Translate this page into:
Isolated intermittent vertigo: A presenting feature of persistent trigeminal artery
Address for correspondence: Dr. Khurshid Khan, 2E3 WC Mackenzie Health Science Center, Edmonton, Alberta T6G 2R7, Canada. E-mail: khurshid.khan@ualberta.ca
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Embryonic carotid – basilar anastomosis when persistent in adult life can present with a variety of neurological symptoms. We present a patient with isolated intermittent vertigo attributable to the embryonic anastomosis and describe the different types of persistent trigeminal artery. A 76-year-old Caucasian man presented with isolated intermittent vertigo and symptoms suggestive of anterior and posterior circulation strokes. Impaired vasomotor reactivity was demonstrated on insonation of the anterior and posterior cerebral arteries in this patient with a persistent left trigeminal artery and 75% stenosis of the left internal carotid artery (ICA). The symptom of intermittent vertigo resolved with carotid endarterectomy. Decreased flow across the stenotic segment of the ICA which subserved the posterior circulation resulted in basilar insufficiency. Hypoperfusion to the flocculonodular lobe supplied by the anterior inferior cerebellar artery is a likely cause for the intermittent vertigo.
Keywords
Hypoperfusion
isolated vertigo
persistent trigeminal artery
Introduction
A number of embryonic vascular channels connect the developing internal carotid artery (ICA) and the paired longitudinal neural arteries. The embryonic anastomoses primarily serve to feed the paired longitudinal arteries in early embryonic life. The trigeminal artery is the most cephalad of them and is the last to regress. By 7–14 mm embryonic stage, all the embryonic anastomosis disappears and the cervical inter-segmental arteries act to feed the developing basilar artery.[12] Though not common, knowledge of these embryonic vessels plays an important role in understanding the mechanisms underlying the various neurological presentations when they persist in adult life.
Case Report
A 76-year-old Caucasian male presented with a history of intermittent dizziness. His initial symptom of intermittent short lasting spinning sensation started 6 weeks prior to admission. The vertigo was not positional and not associated with diplopia, dysarthria, or hearing loss. He later experienced word finding difficulty, unsteadiness on his feet and incoordination of the right arm, and blurred vision that affected the right side of his visual field for 3-, 2-, and 1-week prior to admission, respectively. Intermittent vertigo occurred independent of his other symptoms. He is an ex-smoker (7.5 pack years) and took rosuvastatin for dyslipidemia.
On examination, he had mild dysmetria and intentional tremor affecting the right arm, tandem gait ataxia, and right-sided hemianopia. The Dix-Halpike maneuver and head impulse test were negative.
The magnetic resonance imaging of the brain revealed acute diffusion-weighted imaging (DWI) restricted lesion in the external border-zone territory between the middle cerebral artery (MCA) and posterior cerebral artery (PCA), as well as internal border-zone infarct, between the perforators and the cortical branches of the MCA. In addition, there was a cortical prefrontal gyrus DWI restricted lesion. There was 75% narrowing at the origin of the ICA along with a persistent trigeminal artery (PTA) on the left. Computed tomography angiography [Figure 1]. The basilar artery below the level of the trigeminal artery was hypoplastic, and the posterior communicating artery (PCoA) was absent.
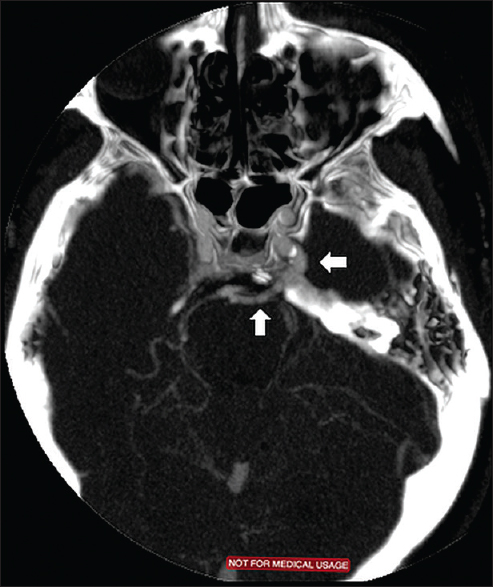
- Persistent trigeminal artery on computed tomography angiogram
Transcranial Doppler insonation of the left MCA and left PCA revealed impaired vasomotor reactivity (VMR) on breath holding. The breath holding index was 0.35 and − 0.25 on insonating the left MCA and PCA, respectively [Figure 2]. Furthermore, the microembolic signal was identified on insonating the left MCA. The symptom of intermittent vertigo resolved with carotid endarterectomy and has not recurred.
