple sclerosis. Can J Neurol Sci. 1994;21:9-14.
- [Google Scholar]
- North American Research Committee on Multiple Sclerosis. Fatigue characteristics in multiple sclerosis: The North American Research Committee on Multiple Sclerosis (NARCOMS) survey. Health Qual Life Outcomes. 2008;6:100.
- [Google Scholar]
- Fatigue, depression, and health-related quality of life in patients with multiple sclerosis in Isfahan, Iran. Eur J Neurol. 2012;19:431-7.
- [Google Scholar]
- Factors predicting quality of life in a group of Polish subjects with multiple sclerosis: Accounting for functional state, socio-demographic and clinical factors. Clin Neurol Neurosurg. 2012;114:341-6.
- [Google Scholar]
- Quality of life in multiple sclerosis: Measuring the disease effects more broadly. Neurology. 1999;53:1098-103.
- [Google Scholar]
- Quality of life in multiple sclerosis in France, Germany, and the United Kingdom. Cost of Multiple Sclerosis Study Group. J Neurol Neurosurg Psychiatry. 1998;65:460-6.
- [Google Scholar]
- Factors influencing quality of life in multiple sclerosis patients: Disability, depressive mood, fatigue and sleep quality. Acta Neurol Scand. 2004;110:6-13.
- [Google Scholar]
- A study of various scales of fatigue and impact on the quality of life among patients with multiple sclerosis. Rev Neurol. 2000;30:1235-41.
- [Google Scholar]
- Quality of life in multiple sclerosis: The impact of depression, fatigue and disability. Mult Scler. 2001;7:340-4.
- [Google Scholar]
- Fatigue in multiple sclerosis is related to disability, depression and quality of life. J Neurol Sci. 2006;243:39-45.
- [Google Scholar]
- Predicting quality of life in multiple sclerosis: Accounting for physical disability, fatigue, cognition, mood disorder, personality, and behavior change. J Neurol Sci. 2005;231:29-34.
- [Google Scholar]
- Impact of recently diagnosed multiple sclerosis on quality of life, anxiety, depression and distress of patients and partners. Acta Neurol Scand. 2003;108:389-95.
- [Google Scholar]
- Diagnostic criteria for multiple sclerosis: 2005 revisions to the “McDonald Criteria”. Ann Neurol. 2005;58:840-6.
- [Google Scholar]
- Rating neurologic impairment in multiple sclerosis: An expanded disability status scale (EDSS) Neurology. 1983;33:1444-52.
- [Google Scholar]
- The fatigue severity scale. Application to patients with multiple sclerosis and systemic lupus erythematosus. Arch Neurol. 1989;46:1121-3.
- [Google Scholar]
- Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551-8.
- [Google Scholar]
- The effect of functional limitations and fatigue on the quality of life in people with multiple sclerosis. Arq Neuropsiquiatr. 2009;67:812-7.
- [Google Scholar]
- Fatigue and progression of corpus callosum atrophy in multiple sclerosis. J Neurol. 2011;258:2199-205.
- [Google Scholar]
- Relationship of cortical atrophy to fatigue in patients with multiple sclerosis. Arch Neurol. 2010;67:447-53.
- [Google Scholar]
- Regional brain atrophy in primary fatigued patients with multiple sclerosis. Neuroimage. 2010;50:608-15.
- [Google Scholar]
- Voxelwise assessment of the regional distribution of damage in the brains of patients with multiple sclerosis and fatigue. AJNR Am J Neuroradiol. 2011;32:874-9.
- [Google Scholar]
- Basal ganglia and frontal/parietal cortical atrophy is associated with fatigue in relapsing-remitting multiple sclerosis. Mult Scler. 2010;16:1220-8.
- [Google Scholar]
- Motor cortex excitability and fatigue in multiple sclerosis: A transcranial magnetic stimulation study. Mult Scler. 2005;11:316-21.
- [Google Scholar]
- Post-exercise facilitation and depression of motor evoked potentials to transcranial magnetic stimulation: A study in multiple sclerosis. Clin Neurophysiol. 2004;115:2128-33.
- [Google Scholar]
- A quantitative description of membrane currents in rabbit myelinated nerve. J Physiol. 1979;292:149-66.
- [Google Scholar]
- Action potentials and membrane currents in the human node of Ranvier. Pflugers Arch. 1995;430:283-92.
- [Google Scholar]
- The effects of experimental demyelination on conduction in the central nervous system. Brain. 1970;93:583-98.
- [Google Scholar]
- Fatigue in multiple sclerosis: An example of cytokine mediated sickness behaviour? J Neurol Neurosurg Psychiatry. 2006;77:34-9.
- [Google Scholar]
- Symptom cluster and quality of life: Preliminary evidence in multiple sclerosis. J Neurosci Nurs. 2010;42:212-6.
- [Google Scholar]
- The impact of pain and other symptoms on quality of life in women with relapsing-remitting multiple sclerosis. J Neurosci Nurs. 2009;41:322-8.
- [Google Scholar]
- The impact of disability, fatigue and sleep quality on the quality of life in multiple sclerosis. Ann Indian Acad Neurol. 2008;11:236-41.
- [Google Scholar]
- Managing the symptoms of multiple sclerosis: A multimodal approach. Clin Ther. 2006;28:445-60.
- [Google Scholar]
- Donepezil improved memory in multiple sclerosis in a randomized clinical trial. Neurology. 2004;63:1579-85.
- [Google Scholar]
- Effects of change in fatigue and depression on physical activity over time in relapsing-remitting multiple sclerosis. Psychol Health Med. 2011;16:1-11.
- [Google Scholar]
- Health problems and health-related quality of life in people with multiple sclerosis. Clin Rehabil. 2006;20:67-78.
- [Google Scholar]






