Translate this page into:
Rates and Correlations of Psychiatric Drug Administration in a Rehabilitation Center
Address for correspondence: Dr. Vaios Peritogiannis, Moulaimidou Street 1, Ioannina 45444, Greece. E-mail: vaios.peritogiannis@medai.gr
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Physical injury has been associated with the development of several psychopathological manifestations. Less is known about the use of psychiatric medication in those patients.
Objectives:
This study aimed to explore the use of psychiatric medication by patients been admitted in a rehabilitation center in a tertiary care teaching hospital and to inquire for the correlations of such drug administration.
Materials and Methods:
The sample consisted of 127 patients who had been admitted to a rehabilitation center, being in the postacute phase of their condition during a 2-year period. Patients’ medical records were searched for the demographic and clinical information.
Results:
Analysis was performed for 118 patients, mostly men (62.7%) with the mean age of 57.5 years. About 43.2% of patients (n = 51) were referred for psychiatric consultation, and 39.8% (n = 47) were prescribed a psychiatric drug. Traumatic brain injury was the diagnosis, positively correlated to referral. Twenty-seven out of the 67 nonreferred patients (40.3%) were prescribed psychiatric regimens by physicians. Nearly 38.1% of patients were diagnosed with a psychiatric disorder by the consultation-Liaison psychiatric service.
Conclusions:
In a rehabilitation center, psychiatric drug administration is common practice and drugs may be prescribed by the center's physicians and by psychiatrists. Such a drug prescription was found to be correlated to referral to the consultation-Liaison psychiatric service.
Keywords
Consultation-Liaison psychiatry
psychiatric medication
rehabilitation
traumatic brain injury
INTRODUCTION
The association between physical injury and psychiatric disorders has been the subject of extensive investigation. Patients facing a traumatic event have been reported to present with several psychopathological manifestations, such as delirium and other organic brain syndromes, depression, and anxiety disorders. A number of reports have supported the correlation between stroke or traumatic brain injury (TBI) and depressive or anxiety syndromes.[12345] Other studies have examined the frequency of psychiatric disorders after a cerebrovascular event or traumatic injury requiring rehabilitation,[6] whereas other research documented high rates of psychological disorders after spinal cord injury.[789] It has been shown that the development of psychiatric syndromes adversely affects the rehabilitation process and the outcome of injuries and related conditions.[1011]
Less is known about the use of psychiatric medication in those patients. Some studies have reported on the effectiveness of antidepressants in patients suffering from depression after TBI,[1213] but evidence is lacking regarding the everyday clinical practice of administration of psychiatric medication to inpatients attending short-term rehabilitation programs during the postacute phase. Notably, a recent study comprising data from four European rehabilitation centers revealed significant differences among countries in the prevalence and treatment of depression.[14] In a recent multisite study on the use of any psychotropic medication during inpatient rehabilitation in patients with TBI, it was found that almost all patients (95%) received a psychotropic agent. However, the “psychotropic medication” category was broadly defined in this study and comprised narcotic analgesics, anticonvulsants, and anti-Parkinson agents, as well as psychiatric drugs, such as antidepressants and antipsychotics; anxiolytics and hypnotics were also included.[15] Similarly, another recent study on TBI patients reported all psychotropic medication use to be as high as 83.9%.[16] As in the study by Hammond et al.,[15] psychotropic medication was broadly defined. In the study of Craig et al. on spinal cord injury patients, psychotropic medications were prescribed to >36% of the sample, with most being antidepressants.[8] Furthermore, depression shows high rates in stroke patients, with dominant symptom the insomnia.[17] Moreover, a recent study found all-cause mortality to increase in stroke patients treated with psychotropic medications.[18]
Objectives
The primary objective of the present study was to explore the use and the administration of psychiatric medication by patients been admitted in a rehabilitation center in a tertiary care teaching hospital; a secondary objective was to inquire for the correlations of such drug administration.
MATERIALS AND METHODS
This study setting was the rehabilitation center of the University Hospital of Ioannina, Northwestern Greece. This is a 40-bed facility which provides multidisciplinary services for patients in the postacute phase after a traumatic event. According to the rehabilitation center's guidelines, patients stay in the center for 6 weeks, regardless of the outcome; they may continue treatment in other services afterward. The cooperation of the center with other wards of the hospital, such as the neurology, neurosurgery, and orthopedics, and with the consultation Liaison psychiatry (CLP) is well established. Patients presenting psychopathological manifestations may be referred to the CLP for full evaluation of their mental state.
