Translate this page into:
Moyamoya Disease as a Cause of Stroke in a Child with Tetralogy of Fallot
Address for correspondence: Dr. Shambhavi, Senior Resident, Department of Pediatrics, J. K. Lon Hospital, Sawai Man Singh Medical College, Jaipur, Rajasthan, India. E-mail: 21me.shambhavi@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Moyamoya disease is a rare, chronic, idiopathic, and progressive vaso-occlusive disease of cerebral blood vessels. Due to its chronic nature, a number of collaterals form at the base of brain giving a “smoke of puff” (”moyamoya” in Japanese), appearance in angiography. It was first reported in Japan in 1957.[1] Its worldwide incidence is 0.07%;[2] highest in Japan.[3] Its idiopathic form has to be distinguished from moyamoya syndrome which is known to be associated with neurofibromatosis, Downs, Turners, Alagille, and Williams Syndrome.[4] Its association with congenital heart disease (CHD) was first time reported in 1998,[4] but still it is an under-recognized cause of stroke and seizure in CHDs.
We report a child with tetralogy of Fallot (TOF) presenting with stroke due to moyamoya disease.
A 5-year-old female child presented with complaints of sudden loss of speech for 1 day progressing to decreased movement of right upper and lower limbs within few hours. History revealed one episode of generalized tonic–clonic seizure lasting for about 5 min, at the age of 18 months, for which the child was not evaluated. On examination, the patient was irritable, having central cyanosis, clubbing, deviation of angle of mouth to left and upper motor neuron type right-sided hemiparesis. Cardiac evaluation showed left parasternal heave with short systolic murmur in pulmonary area. Provisional diagnosis of congenital cyanotic heart disease most probably TOF with intracranial thrombosis versus brain abscess was kept. Chest radiography had features of right ventricular hypertrophy. Her hematocrit was 65.8%; rest blood investigations were normal. Two-dimensional echocardiography confirmed TOF. Magnetic resonance imaging of the brain with diffusion-weighted imaging was done which showed large acute infarcts in left middle cerebral artery (MCA) territory with mild contralateral midline shift. Diffuse cortical hyperintensities were seen in distribution of right MCA and bilateral anterior cerebral artery territories. No contrast enhancement was seen [Figure 1]. Magnetic resonance angiography showed marked irregular narrowing of supraclinoid portions of bilateral internal carotid arteries and bilateral M1 middle cerebral arteries with multiple collaterals, suggesting moyamoya disease [Figure 2].
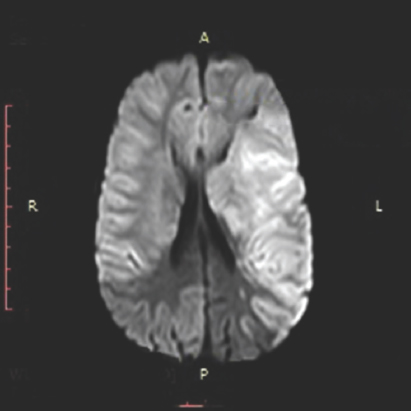
- Magnetic resonance imaging with diffusion-weighted imaging showing large acute infarcts in left middle cerebral artery territory involving left basal ganglia, including insula, left temporal lobe, left parietal lobe and left posterior frontal lobe with effacement of underlying sulci, and mild contralateral midline shift
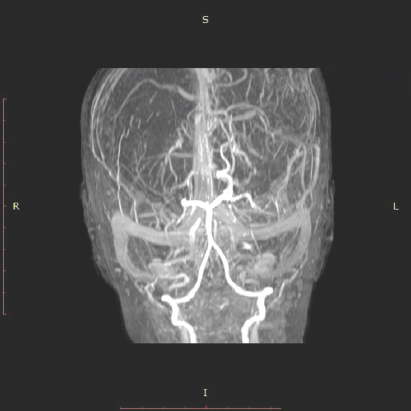
- Magnetic resonance angiography showing marked irregular narrowing of supraclinoid portions of bilateral internal carotid arteries and bilateral M1 middle cerebral arteries with multiple collaterals, suggestive of moyamoya disease
The child was managed conservatively; her neurosurgical intervention was planned after angiography, but she succumbed to the disease before procedure.
Children with CHDs are at increased risk of seizures and strokes throughout their lives. Most common causes of stroke in children with TOF are cerebral thrombosis due to polycythemia, thromboembolism, and brain abscess. Our child had hematocrit of 65.8% suggesting cerebral thrombosis. Possibility of brain abscess, commonly seen in these patients, was also kept.
Lutterman et al. initially reported association of moyamoya syndrome with CHDs. In their study of five children, one had TOF.[4] Shoukat et al. studied a series of 13 patients with moyamoya disease where two had CHDs.[5]
Its presentation varies with age; adults present with intracranial hemorrhages while children present with seizure and stroke. Treatment includes neurosurgical intervention such as encephalo-duro-arterio-myo-synangiosis, direct revascularization through the superficial temporal artery, and the middle cerebral artery bypass, combined approaches and rarely, denervation of cerebral vasculature.[5]
This case broadens the etiology of stroke in CHDs and highlights the fact that moyamoya disease should be kept in differential diagnosis of such cases.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Worldwide distribution of moyamoya disease. Neurol Med Chir (Tokyo). 1992;32:883-6.
- [Google Scholar]
- Clinical features of probable moyamoya disease in Japan. Clin Neurol Neurosurg. 1997;99(Suppl 2):S173-7.
- [Google Scholar]
- Moyamoya syndrome associated with congenital heart disease. Pediatrics. 1998;101:57-60.
- [Google Scholar]
- Moyamoya disease: A clinical spectrum, literature review and case series from a tertiary care hospital in Pakistan. BMC Neurol. 2009;9:15.
- [Google Scholar]





