Translate this page into:
Upper Cervical Bronchogenic Cyst: A Rare Condition at a Rare Location
Address for correspondence: Dr. Chandrasekhar E. Deopujari, Department of Neurosurgery, Bombay Hospital and Medical Research Centre, 12, New Marine Lines, Room No. 126B, Mumbai - 400 020, Maharashtra, India. E-mail: d.chandrashekhar11@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Intraspinal bronchogenic cyst (SBC) is a rare but important cause of spinal cord compression, commonly seen in the cervicothoracic spine. We report a case of a 43-year-old male, presenting with complaints of neck pain, radiating to right shoulder, with numbness of right hand and fingers. Magnetic resonance imaging of the cervical spine revealed an intradural extramedullary, ventral cystic lesion extending from C2 to C4 vertebral levels. Complete surgical excision was performed, and the patient had a complete relief of symptoms postoperatively. Only 11 cases of SBCs have been reported in literature. We discuss the peculiar location of this lesion, possible embryological reasons and the overall surgical outcome of SBC.
Keywords
Bronchogenic cyst
embryology
extramedullary
intradural
neurenteric cyst
upper cervical
INTRODUCTION
Spinal cystic mass lesions are extremely rare. Neurenteric cyst is a rare cause of space-occupying lesion in the spinal canal, accounting for approximately 0.5% of cases of cystic intraspinal lesions.[1] Spinal bronchogenic cysts (SBCs) are benign and are a subtype of neurenteric cysts.[23] They arise due to embryological abnormalities of the developing foregut, with three main theories hypothesizing the exact origin of SBC. Therefore, these cysts are also called as foregut cysts or enterogenous cysts. Hence, bronchogenic cysts are commonly seen in posterior mediastinum, and atypical locations include pericardium, sternum, skin, and spinal cord.[4] The most common location of SBC in the spine is the lower cervical and upper thoracic segment.[35] SBCs are usually intradural, extramedullary in location. Compression of the spinal nerve root, anterior spinal artery, and/or the spinal cord by the cyst can cause features such as radiculopathy, myelopathy, or radiculomyelopathy. Interestingly, acute onset paraplegia has also been described in a case of T5–6 vertebral level SBC.[6] Surgical excision of the SBC is the treatment of choice. Good neurological recovery following surgery has been reported in literature. Histological examination of the cyst is necessary for the confirmation of the diagnosis. A lining of pseudostratified ciliated columnar epithelium resembling respiratory epithelium is the diagnostic hallmark of SBC. Rarely, malignant transformation of these cysts has been described in the mediastinal bronchogenic cysts but not in the spine.[7] As per a recent review, only 11 cases of SBC have been reported in literature.[8]
We describe a rare case of upper cervical SBC and discuss the pertinent literature with an emphasis on the embryological origin. To the best of our knowledge, no case of upper cervical bronchogenic cyst has been reported in literature.
CASE REPORT
A 43-year-old male presented with complaints of insidious onset, gradually progressive neck pain radiating to the right shoulder for 4 months with tingling in the right upper limb, involving all fingers without any associated trauma or infection. No other associated symptoms were present. His neurological examination was normal. Magnetic resonance imaging (MRI) of cervical spine with contrast and whole spine screening was performed which revealed ventral cystic mass measuring about 2 cm × 2 cm extending from C2 to C4 vertebral levels. The mass was located in the intradural, extramedullary compartment without any communication or contrast enhancement [Figures 1 and 2]. The patient underwent a C2 to C4 laminectomy. The dura was opened longitudinally in midline with a “T-cut” on the right side to enable access to the lesion. Intraoperatively, lesion was seen as a thin-walled cystic lesion containing clear viscous fluid. Complete excision of the adherent cyst wall was performed. Dura was closed in watertight manner and wound closed in layers. Postoperatively, the patient had complete relief of his symptoms. Histopathological examination of the specimen showed cystic cavity lined by ciliated columnar epithelium; few subepithelial mucous glands were also seen, suggestive of bronchogenic cyst [Figure 3]. Postoperative MRI performed 1 year after surgery showed no recurrence [Figure 4]. The patient was completely asymptomatic at the time of his follow-up.