This study was a retrospective chart review. All admissions during the last 2 years were considered. Patients’ medical records were searched for demographic (age, gender), and clinical information (diagnosis, referral to CLP, drug administration, and other interventions, such as psychotherapeutic interventions and counseling). Primary diagnoses (that are disorders requiring admission in the rehabilitation center) included cerebrovascular event, TBI, orthopedic diseases, and other neurologic disorders. Psychiatric drugs comprised antipsychotics, antidepressants, and anxiolytics, namely, benzodiazepines, as these types of drugs were widely used in rehabilitation centers. All patients aged 17 years or older were included. Exclusion criteria were age < 17 years and the presence of chronic psychiatric history and treatment with a psychiatric drug regimen before admission to the hospital. Despite the fact that people with psychiatric history are in a high risk for accidents resulting in traumatic brain injuries or other serious damages, the aim of the study was to assess the management of medication not only by a psychiatrist but also by doctors of other specialties. However, patients with delirium manifestations during their hospitalization were included. This study protocol has been approved by the University Hospital of Ioannina ethics committee.
Statistical analysis
Data are presented as absolute numbers and percentages for binary variables and as mean with standard deviation for continuous variables. Data are reported separately for patients who were referred to CLP and for nonreferred patients. Comparisons between the two patient groups were performed using Chi-square or Fisher's exact test for binary variables and Mann–Whitney test for categorical variables. All P < 0.05 were considered statistically significant. The statistical software SPSS version 22 (SPSS Inc., Chicago, IL, USA) was used for data analysis.
RESULTS
A total of 127 patients had been admitted to the center during the study period. With the application of the exclusion criteria, 9 of them (2 patients < 17 years and 7 patients having a prior psychiatric diagnosis with current treatment by psychiatric drug) were excluded from analysis. Patients’ (n = 118) characteristics are presented in Table 1. In the majority, they were male and their mean age was 57.5 years.

A significant proportion of patients (43.2%) were referred for psychiatric consultation [Table 1]. The association of primary diagnosis with referral to CLP and with psychiatric drug administration was examined. The results showed that diagnosis appeared to be associated with referral [Table 2]. Patients with TBI were more likely to be referred, whereas patients with orthopedic diseases were less likely to be referred to the CLP. There was no association of patients’ primary diagnosis with psychiatric drug administration. Patients’ psychiatric diagnoses, according to the CLP evaluation are presented in Table 3.
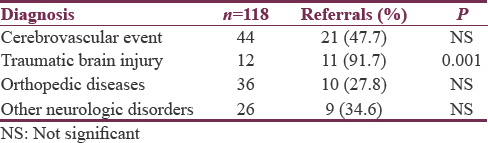
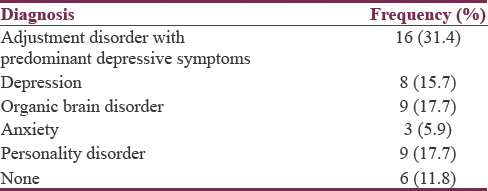
Table 4 presents the prescription of several psychiatric drugs by the psychiatrists of the consultation-Liaison service and by the center's physicians, according to their clinical judgment, without a formal psychiatric examination.
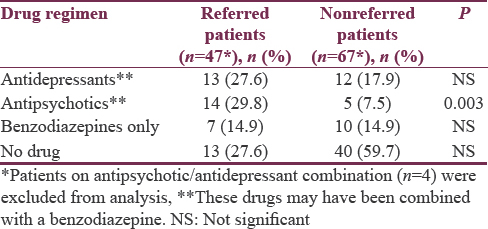
Thirty-eight out of 51 referred patients were prescribed a psychiatric medication, whereas twenty-seven out of the 67 nonreferred patients (40.3%) were prescribed psychiatric regimens by physicians. Those medications included antidepressant and antipsychotic compounds, whereas a benzodiazepine regimen could be prescribed for the short-term management of anxiety or insomnia. There was a significant correlation between referral and psychiatric drug prescription. Patients been referred to the CLP were more likely to be prescribed a psychiatric drug regimen. Nonreferred patients were less likely to receive a psychiatric agent.
