Translate this page into:
The Association between Sagittal Index, Canal Compromise, Loss of Vertebral Body Height, and Severity of Spinal Cord Injury in Thoracolumbar Burst Fractures
Address for correspondence: Dr. Mehmet Sabri Gürbüz, Yıldıztepe Mah. Bağcılar Cad. No. 108 34203 Bağcılar, İstanbul, Turkey. E-mail: mehmetsabrigurbuz@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Aim:
Our aim was to determine whether a combination of sagittal index (SI), canal compromise (CC), and loss of vertebral body height (LVBH) is associated with the severity of neurological injury in patients with thoracolumbar burst fractures.
Materials and Methods:
Seventy-four patients with thoracolumbar burst fracture undergoing instrumentation between 2010 and 2015 were analyzed retrospectively. The degree of neurological injury was determined using the American Spinal Injury Association (ASIA) scoring system. The association between the morphology of the fracture and the severity of neurological injury was analyzed.
Results:
There was a strong association between fracture morphology and the severity of neurological injury. Of the patients, 77.5% with SI ≥20°, 81.6% with CC ≥40%, and 100% with LVBH ≥50% had lesion according to ASIA. All of 7 patients with ASIA A had SI ≥20°, CC ≥40%, and LVBH ≥50%. On the other hand, 79% of the patients with ASIA E had SI <20°, 83.7% of the patients with ASIA E had CC <40%, and all of the patients with ASIA E had LVBH <50%. SI, CC, and LVBH were lower in neurologically intact patients (ASIA E), whereas they were higher in patients with neurological deficits (ASIA A, B, C, D) (P = 0.001; P < 0.01). These measurements had 100% negative predictive values and relatively high positive predictive values.
Conclusion:
SI, CC, and LVBH are significantly associated with the severity of neurological injury in patients with thoracolumbar burst fractures. The patients with SI >25°, the patients with CC >40%, and the patients with LVBH >50% are likely to have a more severe neurological injury.
Keywords
American Spinal Injury Association score
fracture morphology
measurement
neurological injury
radiological characteristic
INTRODUCTION
There are certain prognostic factors to determine the neurological outcome of the patients in spinal cord injury (SCI). Etiology, severity of trauma, and preoperative neurological condition are the most important factors influencing the prognosis.[123] Patients with a complete SCI have a <5% chance of neurological recovery whereas the prognosis is much better for the patients with an incomplete SCI. On the other hand, there is no consensus about the association between the severity of the SCI and the radiological characteristics of the fracture.[45]
It is well known that posttraumatic neurological condition of the patient is the most important factor determining the extent of the neurological improvement which is the main goal of the treatment.[67] To reach this aim, we need to evaluate radiology of the fractured vertebra and correlate this to the neurological condition of the patient. By assessing the morphology of the fracture, it might be possible to determine the severity of the injury and to identify the patients who would have a chance of neurological recovery. There are many measurement methods to evaluate the fracture morphology. Sagittal index (SI), canal compromise (CC), and loss of vertebral body height (LVBH) are the most accepted measurement techniques to assess the radiological characteristics of thoracolumbar burst fractures.[8910111213]
Association between SI, CC, LVBH and neurological damage is controversial. Each measurement technique has certain limitations when evaluated individually. To make a more comprehensive evaluation, it might be useful to measure SI, CC, and LVBH together and search for their correlation to the degree of neurological injury. For this reason, we calculated the SI, CC, and LVBH in thoracolumbar burst fractures and aimed to determine whether- and to what extent these 3 parameters are associated with the severity of neurological injury.
MATERIALS AND METHODS
Seventy-four patients with thoracolumbar burst fracture undergoing thoracolumbar instrumentation between 2010 and 2015 were analyzed retrospectively. All of the patients underwent a transpedicular screw fixation of 2-level above and 2-level below the fractured vertebra. Patients with multisegmental fractures, pathological or osteoporotic fractures, and patients with ankylosing spondylitis were excluded from the study. Magnetic resonance (MR) imaging scans of the patients were analyzed. To identify the morphology of the injury; SI, CC, and LVBH were calculated as proposed in the literature.
Mid-sagittal T2-weighted MR images were used to determine the SI as proposed by Farcy et al.,[8] SI was calculated as the kyphotic deformity at the fracture motion segment level minus the normal contour (baseline value). An angle of 5° in the thoracic, 0° at the thoracolumbar junction, and 10° in lumbar region were considered baseline values [Figure 1]. SI was classified as either <20° and ≥20°.
