Translate this page into:
Evaluation of low back pain with low field open magnetic resonance imaging scanner in rural hospital of Southern India
Address for correspondence: Asst. Prof. Sadhanandham Shrinuvasan, Sri Lakshmi Narayana Institute of Medical Sciences (Affiliated to Bharath University), Osudu, Puducherry, India. E-mail: drshrinuvas@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Low back pain (LBP) is the most common symptom which is associated with limitation of normal activities and work-related disability. Imaging techniques are often essential in making the correct diagnosis for prompt management. Plain Radiography though remain a first imaging modality, magnetic resonance imaging (MRI) due to its inherent softtissue contrast resolution and lack of ionizing radiation remains invaluable modality in the evaluation of LBP.
Aim:
To find the common causes of LBP in different age groups and the role of MRI in detecting the spectrum of various pathological findings.
Materials and Methods:
This is a prospective study done in the Department of Radiodiagnosis during a period of 2 years from July 2013 to July 2015. The study population includes all the cases referred to our department with complaints of LBP. Patients with ferromagnetic metallic implants and uncooperative cases were excluded. HITACHI 0.4 Tesla open MRI machine was used for imaging.
Results and Conclusion:
This study involved a total of 235 cases. There were 121 males and 114 females. The age of the patient ranged from 21 to 68 years with an average of 41.3 years. Back pain was commonly observed in the third to fifth decade. The common causes for back pain are disc herniations (disc bulge – 35.3%, disc protrusion – 39.6%, disc extrusion – 7.2%) accounting to 82.1%, followed by normal study (10.2%), vertebral collapse (traumatic – 2.1%, osteoporotic – 1.7%), infections (2.1%), and neoplasm (1.7%). MRI provides valuable information regarding the underlying causes of LBP, especially in disc and marrow pathology.
Keywords
Back pain
herniated disk
lumbar magnetic resonance imaging
spondylolisthesis
vertebral collapse
Introduction
Low back pain (LBP) is a common problem involving the spine and back muscles. LBP may be classified into acute (0–6 weeks), subacute (6–12 weeks), and chronic (>12 weeks) based on the duration of disease. The lifetime prevalence of LBP has been reported to be 70–85%.[1] Acute LBP is one of the most common conditions encountered in primary care. When acute back pain is associated with neurologic symptoms, then an extensive workup is warranted to look for causes such as herniated intervertebral disk, spinal stenosis, and cauda equine syndrome, which accounts for only 5% of acute back pain cases.[2] The most commonly used imaging modalities are X-ray, magnetic resonance imaging (MRI), computed tomography, and nuclear medicine bone scan. It is important to keep in mind the limitations of the diagnostic studies and to consider how the management will be influenced by the information obtained from these studies. MRI plays a vital role in back pain associated with radiculopathy or spinal stenosis and back pain associated with progressive neurologic deficits. However, because of the lesser radiation exposure and better delineation of soft tissue surrounding the vertebrae, it has become one of the preferred imaging modality in the evaluation of back pain.
Materials and Methods
This is a prospective study done in the Department of Radiodiagnosis during a period of 2 years between July 2013 and July 2015. The study population included all the patients referred to our department for MRI lumbar spine with complaints of LBP. Those with ferromagnetic metallic implants and uncooperative cases were excluded from the study.
Imaging and image analysis
All patients referred to the Department of Radiology for MRI lumbar spine underwent MRI examinations as per protocols. The routine protocol included was sagittal and axial T1- and T2-weighted images and short tau inversion recovery (STIR) coronal images. Special sequences such as myelogram, gadolinium-enhanced T1-weighted images were also done whenever needed. All MRI examinations were performed on a 0.4 Tesla HITACHI open MRI scanner. All images were reviewed at an electronic PACS workstation by radiologists, and a consensus diagnosis was given by two radiologists in controversial cases. All lumbar levels and in some cases to look for multi-vertebral involvement, whole spine screening were done.
Statistical analysis
The frequency of distribution of various causes for LBP and the distribution of various etiologies among different age groups were evaluated manually.
Results and Observation
This study involved a total of 235 cases. There were 121 males and 114 females. The age of the patient ranged from 21 to 68 years with an average of 41.3 years. Back pain was commonly observed in the third to fifth decade. The distribution of back pain in different age groups is tabulated in Table 1.
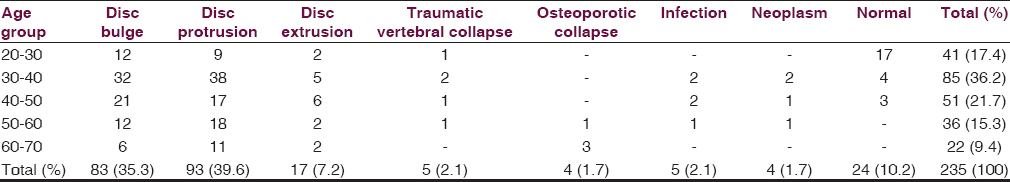
The common causes for back pain are disc herniations (disc bulge – 35.3%, disc protrusion – 39.6%, disc extrusion – 7.2%) accounting to 82.1%, followed by normal study (10.2%), vertebral collapse (traumatic – 2.1%, osteoporotic – 1.7%), infections (2.1%), and neoplasm (1.7%) [Chart 1].

