Translate this page into:
Dorsal spinal epidural psammomatous meningioma in an adult male
Address for correspondence: Dr. Sharad Pandey, Department of Neuro Surgery, Sir Sunderlal Hospital, Institute of Medical Science, Banaras Hindu University, Varanasi - 221 005, Uttar Pradesh, India. E-mail: drsharad23@yahoo.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Meningiomas are benign in nature and arise from the arachnoid cells. They are mostly situated in the intracranial compartment, whereas spinal meningiomas are rare. Approximately, in 10% of cases, an extradural component is seen but an exclusively extradural meningioma is quite uncommon. However, WHO Grade II (atypical) and Grade III (anaplastic) tumors can behave aggressively. We reported a case of purely extradural psammomatous meningioma in an adult male affecting the dorsal spine although uncommon meningiomas should be included in the differential diagnosis of extradural intraspinal masses.
Keywords
Dorsal spine
extradural
intraspinal
psammomatous meningioma
Introduction
Approximately, 1.2% of all meningiomas of the central nervous system affect the spine, being relatively rare compared to those in the intracranial compartment. Further, isolated extradural spinal meningiomas are exceedingly rare.[12] Thus are seldom considered in the differential diagnosis of spinal extradural lesions.[3] We are reporting a case of purely extradural psammomatous meningioma affecting the dorsal spine. It is important to emphasize that to reach the definitive diagnosis of extra-axial soft tissue lesions and properly manage the patient, histopathological examination, and frozen section biopsy are required.
Case Report
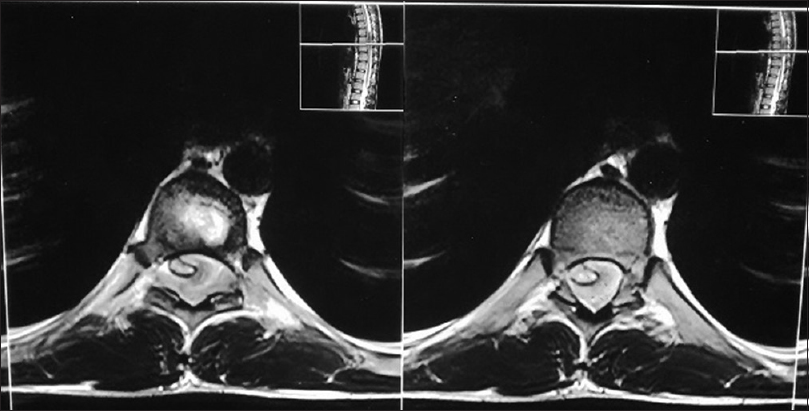
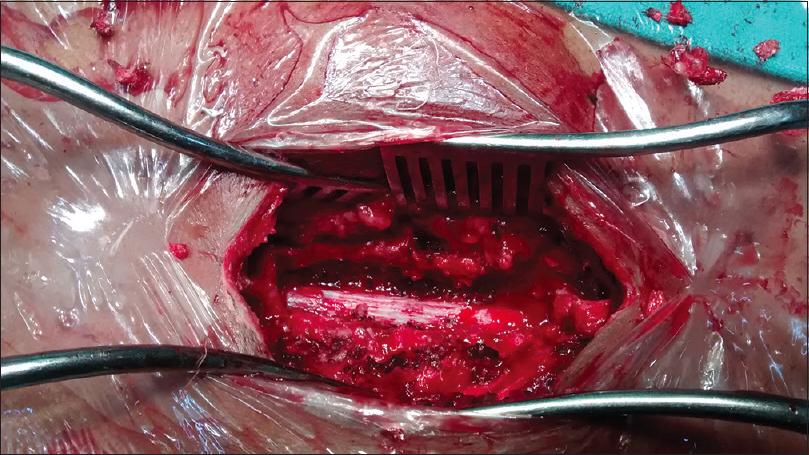
An 18-year-old adult male presented at the Neurosurgery Outpatient Department with chief complaints of gradually progressing weakness and diminished sensation in both the lower limbs of 1 year duration. Ten months later, he started experiencing constipation and urinary incontinence. These complaints were preceded by pain in the dorsal spine. His lower limb weakness progressed, and he became bed ridden. There was no history of fever, trauma, or any chronic illness. On physical examination, spastic paraplegia and loss of all sensory modalities below the D7 dermatome were found. On gadolinium enhanced magnetic resonance imaging of the dorsal spine, an extradural spinal lesion extending from midbody of D7 to midbody of D9 vertebra [Figure 1], which was hypointense on T1 and T2 [Figure 2] with homogenous enhancement with contrast was seen posterior and lateral to the spinal cord compressing the dura anteriorly, and extending to the left D8–D9 neural foramina, thus with features suggestive of either neurofibroma or meningioma [Figure 3]. The patient was planned for elective surgery and underwent D7–D9 laminectomy and total excision of the lesion. Intraoperatively, it was a vascular lesion which was adherent to the dura mater [Figure 4]. Histopathological examination reported features suggestive of psammomatous meningioma [Figure 5]. The patient improved in the postoperative period and regained Grade 5/5 power in both lower limbs, sensations, and bowel and bladder function improved at 6 months follow-up.