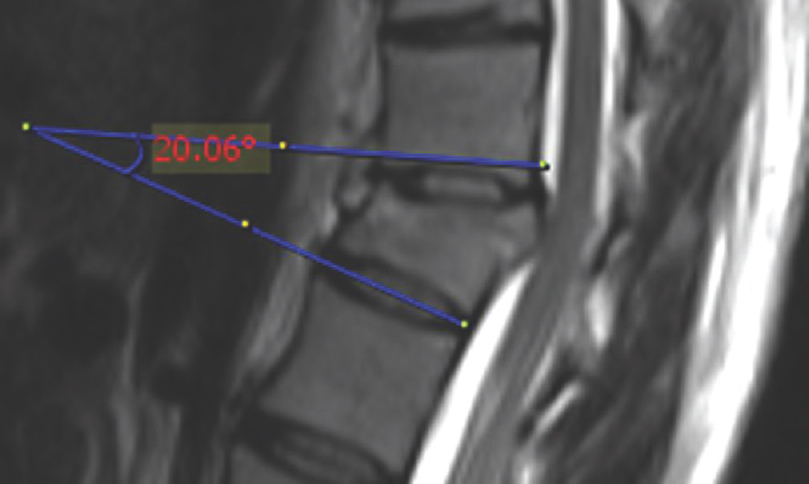
- Mid-sagittal T2-weighted magnetic resonance image showing the calculation of the sagittal index. The sagittal index was calculated as the kyphotic deformity at the fractured motion segment level minus the normal contour (baseline values). An angle of 5° in the thoracic, 0° at the thoracolumbar junction, and 10° in lumbar region were considered baseline values
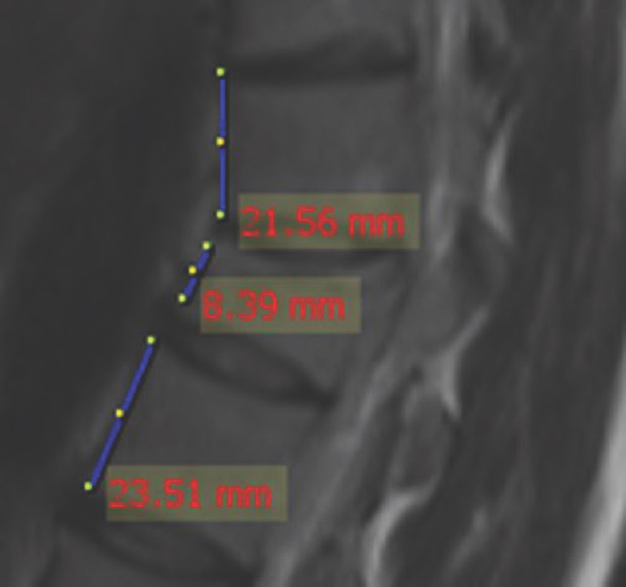
Mid-sagittal T2-weighted MR images were used to measure the CC as originally described by Fehlings et al.[9] for cervical spine and applied to the thoracolumbar region by Vaccaro et al.[14] The percentage of the CC was calculated using the narrowest mid-sagittal diameter of the spinal canal at the level of fractured vertebra, and the average mid-sagittal diameters of the spinal canal at one level above and below the fractured vertebra [Figure 2]. CC was classified as either <40% and ≥40%.

- Mid-sagittal T2-weighted magnetic resonance image showing the calculation of the canal compromise. The percentage of the canal compromise was calculated using the ratio of the narrowest mid-sagittal diameter of the spinal canal at the level of fractured vertebra to the average mid-sagittal diameter of the spinal canal at one level above and below the fractured vertebra
Mid-sagittal T2-weighted MR images were used to measure the LVBH as proposed by Keene.[11] The percentage of the LVBH was calculated using the anterior height of the injured vertebra and the mean of the anterior height of the adjacent two intact vertebrae [Figure 3]. LVBH was classified as either <50% and ≥50% as suggested by McAfee et al.[5] All measurements were done by two separate neurosurgeons, and the means were recorded to minimize the measurement errors.
- Mid-sagittal T2-weighted magnetic resonance image showing the calculation of the loss of vertebral body. The percentage of the loss of vertebral body height was calculated using the ratio of the anterior height of the injured vertebra to the mean of the anterior height of the adjacent two intact vertebrae
For the combined measurement, the patients were divided into two groups based on their SI, CC, and LVBH values. Group 1 included the patients with SI ≥20°, CC ≥40%, and LVBH ≥50%. Group 2 included the patients with SI <20°, CC <40%, and LVBH <50%.