- Distribution of various causes of low back pain
The most common etiology in this study was disc disease and herniation. Disc herniations when associated with ligamentum flavum thickening and facetal joint hypertrophy results in lumbar canal stenosis. There were forty cases of lumbar canal stenosis in our study which was more common in middle- and old-age group. The second most common condition found associated with disc herniations were spondylolysis with or without listhesis. Our study showed 18 cases of spondylolysis with or without listhesis. Vertebral collapse either due to trauma or osteoporosis, and infective etiologies (pyogenic and tuberculous) were the other most common causes; whereas neoplastic conditions were rare causes of back pain in our study. MRI lumbar spine did not show any abnormality with normal study in 24 cases (10.2%) but incidentally other causes of back pain such as ruptured cyst, hemorrhagic cyst, and pelvic inflammatory diseases in females, ureteric calculus with hydroureteronephrosis in males were found.
Discussion
The prevalence of LBP in Indian population has been found to vary between 6.2% (in general population) to 92% (in construction workers). Low socioeconomic status and poor education have been found to be associated with LBP.[3] In this study, back pain was observed more in males, and it was commonly seen in third and fourth decades.
Disc degeneration
Disc degeneration is commonly seen in elderly age group. Intervertebral disks likely degenerate because of reduction in oxygen and nutrient supply due to the normal aging process or trauma. In this study, most of the degenerations are due to normal aging process. Vertebral endplates play a key role in providing the nutrients to intervertebral disks. T1- and T2-weighted sagittal and axial MRI can clearly visualize the vertebral endplates and intervertebral disks. T2-weighted images show good contrast between the outer part of the annulus, which is more fibrous tissue (low signal), and inner part of the annulus and nucleus pulposus, which have more water content (high signal). Modic et al. described three types of endplate changes. Type 1 is low signal on T1-weighted images and high signal on T2-weighted images and likely represents endplate edema. Type 2 is high signal on T1-weighted images and on T2 fast spin-echo images but is dark on fat-suppressed sequences and likely represents fat. Type 3 is low signal on both T1- and T2-weighted sequences and represents endplate sclerosis. These endplate changes are commonly referred to as “Modic” changes.[4] MRI, in our study, also showed Modic changes ranging from Type 1 to Type 3.
Disc herniations (bulges, protrusion, extrusion)
MRI is the method of choice for the evaluation of disk morphology because of the good sensitivity (60–100%) and specificity (43–97%) for disk herniations (both protrusions and extrusion).[2] The lower specificity of MRI can be attributed to the high prevalence of degeneration (46–93%) and protrusions (20–80%) in asymptomatic adults.[5] In a study by Hapani et al., 7/35 patients presented with disc herniations.[6] A bulging disk is not considered a herniated disk and is defined as the presence of disk tissue diffusely (>50% of the circumference) extending beyond the edges of the ring apophyses. This bulging can be symmetric or asymmetric. Herniations are subdivided into protrusion and extrusions. As defined by the Combined Task Forces, a “protrusion is present if the greatest distance in any plane between the edges of the disc material beyond the disc space is less than the distance between the edges of the base in the same plane.” If in any plane, the greatest distance between the edges of the disk goes beyond the distance between the edges of the base, the lesion is called “extrusion.”[7] In practical terms, if the herniated disk material has a neck, it is an extrusion. Migration indicates the displacement of disc material away from the site of extrusion. Sequestration is used to indicate that the displaced disc material has lost completely any continuity with the parent disc. This study shows 93 cases of disc protrusions [Figure 1], 83 cases of disc bulge [Figure 2], and 17 cases of disc extrusion [Figure 3], which were diagnosed accordingly to their definition.

