Translate this page into:
Emergent management with favorable outcome of an unusual presentation of a primary CNS lymphoma in an immunocompetent patient
Address for correspondence: Dr. Ravi Dadlani, Department of Neurosurgery, Sri Sathya Sai Institute of Higher Medical Sciences, EPIP Area, Whitefield, Bangalore - 560 066, Karnataka, India. E-mail: ravi.dadlani@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Primary CNS lymphomas (PCNSL) are extra-nodal, malignant tumors arising within the brain, eyes, leptomeninges and spinal cord in the absence of systemic involvement at the time of diagnosis.[12] PCNSL is seen in both immunocompromised and immunocompetent patients.[12] PCNSL differs from its systemic counterpart by having a poorer prognosis and demonstrating a angio-centric growth pattern without follicles.[2] In immunocompetent patients most of the PCNSL (90-95%) are B cell lymphomas.[2]
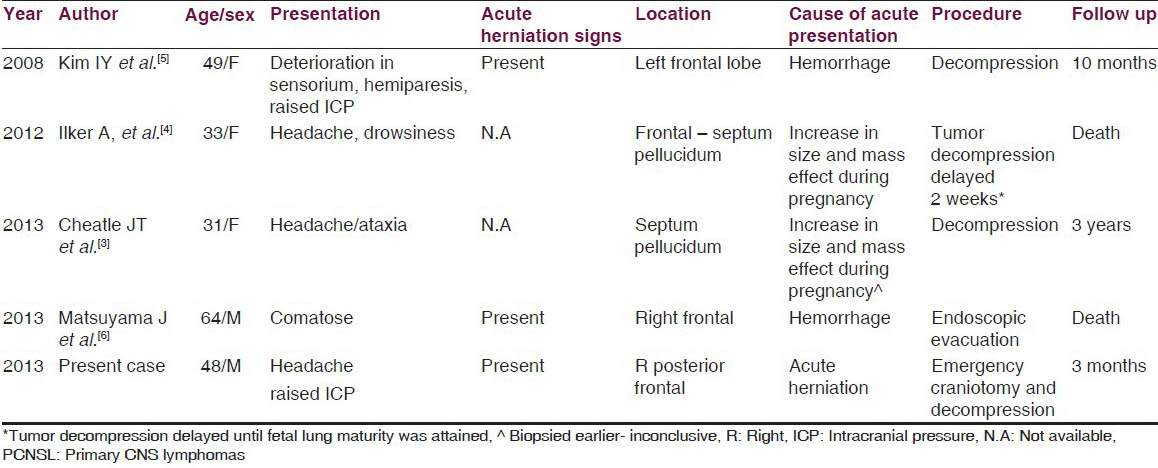
PCNSL occur in decreasing order of frequency in the cerebral hemisphere (38%), basal ganglia and thalamus (16%) corpus callosum (14%), ventricular region (12%), and the cerebellum (9%), demonstrating a proclivity toward the midline peri-ventricular structures.[13] The commonest presenting features are neuropsychiatric.[13] Although features of raised intracranial pressure may be present in as many as 33% (mainly due to hydrocephalus), impending herniation during the presentation is extremely rare and only three such cases have been reported in the literature [Table 1].[12345]
A 48-year-old male patient presented to the emergency room in an altered sensorium of 1 h duration with preceding progressive hemiparesis of six months duration. The neurological examination revealed a deeply comatose patient with a Glasgow Coma score of 7/15 [E1V1M5]. The patient had a dilated right pupil with left hemiparesis of grade 2. MRI of the brain [Figure 1] showed a well-defined lobulated parasagittal lesion.
The patient underwent emergency craniotomy and decompression of the lesion. Intra-operatively the tumor had a poor plane with the brain in some areas. Histopathology clinched the diagnosis of a B cell non-Hodgkin's lymphoma [Figure 2]. Post-operatively the patient improved in sensorium as did his motor power to grade 4. Evaluation for systemic lymphoma was negative. The patient underwent whole brain radiotherapy of 60 Gy and received high dose of methotrexate chemotherapy.
