Translate this page into:
The first case of Nocardia beijingensis isolated infection to lumbar spine
Address for correspondence: Dr. Stefano Rigotti, Department Orthopaedic and Traumatology, S. Cuore-Don Calabria Hospital, Negrar, Italy. E-mail: stefano.rigotti@sacrocuore.it
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
We report a case of isolated lumbar spine infection in an immunocompetent patient caused by Nocardia beijingensis, a recently identified Nocardia isolated from soil in Beijing in 2001. Osteoarticular foci are uncommon and among them, spinal infection is exceedingly rare.
In July 2013, we treated a immunocompetent patient of 75-year-old suffering persistent fever from 10 weeks, abdominal pain, constipation, and low back pain on the right side. Routine laboratory studies results revealed moderate neutrophilia, slight anemia and lymphocytopenia, high C-reactive protein levels. Chest radiograph, urine, and blood culture were negative. Positron emission tomography-computed tomography scan [Figure 1] showed an isolated reactive zone on the right paravertebral side of L3-L4-L5. An ultrasound-guided biopsy was performed, but microbiological analysis on the collected samples resulted negative. Open biopsy was then performed according to Cottle et al.[1] It was present an important subfascial abscess extended from L3 to L5 on the right side, deep to L4 lamina. Pus and affected tissue were removed and an extensive debridement of surrounding tissues was performed. Microbiological analysis was performed on tissue samples. Cultures were incubated aerobically at 35°C for 3 weeks. All whitish gipsy and wet hay-smelling colonies yielded on blood agar were stained by the partial acid-fast method according to Kinyoun technique modified for nocardioforms. Identification of the strain suspected to belong to Actinomycetales was based on the capacity to clear casein, xanthine, hypoxanthine, tyrosine, adenine, uric acid, and esculin (Biorad, France) and to be resistant to lysozyme and to 5-fluorouracil, and on the enzymatic activities (arylsulfatase, butyrate esterase, caprylate esterase, catalase, chymotrypsine, cystine arylamidase, a-fucosidase, a-and b-galactosidases, N-acetil-b-glucosaminidase, a-and b-line glucosidases, b-glucuronidase, leucine arylamidase, a-mannosidase, myristate lipase, nitrate reductase, acid and alkaline phosphatases, phosphohydrolase, valine arylamidase, and trypsine). Identification was completed by the evaluation of the presence of urease after growth on Christensen urea agar and incubation at 25°C for 3 weeks. Additional tests were performed to evaluate the acid production from mannitol and sorbitol after 4 weeks incubation at 35°C. Minimal inhibitory concentrations’ testing was performed by the Epsilometer (E-test, bioMérieux) testing: Amikacin, amoxicillin plus clavulanic acid, ceftriaxone, cefepime, ciprofloxacin, clarithromycin, gentamicin, imipenem, linezolid, tobramycin, trimethoprim plus sulfonamide. Susceptibility testing was performed on Mueller Hinton Agar (bioMérieux). The results were read after 24 h of incubation at 37°C. Susceptibility testing was revised and interpreted according to Clinical and Laboratory Standards Institute criteria.
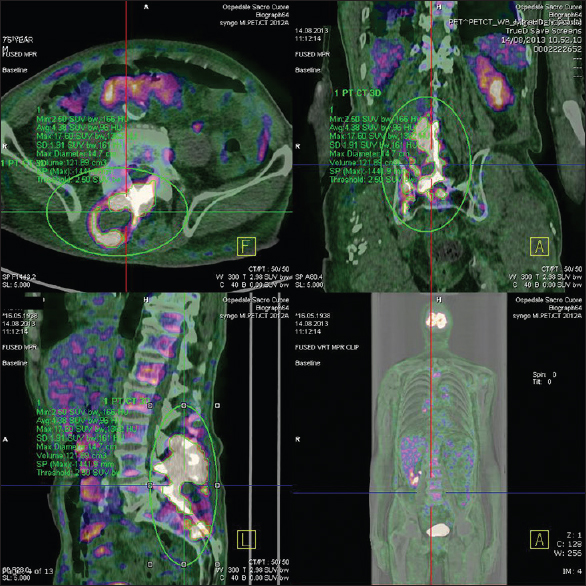
- Positron emission tomography-computed tomography scan showed an isolated reactive zone on the right paravertebral side of L3-L4-L5
Finally, genotypical identification has been performed by amplification and sequencing of a DNA fragment coding rRNA 16S according with the manufacturer's (Applied Biosystem) suggestions. Sequences have been compared with the reference ones present in the GenBank (National Center for Biotechnology) database by the Basic Local Alignment Search Tool program. The sequence has been deposited in the GenBank (accession number: AB094648.1). Sequences producing significant alignments permitted to identify the strains with 100% value of identity with the reference strain. Final identification was Nocardia beijingensis. After surgery, the patient started broad spectrum antibiotic therapy with regression of fever. Once the pathogen was identified, specific antibiotic therapy with imipenem, and amikacin was administered for 3 weeks according to susceptibility test results. Patient experienced a rapid clinical improvement and progressive regression of low back pain. After that, cotrimoxazole was administered for 3 months. Laboratory tests became normal 4 weeks after starting antibiotic therapy. Ultrasound examination and blood tests were performed every 3 months. Complete recovery and absence of lumbar abscess at ultrasound was obtained after 12 months.
Nocardiosis beijingensis isolated infection are extremely rare, as described by Crozier et al.[2] Chatelus et al.[3] confirm that the spinal infections are rare and that thoracic and cervical spine localizations are predominant. The high morbidity and mortality rates of nocardiosis indicate a need for an early diagnosis, but it is often very difficult to isolate the pathogen: Blood cultures are usually negative and local specimens must therefore be obtained. In this case, as in that described by Chatelus et al., a vertebral biopsy was useless in the pathogen identification.[4] The choice of therapy should be guided by susceptibility testing. Treatment with a combination of antibiotics is necessary to avoid both the recurrence of infection and drug resistance.[5] This patient was successfully treated with a combination of imipenem and amikacin, followed by oral cotrimoxazole based on antibiotic susceptibility testing. Concluding, we first report a case of isolated subfascial lumbar spine infection caused by Nocardia beijingensin in an immunocompetent host. Once isolated the pathogen, in agreement with other authors,[46] it is convenient to perform surgical debridement and specific antibiotic therapy.[3456]
References
- First report of Nocardia beijingensis infection in an immunocompetent host in the United States. J Clin Microbiol. 2014;52:2730-2.
- [Google Scholar]
- Nocardia species infections in a large county hospital in Miami: 6 years experience. J Infect. 2007;54:358-61.
- [Google Scholar]
- First case of Nocardia nova spinal abscess in an immunocompetent patient. Braz J Infect Dis. 2012;16:196-9.
- [Google Scholar]