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows mild disc degeneration and right posterolateral disc protrusion at L4–L5 and L5–S1 level

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows diffuse L4–L5 disc bulge with left posterolateral annular tear

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows L4–L5 disc degeneration with posterocentral disc extrusion and inferior migration
Lumbar canal stenosis
Lumbar spinal stenosis has been associated with “buttock or lower extremity pain, which may occur with or without LBP, and is associated with diminished space available for the neural and vascular elements in the lumbar spine.” The reported sensitivity and specificity of MRI for the diagnosis of spinal stenosis varies from 77% to 90% and 72% to 100%, respectively.[8] Spinal stenosis can occur for various reasons, such as congenital spine abnormalities and disk herniation, but classically consists of the triad of disk bulge with facet hypertrophy and hypertrophy of the ligamentum flavum. In general, MRI is considered the best approach for the workup of spinal stenosis. In a study by Hapani et al., 4/7 cases of disc herniations were the causes for moderate to severe spinal canal stenosis.[6] In this study, there were forty cases of spinal canal stenosis [Figure 4], all of which were secondary to disc herniations, and there were no cases of congenital anomalies causing stenosis.

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows L3–L4 disc degeneration with circumferential bulge together with facetal joint hypertrophy and ligamentum flavum thickening causing lumbar canal stenosis
Spondylolysis and spondylolisthesis
Lumbosacral spondylolysis is a unilateral or bilateral defect of the pars interarticularis that affects one or more of the lumbar vertebrae. Lumbosacral spondylolysis is most common at L5, accounting for 85% of all cases,[9] and it is the most common cause of the spondylolisthesis.[10] In this study, there were 18 cases of spondylolisthesis; 12 of which were due to spondylolysis and the rest were by malalignment of facetal joints, and most of all cases involved L5–S1 vertebral level [Figure 5]. Hapani et al. observed spondylolysis in 4/35 patients with LBP.[6]

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows anterolisthesis of L5 over S1 with posterior pseudodisc bulge
Infective spondylodiscitis
MRI is the method of choice for evaluation of spinal infections, with sensitivity of 96% and specificity of 92%, using final clinical, histologic, and microbiologic information as the reference standard.[11] Koch's infection was found to be the most common cause of infective spondylitis. Classic imaging findings such as marrow changes, endplate erosion, disc involvement, pre and paravertebral abscesses supports the diagnosis of tuberculous infective spondylitis. Well defined paraspinal abnormal signal and thin and smooth enhancement of abscess wall are the two most reliable MRI findings suggesting tuberculous spondylitis. Though multiple vertebral involvements are common in tuberculosis, single vertebral involvement may also be seen. This study involved five infectious causes, four of which were of tuberculous etiology and one was due to pyogenic infection. One case of tuberculous spondylitis was associated with psoas abscess [Figure 6].

- T1- and T2-weighted sagittal (a and b) magnetic resonance imaging shows L5–S1 end plate irregularity with subchondral marrow changes with prevertebral and epidural soft tissue component. T2-weighted axial (c) and short tau inversion recovery coronal images (d) shows hyperintense paravertebral psoas abscess
Trauma
Fractures of lumbar vertebrae can be due to either severe trauma or pathologic weakening of the bone. Osteoporosis is the underlying cause of many lumbar fractures, especially in postmenopausal women. In this study, there were five cases of traumatic fractures and four cases of compression fractures secondary to osteoporosis. MRI clearly depicts cord compression due to displaced bone or disk. MRI also clearly shows bone marrow edema, helping to identify which fractures are acute. Edema is better visible in the sagittal plane using fat-suppressed T2-weighted [Figure 7] or STIR sequences.[12] Other potential findings that could indicate acute versus chronic fracture are paravertebral hemorrhage and spinal cord edema. Moreover, MRI findings can be used to differentiate between malignant versus benign vertebral fractures. The presence of each one of the following findings could indicate spinal metastasis: Vertebral body expansion with a convex posterior border, abnormal signal completely replacing normal marrow and extending into the posterior elements, and presence of a paraspinal mass.[13] In contrast, low-signal bands in the vertebral bodies on T1- and T2-weighted images, normal bone marrow appearance, and presence of several compression fractures are more in support of benign osteoporotic compression fractures.