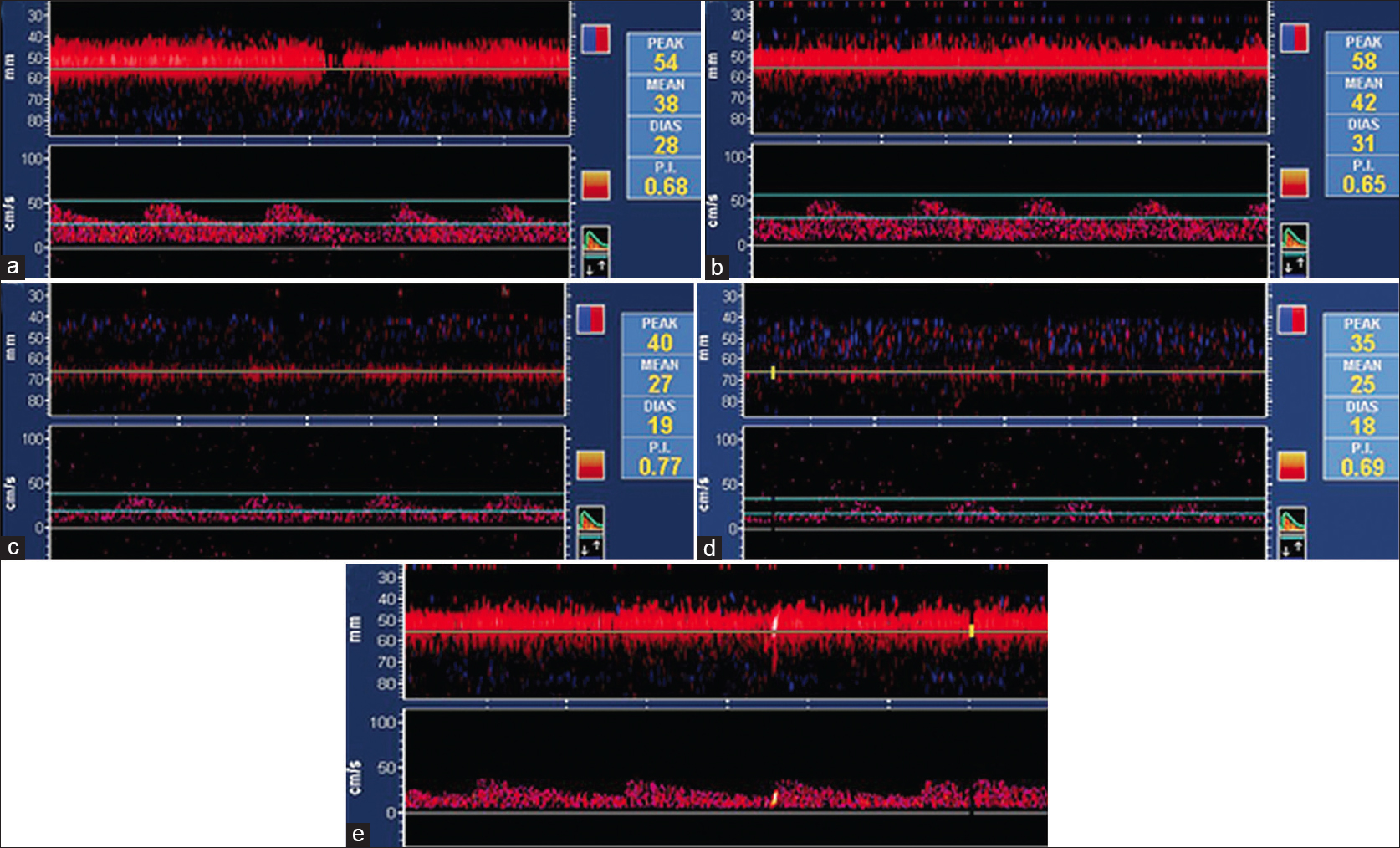
- TCD findings on insonation of Left MCA and PCA. (a) Left MCA (baseline) (MFV: 38). (b) Left MCA (end of breath holding) (MFV: 42). (c) Left PCA (baseline) (MFV: 27). (d) Left PCA (end of breath holding) (MFV: 25). (e) MES left MCA. TCD: Transcranial Doppler, MCA: Middle cerebral artery, PCA: Posterior cerebral artery, MES: Microembolic signal, MFV: Mean flow velocity
Discussion
The PTA was initially described by Quain in 1844 in an autopsy case. Later, Sutton demonstrated PTA angiographically in 1950.[12] The incidence of PTA varies between 0.1% and 0.6%.[1] It is the most cephalad of the embryonic carotid – basilar anastomosis. The PTA originates from the ICA at the proximal part of the cavernous segment. It can take either a lateral (petrosal type) or a medial (sphenoidal type) course to reach the posterior fossa.[23] The PTA joins the basilar artery between the superior cerebellar and the anterior inferior cerebellar arteries (AICAs). In Saltzman type I anastomosis, the BA proximal to the PTA and the PCoA are hypoplastic.[234] The PTA supplies the upper basilar, superior, and AICA and PCA territories. Conversely, in Saltzman type 2 anastomoses, the PCoA takes over the supply of the PCA territory. The vertebrobasilar system is not hypoplastic, and the posterior fossa structures are supplied by both the PTA and the vertebrobasilar system. In the variant type, PTA supplies one of the ipsilateral cerebellar arteries. Our patient had a Saltzman type 1 PTA.