- MRI of the dorsal spine, an extradural spinal lesion extending from midbody of D7 to midbody of D9 vertebra (plane and contrast)
- MRI of the dorsal spine, showing an extradural spinal lesion hypointense on T1 and T2 images
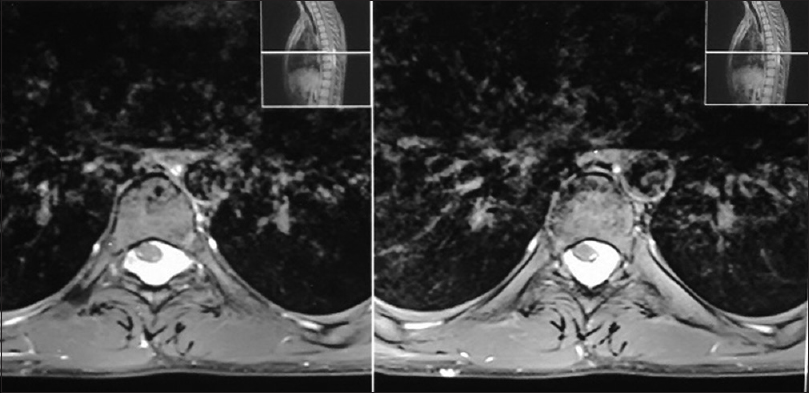
- MRI of the dorsal spine, showing an extradural spinal lesion with homogenous enhancement with contrast
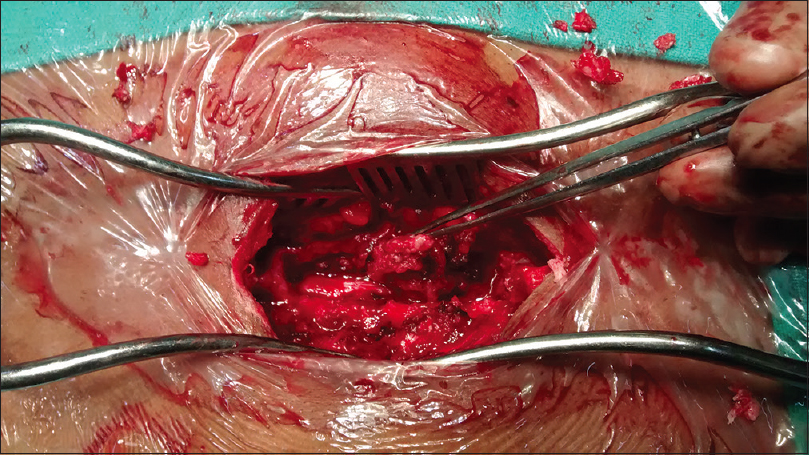
- Intraoperative photograph showing a vascular lesion adherent to the dura mater
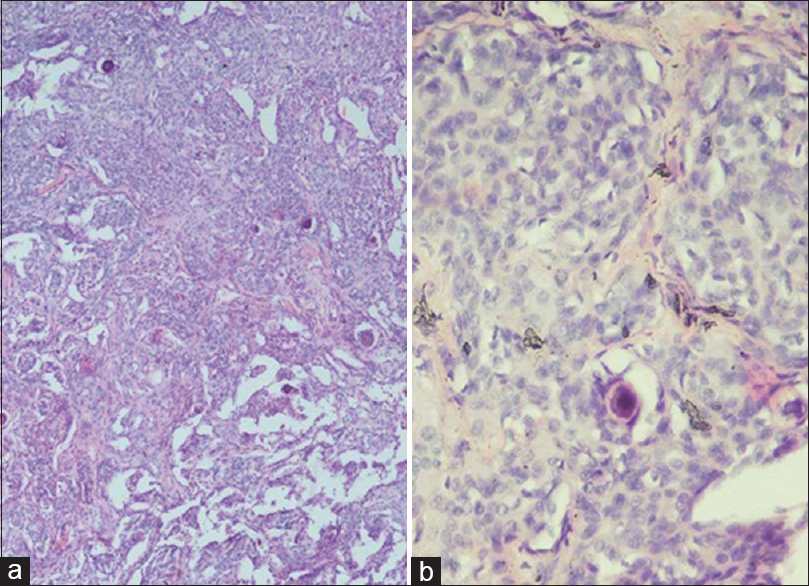
- (a) Histopathological examination showing sheets of meningothelial cells showing whirling pattern focally (×40). (b) Magnified view of tumour showing syncytial sheets of meningothelial cells, with psammoma bodies on HPE (×200)
Discussion
Meningiomas are benign in nature and arise from the arachnoid cells. They are mostly situated in the intracranial compartment, whereas spinal meningiomas are rare. Spinal meningiomas comprise approximately 1.2% of all the meningiomas and 25% of all the spinal cord tumors.[45] These tumors show female predominance with a male: female ratio of 1:9, with no sex predilection in children.[6] Approximately, in 10% of cases, an extradural component is seen but an exclusively extradural meningioma is quite uncommon.[3]
These tumors are attributed to the presence of ectopic or separated arachnoid tissue around the periradicular nerve root sleeve, where the spinal leptomeninges merge directly into the dura mater.[3]
It is pertinent to be aware of the fact that totally extradural spinal meningiomas, especially the “en plaque” variety may mimic metastatic disease.[7] This can be ruled out by an intraoperative histology, i.e., frozen section histopathology, which is a must for optimal surgical decision-making. In this case, intraoperative frozen section enabled us to correctly identify the pathology and perform the near-total resection. After the intraoperative diagnosis of meningioma is confirmed for an extradural spinal lesion, gross total resection of the tumor including extensions into the bone or the paraspinal space should be conducted. This approach is likely to give the best results since the prognosis of this tumor depends on the extent of resection.[7]