- T2-weighted sagittal (a) and axial (b) magnetic resonance imaging shows traumatic anterior wedge compression of L1 vertebral body with marrow edema and retropulsion of posterosuperior border indenting thecal sac and cord
Tumor
Neoplasm is a rare cause for LBP and may range from a completely benign, sclerotic enostosis (bone Island) to a malignant bone tumor. Primary bone tumors of the spine are much less common than secondary metastatic disease. MRI is the best approach for evaluation of spine metastases because its high soft-tissue contrast results in excellent sensitivity. The reported sensitivity of MRI varies from 83% to 100%, and the estimated specificity is 92%.[14] Spinal metastases can be intramedullary, extramedullary–intradural, or extradural. T2-weighted MRI shows intramedullary lesions as areas with high-intensity signals that enhance with contrast administration. In a study by Hapani et al., posterior epidural hemangioma and bony metastasis in a known case of Ewing's sarcoma were the only two neoplastic conditions that were causing back pain.[6] Shih et al. reported that an ill-defined margin, pedicle involvement, a marked, heterogenous MR enhancement pattern, and an irregular nodular type paravertebral soft tissue lesion are MRI characteristics of malignant solitary vertebral collapse.[15] In addition, pedicle change in the presence of expansile lesion is an important MRI finding that totally excludes a benign cause. Therefore, MRI can be a useful diagnostic tool for the differential diagnosis of solitary vertebral collapse. Our study shows four cases of neoplasms causing back pain which includes a case of aggressive bone tumor, showing L5 vertebral collapse with posterior convexity and subchondral marrow changes corresponding to expansile lytic lesion involving right hemivertebra, pedicle, and transverse process [Figure 8]. Biopsy from the lesion showed features of malignant giant cell tumor. Vertebral hemangioma with epidural soft tissue component causes extraneous compression of cord [Figure 9], multiple myeloma, and metastatic renal cell carcinoma.

- T1- and T2-weighted sagittal (a and b) magnetic resonance imaging shows L5 vertebral collapse with posterior convexity and marrow signal changes. Axial T2-weighted magnetic resonance imaging (c) and computed tomography scan (d) images shows heterogenously hyperintense signal corresponding to expansile lytic lesion involving right hemivertebra, pedicle, and transverse process

- T1-weighted, T2-weighted and short tau inversion recovery sagittal (a-c) dorsolumbar magnetic resonance imaging shows hemangiomatous changes involving D12 vertebral body and D8 vertebral body including posterior arch elements with epidural soft tissue component in posterior aspect compressing the cord extraneously. Short tau inversion recovery coronal image (d) shows D11 butterfly vertebra
Miscellaneous
MRI did not show any abnormality of lumbar spine in 24 cases (10.2%). Most of these patients with normal study were young females. Incidentally other causes of back pain such as ruptured cyst, hemorrhagic cyst, and pelvic inflammatory diseases were found in females, whereas ureteric calculus with hydroureteronephrosis was found in males.
Conclusion
MRI with its inherent soft-tissue contrast resolution, multiplanar capability, and lack of ionizing radiation remains invaluable modality in evaluation of LBP, especially in disc and marrow pathology. This study shows high prevalence of LBP in middle age group among the rural population with disc degeneration and herniations as the common etiology of LBP. MRI remains the unique modality of choice in detailed evaluation of other LBP causes such as spinal trauma, infections, and neoplastic conditions.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Diagnostic evaluation of low back pain with emphasis on imaging. Ann Intern Med. 2002;137:586-97.
- [Google Scholar]
- Epidemiology of low back pain in Indian population: A review. Int J Basic Appl Med Sci. 2015;5:166-79.
- [Google Scholar]
- Degenerative disk disease: Assessment of changes in vertebral body marrow with MR imaging. Radiology. 1988;166((1 Pt 1)):193-9.
- [Google Scholar]
- Lumbar spine MRI for low back pain: Indications and yield. Am J Roentgenol. 2010;195:550-9.
- [Google Scholar]
- Magnetic resonance imaging of back pain in young population. J Evol Med Dent Sci. 2014;3:12644-9.
- [Google Scholar]
- Nomenclature and classification of lumbar disc pathology: Recommendations of the combined task forces of the North American Spine Society, American Society of Spine Radiology, and American Society of Neuroradiology. Spine. 2001;26:E93-113.
- [Google Scholar]
- Diagnosis of lumbar spinal stenosis in adults: A metaanalysis of the accuracy of CT, MR, and myelography. AJR Am J Roentgenol. 1992;158:1135-44.
- [Google Scholar]
- Spondylolisthesis in children. Cause, natural history, and management. Spine (Phila Pa 1976). 1999;24:2640-8.
- [Google Scholar]
- Bone marrow edema in osteoporotic vertebral compression fractures after percutaneous vertebroplasty and relation with clinical outcome. AJNR Am J Neuroradiol. 2006;27:983-8.
- [Google Scholar]
- Trauma of the spine and spinal cord: Imaging strategies. Eur Spine J. 2010;19(Suppl 1):S8-17.
- [Google Scholar]
- Does bone SPECT actually have lower sensitivity for detecting vertebral metastasis than MRI? J Nucl Med. 1996;37:975-8.
- [Google Scholar]
- Solitary vertebral collapse: Distinction between benign and malignant causes using MR patterns. J Magn Reson Imaging. 1999;9:635-42.
- [Google Scholar]