Posterior circulation stroke due to various etiologies in the context of PTA have been reported in literature and include the following: (a) Cardioembolic occlusion of PTA, (b) ICA dissection, and (c) Large artery atheroembolism.[4567] Though there have been reports of basilar insufficiency (BI) in patients with PTA and carotid disease, isolated vertigo resulting from impaired VMR has not been objectively demonstrated.[8]
Our patient had symptoms of isolated intermittent vertigo, and discrete occurrences suggestive of anterior and posterior circulation ischemic strokes. It is important to note that the symptoms of isolated intermittent vertigo preceded his stroke symptoms by 3 weeks. On imaging, the distribution of strokes in the anterior circulation was in the border-zone territory and frontal cortex suggestive of both a hemodynamic and embolic phenomenon, respectively. Though there was no diffusion restriction, there was a strong clinical suggestion on history and examination that the patient had a posterior circulation stroke.[11] The intermittent vertigo was short, and there were no signs to indicate a peripheral cause for his vertigo. Intermittent vertigo resolved completely with carotid endarterectomy.
Although, the etiology of isolated vertigo is usually peripheral in origin, ischemia involving the flocculonodular lobe supplied by the AICA can present with a similar picture.[1112] In our patient, the AICA territory is supplied by flow in the PTA. We hypothesize that a preferential involvement of AICA territory due to the following: (a) Altered flow dynamics in the PTA and basilar, (b) Hypoplastic basilar prior to origin of AICA and flow subserved by the PTA, and (c) Probable atheromatous AICA origin ostial stenosis. The intermittent symptoms can be explained by hypoperfusion from BI.
To our knowledge, this is the first case wherein we demonstrated the following: (a) Impaired VMR on insonation of the MCA and PCA on the side of the persistent trigeminal artery, (b) Microembolic signal in the MCA, (c) anterior and posterior circulation strokes, and (d) Isolated vertigo secondary to a hemodynamic phenomenon which resolved with endarterectomy.
Conclusion
Knowledge of the embryonic carotid basilar anastomoses is important to understand uncommon manifestations of the cerebrovascular disease. Isolated intermittent vertigo in most instances is due to a peripheral cause. However, it can rarely be the presenting manifestation of a central cause. Hypoperfusion to the flocculonodular lobe subserved by the AICA is a likely cause for the isolated intermittent vertigo in this patient.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The Anatomy of the Arteries of the Human Body and Its Applications to Pathology and Operative Surgery. London: Taylor and Walton; 1844. p. :550.
- [Google Scholar]
- The persistent trigeminal artery: Development, imaging anatomy, variants, and associated vascular pathologies. Neuroradiology. 2013;55:5-16.
- [Google Scholar]
- Anatomical features and clinical relevance of a persistent trigeminal artery. Surg Neurol Int. 2012;3:111.
- [Google Scholar]
- Normal and abnormal embryology and development of the intracranial vascular system. Neurosurg Clin N Am. 2010;21:399-426.
- [Google Scholar]
- Brainstem infarction secondary to persistent trigeminal artery occlusion: Successful treatment with intravenous rt-PA. Eur Neurol. 2010;64:311.
- [Google Scholar]
- Brainstem infarction in a patient with internal carotid dissection and persistent trigeminal artery: A case report. BMC Med Imaging. 2010;10:14.
- [Google Scholar]
- Bilateral occipital infarctions associated with carotid stenosis in a patient with persistent trigeminal artery.The Collaborators of the North American Carotid Endarterectomy Trial (NASCET) Stroke. 1994;25:1520-3.
- [Google Scholar]
- Vertebrobasilar insufficiency in a patient with persistent trigeminal artery and stenosis of the ipsilateral carotid bifurcation – case report. Neurol Med Chir (Tokyo). 1988;28:584-7.
- [Google Scholar]
- Persistent trigeminal artery (carotid-basilar anastomosis) J Neurosurg. 1964;21:199-206.
- [Google Scholar]
- VISION Study Group. When to expect negative diffusion-weighted images in stroke and transient ischemic attack. Stroke. 2008;39:1898-900.
- [Google Scholar]
- Recent advances in central acute vestibular syndrome of a vascular cause. J Neurol Sci. 2012;321:17-22.
- [Google Scholar]