The International Standards for Neurological Classification of SCI, published by the American Spinal Injury Association (ASIA) and revised in 2011,[15] was used to identify the neurological conditions of the patients. The degree of neurological injury was determined based on their ASIA scores on admission to the emergency department. The terms “Normal neurological function,” “Neurologically intact,” and “No lesion” were used for ASIA E whereas “Lesion” was used for ASIA A, B, C, and D. The term “Complete SCI” was used for ASIA A whereas “Incomplete SCI” was used for the scores in between (ASIA B, C, and D). The term ’High score’ was used for ASIA A, B, C, and D whereas “Low score” was used for ASIA E. For scoring, neurological examination notes of both emergency department and the neurosurgeons were taken into consideration.
Statistical analysis was performed using Number Cruncher Statistical System (NCSS) 2007 Statistical Software (NCSS LLC, Kaysville, Utah, USA). Association between the radiological measurements and ASIA scores was measured using the Fisher-Freeman test and Yates Continuity Correction. P < 0.05 was considered statistically significant.
RESULTS
Considering the inclusion criteria, 74 patients met the criteria (47 males and 27 females) with a mean age of 45.8 years ranging from 16 to 81 years.
SI was >20° in all of the patients with ASIA A, B, C, and D (lesion). However, SI was <20° in 79% of the patients with ASIA E (P = 0.001; P < 0.01) [Table 1]. The association between the SI and the severity of neurological injury was significant with 100% sensitivity, 79% specificity, 77.5% positive predictive value, 100% negative predictive value, and 87.8% accuracy [Table 2].
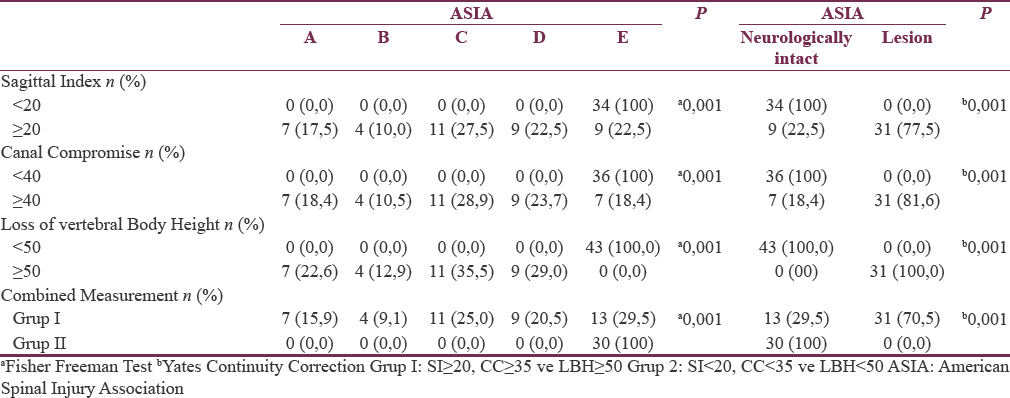
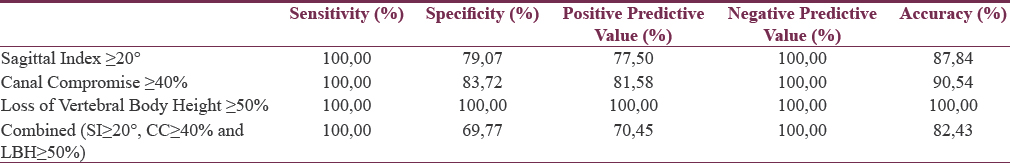
CC was >40% in all of the patients with ASIA A, B, C, and D (lesion). However, CC was <40% in 83.7% of the patients with ASIA E (P = 0.001; P < 0.01) [Table 1]. The association between the SI and the severity of neurological injury was significant with 100% sensitivity, 83.7% specificity, 81.5% positive predictive value, 100% negative predictive value, and 90.5% accuracy [Table 2].
LVBH was >50% in all of the patients with ASIA A, B, C, and D (lesion) and <50% in all of the patients with ASIA E (P = 0.001; P < 0.01) [Table 1]. The association between the SI and the severity of neurological injury was significant with 100% sensitivity, 100% specificity, 100% positive predictive value, 100% negative predictive value, and 100% accuracy [Table 2].