Intraoperatively, we were able to strip off the tumor from the spinal dura, without excising the dura to expose the shining white dura underneath [Figure 6], as these extradural spinal meningiomas arise from the dural root sleeve and not from the external surface of the spinal dura. Most meningiomas are benign, well-circumscribed, slow growing tumors, and behave mostly according to the pathological (WHO) grading and usually follow an uneventful clinical course. However, the WHO Grade II (atypical) and Grade III (anaplastic) tumors can behave aggressively clinically and histologically.[8] Bony involvement and paraspinal extent are responsible for the worse prognoses due to difficult removal.[7]
- Intraoperativel photograph showing, shining-white dura after striping off the tumor
To conclude, meningiomas should be included in the differential diagnosis of extradural intraspinal masses. Intraoperative pathological examination helps in further management. Although benign, but it is necessary to conduct long-term clinical and radiological follow-up to diagnose recurrence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Review of 36 cases of spinal cord meningioma. Spine (Phila Pa 1976). 2000;25:727-31.
- [Google Scholar]
- Concurrent intradural and extradural meningiomas of the cervical spine. Neurosurgery. 1990;27:629-31.
- [Google Scholar]
- Purely epidural spinal meningioma mimicking metastatic tumor: Case report and review of the literature. Spine (Phila Pa 1976). 2002;27:E403-5.
- [Google Scholar]
- Cervical extradural meningioma: Case report and literature review. J Spinal Cord Med. 2008;31:302-5.
- [Google Scholar]
- Preoperative radiologic classification of convexity meningioma to predict the survival and aggressive meningioma behavior. PLoS One. 2015;10:e0118908.
- [Google Scholar]