DISCUSSION
This study retrospectively examined the use of psychiatric medication in patients being in a postacute phase of a condition requiring rehabilitation and been admitted in a rehabilitation center. Another study objective was to inquire for the possible correlations of such drug administration. In total, psychiatric drugs were prescribed in 65 patients out of 118 admissions (55.1%). Importantly, in 27 of those cases psychiatric drugs had been prescribed by the center's physicians, without a formal psychiatric examination. Psychiatric drug prescription was found to be associated with referral to the CLP, and such correlation involved antipsychotic medication. Rates of antidepressant drugs prescribed by center's physicians and psychiatrists were not significantly different as well as benzodiazepine prescription. It seems that physicians tend to refer patients with more severe symptoms requiring treatment with antipsychotic agents. On the other hand, they feel familiar with depressive and anxiety symptoms’ recognition and with antidepressant prescription. Regarding benzodiazepines, their short-term use does not necessarily imply the recognition of a clinical syndrome, but they were rather prescribed for the management of anxiety and insomnia by physicians and psychiatrists.
Regarding referrals to CLP, TBI was the diagnosis strongly associated with referral, whereas patients with orthopedic disorders were less likely to be referred for psychiatric consultation. TBI has been associated with several psychopathological manifestations[2] and thus physicians often refer such patients for a comprehensive evaluation of their mental health state. Patients’ primary diagnosis was found not to be correlated with psychiatric drug administration.
It seems that physicians in this rehabilitation center have a high index of awareness of psychopathological manifestations of their patients. They often referred patients (43.2% of total admissions) to the CLP service of the hospital, and importantly, they felt comfortable with psychiatric drugs prescription in large proportion (27 from 67, 40.3%) of the nonreferred patients. This may mean that practicing physicians in this rehabilitation center are familiar with psychiatric manifestations and easily recognize such symptoms in their patients; moreover, they are familiar with the use of psychiatric drugs. Whether their approach was confirmed by subsequent psychiatric examination is an intriguing question to be addressed by the future research. Perhaps, in the case of this hospital, the educational activity of the well-established CLP service[19] according to the European guidelines for training in CLP,[20] may have facilitated physicians’ awareness of patients’ psychiatric manifestations and their familiarity with drug treatment. This may not be the case of other rehabilitation centers in the same country and elsewhere.
Regarding psychiatric diagnoses, there were differences from other, more rigorous prospective studies. For instance, Meroni et al.[6] reported a rate of 40% of psychiatric disorders in their sample of patients, which is comparable to 38.1% rate (45 out of 118 patients) of the present study, as diagnosed by the CLP service. However, when cases of drug prescription by the center's physicians encountered (n = 17 patients received antidepressant or antipsychotic drug regimen who presumably had a psychiatric disorder), a total of 62 patients (52.5%) appears to suffer from psychiatric syndrome. This rate is higher than that reported in Meroni et al. study[6] and may be explained when differences in time of assessment and exclusion criteria are taken into account. In their study, patients were evaluated on admission, whereas in the present study, the assessment of the patients could be held at any time during their stay, according to symptom development. Thus, patients who might develop a psychiatric syndrome during their stay in the center would be traced in the sample of the present study. Moreover, Meroni et al. study[6 reported that patients with cognitive impairment were excluded but not in the present study, thus increasing the rates of psychopathology of the sample. In fact, in the present study, there were only a few exclusion criteria, so as to include nearly all patients encountered in usual clinical practice.
Recently, Hammond et al.[15] performed a detailed multicenter study on the use of any psychotropic medication (comprising narcotic analgesics, anticonvulsants, and anti-Parkinson drugs, as well as psychiatric drugs) during inpatient rehabilitation for TBI. The broad definition of “psychotropic” medication and the difference in the sample of patients (only TBI patients in their sample) would make any comparison with the findings of the present study inapplicable.
This study has some limitations. It was designed as a retrospective medical records’ review and thus some information may have been missed. An important question that is whether physicians’ assessments of patients’ psychopathology were accurate cannot be addressed but only in a study with prospective, blind design in which all patients would be assessed independently with the use of a structured clinical interview. Moreover, it is not known whether a proportion of nonreferred and nontreated with psychiatric drugs patients were actually clinical cases that went unrecognized by physicians. On the other hand, the retrospective design of the study ensured that the study procedures were not interfered with the ward's routine. The sample was sufficient and the collected information corresponds to routine clinical practice that is based on usual clinical assessments without regular use of structured instruments. Although some information on patients’ psychopathology may have been missed, this study reported on the everyday approach of patients’ psychiatric manifestations in a tertiary rehabilitation center.
