Translate this page into:
Isolated nuclear III nerve paresis secondary to neurocysticercosis showing spontaneous clinical improvement
Address for correspondence: Dr. Sunil Chauhan, Department of Ophthalmology, Indira Gandhi Medical College, Shimla, Himachal Pradesh, India. E-mail: skc041080@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We wish to present a case of isolated nuclear IIIrd nerve paresis secondary to neurocysticercosis (NCC) showing spontaneous clinical improvement. Isolated third cranial nerve palsy is rare in NCC. A 14-year-old male child of Nepali origin presented with diplopia for 6 days in left lateral gaze and drooping of his upper eyelids in both eyes. The complaints were insidious in onset, non-progressive simultaneous in both eyes with no diurnal fluctuation. Rest of his present and past medical history was not significant. He had history of pork consumption. His general physical examination and systemic examination including neurological examination was unremarkable.
His visual acuity was 6/6 OU with increased wrinkling on forehead. He had severe neurological ptosis in both eyes with poor levator palpebrae superioris (LPS) action with no Marcus Gunn phenomenon and no sign s/o fatigueability. He also had an exotropia of about 15 degree and mild paresis of elevation of eyeball in right eye maximum in lateral gaze. He had mild paresis of his right medial rectus with end gaze nystagmus in left gaze. Rest of the ophthalmological examination was unremarkable including papillary reactions. Diplopia charting showed horizontal diplopia in all gaze positions with maximum difference in left lateral gaze positions [Figure 1]. While waiting for his investigation reports his sign and symptoms showed spontaneous clinical improvement. His magnetic resonance imaging (MRI) showed a solitary ring-enhancing lesion in the pre-aqueductal region of mid brain of size 0.72 × 0.68 cm involving IIIrd nerve nucleus with peri lesional edema [Figure 2]. His lumbar puncture was done and it revealed CSF protein levels 60 and it also showed 9 white blood cells mainly lymphocytes. ADA levels in his CSF were within normal limit. His serology revealed positive IgG levels for taenia solium (1.13 U/ml) by ELISA. In the light of the above findings the patient was diagnosed as a case of nuclear third nerve paresis secondary to NCC of brainstem. After consultation with Department of Neurology the patient was put on oral albendazole and prednisolone. He was continuously followed up with no similar episodes till 1 year after.

- (a) Ptosis in both eyes. (b) Paresis of Medial rectus in right eye. (c) Paresis of elevation in right eye. (d-f) Respective improvement
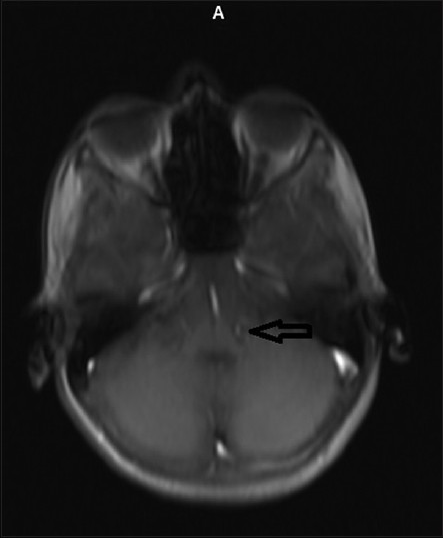
- Transverse section in MRI showing solitary ring enhancing lesion in the pre-aqueductal region of mid brain of size 0.72 × 0.68 cm involving IIIrd nerve nucleus with peri lesional edema
NCC is the most common parasitic infestation of the nervous system.[1] Globally, NCC is endemic in Central and South America, sub-Saharan Africa, and in some regions of the Far East, including the Indian subcontinent, Indonesia, and China, reaching an incidence of 3.6% in some regions.[1] Del Brutto et al. have suggested diagnostic criteria for NCC.[2] In our case these criteria were fulfilled for probable diagnosis of NCC. It usually presents with seizures. Other various CNS clinical manifestations include headache, hydrocephalus, chronic meningitis, focal neurological deficits, dementia and psychiatric manifestations.[3] Involvement of third nerve is rare especially due to a parenchymal lesion.[4] Fluctuation in perilesional edema was probably responsible for spontaneous clinical recovery in our patient. The lesion in such nuclear third nerve paresis involves the central caudal nucleus (CCN), which is a small subgroup of oculomotor nucleus containing subnucleus for levator palpebrae superioris.[5] Involvement of this nucleus results in complete, bilateral ptosis.
We propose a more detailed evaluation of patients with fluctuating ptosis. In those patients where ptosis is restricted to ocular muscle without any other neuromuscular involvement, cranial imaging needs to be done, preferably MRI of the brain with contrast studies that may show lesions in the midbrain.
References
- Neurocysticercosis. Available from: http://www.emedicine.medscape.com/article/1168656-overview
- [Google Scholar]
- Neurocysticercosis presenting as midbrain syndrome. J Assoc Physicians India. 2000;48:533-5.
- [Google Scholar]