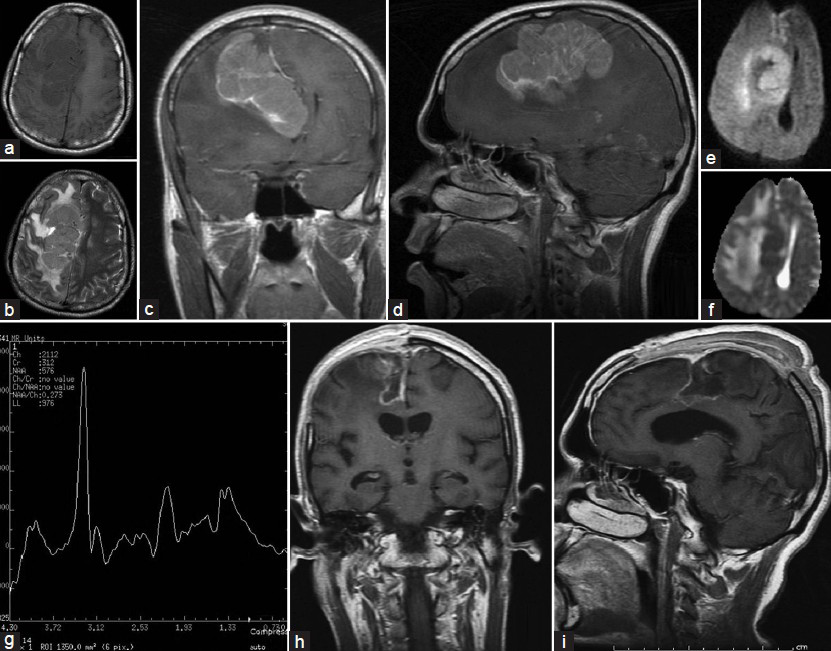
- MRI of the brain revealing a right parasagittal lesion measuring 7.4 × 3.8 × 6.0 cm. It was hypointense on TIW images (a) Hyperintense on T2W images (b) With mass effect and midline shift. Figure 1c and d depict the contrast enhancement on T1W coronal and sagittal images. There was restriction on DWI (e) And hypointensity on ADC. (f) The MR spectroscopy revealed an elevated choline to creatinine ratio and loss of NAA on MRS (g) With surrounding peri-lesional edema with subfalcine/uncal herniation. H and i are post-operative TIW gadolinium images depicting complete excision of lesion
![Paraffin section of non-Hodgkin lymphoma showing monomorphic round to oval cells with hyperchromatic nuclei, mitotic activity and (Inset) immunopositivity for CD20. (H and E ×400) [Inset: Avidin Biotin Complex Immunoperoxidase ×400]](/content/150/2014/5/1/img/JNRP-5-88-g003.png)
- Paraffin section of non-Hodgkin lymphoma showing monomorphic round to oval cells with hyperchromatic nuclei, mitotic activity and (Inset) immunopositivity for CD20. (H and E ×400) [Inset: Avidin Biotin Complex Immunoperoxidase ×400]
Despite advancement in the treatment modalities the prognosis of PCNSL remains poor.[3] Symptomatic therapy results in a median survival of 2-3 months.[12] Steroids decrease the tumor volume by inducing apoptosis in the cells and prolongs the median survival to 4-5 months.[2] The standard of care has been systemic chemotherapy with or without radiotherapy.[12345] Surgery has been traditionally contraindicated in PCNSL due to its diffusely infiltrative nature[12] and has mainly been limited to tissue diagnosis especially in the cases of atypical radiology and partial decompression has no proven benefit over a stereotactic biopsy and has sometimes been associated with a poorer prognosis.[12] There has been one recent review by Weller et al. which challenges this traditional view favoring cytoreductive surgery at least for a subset of patients with PCNSL[7] We have done a review of the literature highlighting the very few instances in which a PCNSL should be operated [Table 1]. In this group of patients, the presentation was due to increased size during the pregnancy in two cases and hemorrhage in two cases.[3456] There have been no cases reported in which the patient had impending herniation due to the size of the tumor, as in the present case.
Despite the criticism associated with surgery in PCNSL, it has a significant and special role in the case of rare emergency presentation and may have a favorable outcome such as in the present case.
References
- Primary CNS lymphoma: Clinical presentation, pathological classification, molecular pathogenesis and treatment. J Neurol Sci. 2000;181:1-12.
- [Google Scholar]
- Atypical presentation of primary central nervous system non-Hodgkin lymphoma in immunocompetent young adults. World Neurosurg. 2013;79:593.e9-13.
- [Google Scholar]
- Primary central nervous system lymphoma presenting as an acute massive intracerebral hemorrhage: Case report with immunohistochemical study. Surg Neurol. 2008;70:308-11.
- [Google Scholar]
- Primary CNS lymphoma arising in the region of the optic nerve presenting as loss of vision: 2 case reports, including a patient with a massive intracerebral hemorrhage. Brain Tumor Pathol 2013
- [Google Scholar]
- Surgery for primary CNS lymphoma? Challenging a paradigm. Neuro Oncol. 2012;14:1481-4.
- [Google Scholar]