CONCLUSIONS
In the mentioned rehabilitation center, psychiatric drug administration is a common practice, and drugs may be prescribed by the center's physicians and by psychiatrists. Such a drug prescription was found to be correlated to referral to the CLP. Patients suffering a TBI were more likely to be referred for psychiatric consultation. These results may be informative for clinical practice and may raise awareness of psychiatric drug prescription in rehabilitation centers.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- A longitudinal study of major and minor depression following traumatic brain injury. Arch Phys Med Rehabil. 2012;93:1343-9.
- [Google Scholar]
- Depression following adult, non-penetrating traumatic brain injury: A meta-analysis examining methodological variables and sample characteristics. Neurosci Biobehav Rev. 2014;47:1-5.
- [Google Scholar]
- Depression after minor stroke: Prevalence and predictors. J Psychosom Res. 2015;79:143-7.
- [Google Scholar]
- Predictors of anxiety after stroke: A systematic review of observational studies. J Stroke Cerebrovasc Dis. 2015;24:1107-17.
- [Google Scholar]
- Part I: Frequency of depression after stroke: An updated systematic review and meta-analysis of observational studies. Int J Stroke. 2014;9:1017-25.
- [Google Scholar]
- Psychiatric disorders in patients suffering from an acute cerebrovascular accident or traumatic injury, and their effects on rehabilitation: An observational study. Eur J Phys Rehabil Med. 2013;49:31-9.
- [Google Scholar]
- Developing an algorithm capable of discriminating depressed mood in people with spinal cord injury. Spinal Cord. 2014;52:413-6.
- [Google Scholar]
- Prospective study of the occurrence of psychological disorders and comorbidities after spinal cord injury. Arch Phys Med Rehabil. 2015;96:1426-34.
- [Google Scholar]
- Prevalence of depression after spinal cord injury: A meta-analysis. Arch Phys Med Rehabil. 2015;96:133-40.
- [Google Scholar]
- Association of depressive symptoms with functional outcome after traumatic brain injury. J Head Trauma Rehabil. 2012;27:87-98.
- [Google Scholar]
- The association between the severity of poststroke depression and clinical outcomes after first-onset stroke in Korean patients. Gen Hosp Psychiatry. 2015;37:245-50.
- [Google Scholar]
- Treatment for depression after traumatic brain injury: A systematic review. J Neurotrauma. 2009;26:2383-402.
- [Google Scholar]
- Role of sertraline in posttraumatic brain injury depression and quality-of-life in TBI. Asian J Neurosurg. 2014;9:182-8.
- [Google Scholar]
- A comparative study of medication use after stroke in four countries. Clin Neurol Neurosurg. 2016;148:96-104.
- [Google Scholar]
- Psychotropic medication use during inpatient rehabilitation for traumatic brain injury. Arch Phys Med Rehabil. 2015;96:S256-3.e14.
- [Google Scholar]
- Polypharmacy and the use of medications in inpatients with acquired brain injury during post-acute rehabilitation: A cross-sectional study. Brain Inj. 2016;30:353-62.
- [Google Scholar]
- Poststroke depression: A review emphasizing the role of prophylactic treatment and synergy with treatment for motor recovery. Top Stroke Rehabil. 2013;20:139-50.
- [Google Scholar]
- Mortality and use of psychotropic medication in patients with stroke: A population-wide, register-based study. BMJ Open. 2016;6:e010662.
- [Google Scholar]
- The psychodynamically oriented consultation-liaison psychiatry unit, university of Ioannina, Greece. J Psychosom Res. 2009;66:95-7.
- [Google Scholar]
- European Association of Consultation-Liaison Psychiatry and Psychosomatics Workgroup on Training in Consultation-Liaison. European guidelines for training in consultation-liaison psychiatry and psychosomatics: Report of the EACLPP Workgroup on Training in Consultation-Liaison Psychiatry and Psychosomatics. J Psychosom Res. 2007;62:501-9.
- [Google Scholar]