Combining these three variables together, of the patients in group 1 (SI ≥20°, CC ≥40% and LVBH ≥50%), 70.4% had a high ASIA score (ASIA A, B, C, D). Similarly, of the patients in Group 2 (SI <20°, CC <40%, and LVBH <50%), all had a low ASIA score (ASIA E) (P = 0.001; P < 0.01) [Table 1]. There is a strong association between fracture morphology (high scores of SS, CC, and LVBH) and the severity of neurological with 100% sensitivity, 69.7% specificity, 70.4% positive predictive value, 100% negative predictive value, and 82.4% accuracy [Table 2].
DISCUSSION
The thoracolumbar spine, which generally refers to the T11-L2 spinal segments, is located at the junction of two physiological spinal curvatures.[6] Since this region is the most mobile region, these spinal segments are particularly vulnerable to fractures.[316]
There is no consensus regarding the exact cause of neurologic deficits in thoracolumbar burst fractures.[1718] There is a general agreement that SCI occurs at the time of trauma, but the debate still exists about the role of secondary factors such as persistence of a bone fragment compressing the spinal cord, segmental kyphosis, or compression of vertebral body.[119] Considering the anatomy and biomechanics of the vertebral column and spinal cord, segmental kyphosis, CC, and loss of height of vertebral body are among the leading factors playing role in SCI.[202122]
Dendrinos et al.[1] pointed out that thoracolumbar burst fractures with severe kyphosis have a better prognosis, in case the restoration of the sagittal alignment of the spinal column is achieved. SI is the measurement of segmental kyphosis at a mobile segment of spinal column including 1 vertebra and 1 disc. Farcy et al.[8] reported that SI >15° is predictive of progression of segmental kyphosis. They assessed SI, instability grade, and neurologic status of the patients at injury and after treatment. Surgical management was suggested for the patients with SI >15°. In our series, the patients with SI >20° had a higher rate of neurological deficit (P < 0.05), 77.5% of them having lesion according to the ASIA classification system (ASIA A, B, C, D). On the other hand, of the patients with ASIA E, 79% had a SI <20° (P < 0.05). The association between the SI and the severity of neurological injury was significant with 87.8% accuracy.
One of the most important factors leading to neurological deficit is believed to be the invasion of the spinal canal by the retropulsed bony fragments. Hashimoto et al.[10] reported a strong association between narrowing of the spinal canal and the level of the neurological injury. Dendrinos et al.[1] found a significant association between initial neurological damage and the amount of CC. Vaccaro et al.[14] found a certain correlation between ASIA score and the amount of CC in thoracolumbar burst fractures. In our series, the patients with CC >40% had a higher rate of neurological deficit (P < 0.05), 81% of them having lesion according to ASIA classification system (ASIA A, B, C, and D). On the other hand, of the patients with ASIA E, 83.7% had a CC <40% (P < 0.05). The association between the CC and the severity of neurological injury was significant with 90.5% accuracy.
Vaccaro et al.[14] emphasized a certain association between ASIA scale and loss of the height of vertebral body. Isomi et al.[20] studied experimental burst fractures of the L1 vertebrae of human cadaveric thoracolumbar spine and showed a significant correlation between the LVBH and the canal encroachment. In our series, the patients with LVBH >50% had a higher rate of neurological deficit (P < 0.05), all of them having lesion according to ASIA classification system (ASIA A, B, C, and D). On the other hand, of the patients with ASIA E, all had an LVBH <50% (P < 0.05). The association between the LVBH and the severity of the neurological injury was significant with 100% accuracy.
As seen from the relevant literature, association between fracture morphology (SI, CC, and LVBH), and the degree of neurological damage remains controversial. Each measurement technique has certain limitations when evaluated individually. Dendrinos et al.[1] found no correlation between initial neurological damage and posttraumatic segmental kyphosis. Some authors[1023] suggest that the canal encroachment by bony fragments adds to the neurological damage while others report no correlation between the CC and neurological damage.[524] Although some authors reported an association between LVBH and neurological status of the patients,[1420] whereas some authors have found no such correlation.[2526] In our series, we combined these 3 parameters and detected that there is a strong association between this combination and the severity of neurological injury. The severity of neurological injury increases as long as the degree of SI, the amount of CC, and the amount of LVBH increase. In other words, SS, CC, and LVBH were lower in patients with lower ASIA scores (ASIA E) whereas they were higher in patients with higher ASIA scores.
CONCLUSION
There is a strong association between SI, CC, and LVBH, and the severity of neurological injury in thoracolumbar burst fractures undergoing instrumentation. The patients with SI >20°, the patients with CC >40%, and the patients with LVBH >50% are likely to have a more severe neurological injury.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Factors influencing neurological recovery in burst thoracolumbar fractures. Acta Orthop Belg. 1995;61:226-34.
- [Google Scholar]
- A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994;3:184-201.
- [Google Scholar]
- Burst fractures in the thoracic and lumbar spine. A clinico-neuropathologic analysis. Spine (Phila Pa 1976). 1989;14:1316-23.
- [Google Scholar]
- Vertebral fractures without neurological deficit. A long-term follow-up study. J Bone Joint Surg Am. 1988;70:1319-21.
- [Google Scholar]
- The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am. 1983;65:461-73.
- [Google Scholar]
- Plating of thoracic, thoracolumbar, and lumbar injuries with pedicle screw plates. Orthop Clin North Am. 1986;17:147-59.
- [Google Scholar]
- Sagittal index in management of thoracolumbar burst fractures. Spine (Phila Pa 1976). 1990;15:958-65.
- [Google Scholar]
- The optimal radiologic method for assessing spinal canal compromise and cord compression in patients with cervical spinal cord injury. Part II: Results of a multicenter study. Spine (Phila Pa 1976). 1999;24:605-13.
- [Google Scholar]
- Relationship between traumatic spinal canal stenosis and neurological deficits in thoracolumbar burst fractures. Spine (Phila Pa 1976). 1990;13:1268-72.
- [Google Scholar]
- Radiographic evaluation of thoracolumbar fractures. Clin Orthop Relat Res. 1984;189:58-64.
- [Google Scholar]
- Radiographic measurement parameters in thoracolumbar fractures: A systematic review and consensus statement of the spine trauma study group. Spine (Phila Pa 1976). 2006;31:E156-65.
- [Google Scholar]
- Neurological deficit and canal compromise in thoracolumbar and lumbar burst fractures. J Orthop Surg (Hong Kong). 2008;16:20-3.
- [Google Scholar]
- The significance of thoracolumbar spinal canal size in spinal cord injury patients. Spine (Phila Pa 1976). 2001;26:371-6.
- [Google Scholar]
- International standards for neurological classification of spinal cord injury (revised 2011) J Spinal Cord Med. 2011;34:535-46.
- [Google Scholar]
- Validity of the three-column theory of thoracolumbar fractures. A biomechanic investigation. Spine (Phila Pa 1976). 1995;20:1122-7.
- [Google Scholar]
- Incidence and outcomes of spinal cord injury clinical syndromes. J Spinal Cord Med. 2007;30:215-24.
- [Google Scholar]
- Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine (Phila Pa 1976). 1993;18:955-70.
- [Google Scholar]
- Spinal instability as defined by the three-column spine concept in acute spinal trauma. Clin Orthop Relat Res. 1984;189:65-76.
- [Google Scholar]
- Radiographic parameters for evaluating the neurological spaces in experimental thoracolumbar burst fractures. J Spinal Disord. 2000;13:404-11.
- [Google Scholar]
- Canal and intervertebral foramen encroachments of a burst fracture: Effects from the center of rotation. Spine (Phila Pa 1976). 2001;26:1231-7.
- [Google Scholar]
- Unstable thoracolumbar fractures. A comparative clinical study of conservative treatment and Harrington instrumentation. Spine (Phila Pa 1976). 1985;10:111-22.
- [Google Scholar]
- Scoliosis research society. Multicenter spine fracture study. Spine (Phila Pa 1976). 1992;17:528-40.
- [Google Scholar]
- Effect of surgery on motor recovery following traumatic spinal cord injury. Spinal Cord. 1996;34:188-92.
- [Google Scholar]
- The retrospective analysis of posterior short-segment pedicle instrumentation without fusion for thoracolumbar burst fracture with neurological deficit. ScientificWorldJournal 2014 2014:E1-8.
- [Google Scholar]
- Correlation of posterior ligamentous complex injury and neurological injury to loss of vertebral body height, kyphosis, and canal compromise. Spine (Phila Pa 1976). 2012;37:1142-50.
- [Google Scholar]