- Sagittal section magnetic resonance imaging image showing cystic lesion, extending from C2 to C3 level, anterior to the cord. Lesion is hypointense on T1-weighted images and hyperintense on T2-weighted images
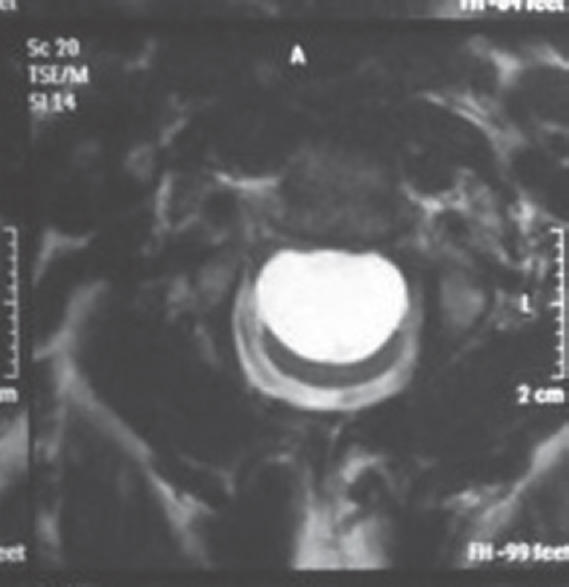
- Axial section of T2-weighted image of magnetic resonance imaging showing hyperintense cystic lesion, lying anterior to the cord
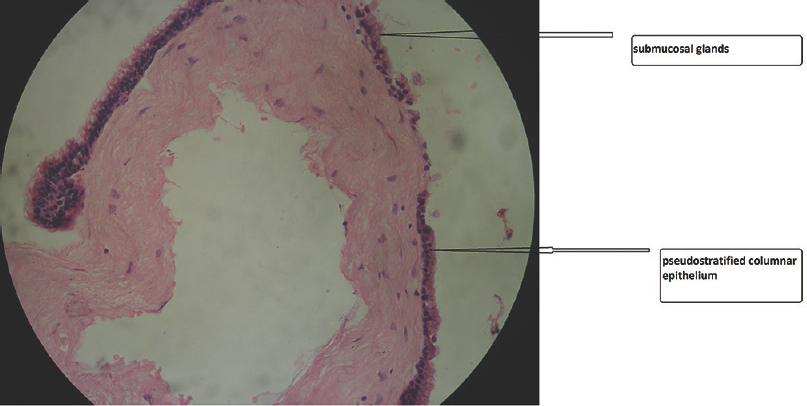
- Histopathology slide showing pseudostratified columnar epithelium lined cystic cavity with few submucosal glands, suggestive of bronchogenic cyst
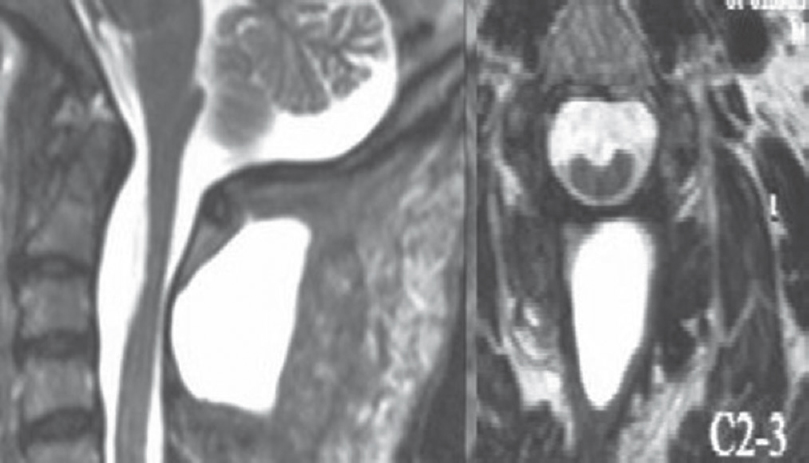
- Postoperative images in axial and sagittal sections of T2-weighted magnetic resonance imaging showing complete excision of the lesion, cerebrospinal fluid accumulation is seen in the intramuscular plane, posterior to the cord
DISCUSSION
SBC is an extremely rare condition and only few cases of SBCs have been published in literature.[8]
It is a developmental anomaly which occurs during embryogenesis and there are various theories regarding the pathogenesis of this entity. As per the first theory, this condition occurs due to persistent adhesion of ectoderm and endoderm while as per the second theory, the cyst is of ectodermal origin, where the ectoderm has the potential to differentiate into endoderm and paraxial mesoderm. The third theory is known as Bentley and Smith's split notochord theory.[9] As per this theory, incomplete duplication and separation of the notochord leads to the formation of a fistula between the yolk sac and the amniotic cavity, which persists during the embryological development. This fistula divides the future spine and spinal cord. Eventually, this fistula closes with a persistence of a ventrally placed ectopic cyst. This theory correctly explains the presence of vertebral body anomalies and predominant ventral location seen in cases of neurenteric cysts. These cysts are therefore most commonly seen in the cervicothoracic region and in the thoracic spine since the cranial end of the notochord develops first and is prone to embryological anomalies at this time. Hence, SBC has not been reported above C3 vertebral level.[810] Thus, the current case is the first reported instance of upper cervical SBC. Not surprisingly, in this case, no vertebral anomalies such as hemivertebra, spina bifida, or fusion anomalies of the vertebra were noted in view of the rare upper cervical spine location of the cyst. This makes the present case unique from an embryological perspective. Thus, this paper gives more credence to the first and the second theory of SBC rather than the split notochord theory. Interestingly, dorsal location of SBC with relation to spinal cord has also been described in literature which would again support the first or second theory more than the split cord theory.[11] Some papers have also described the presence of fat in the cyst wall which would again favor the second theory of ectodermal origin where differentiation into fat, respiratory epithelium is possible.[8] Cysts located at the level of lumbar spine are more likely associated with spinal deformities such as spina bifida and tethering of the cord unlike the ones located at the cervical and thoracic level.[12] Therefore, a common embryological anomaly causing both cord tethering and lumbar SBC has also been proposed.[13] Thus, based on these studies, it is reasonable to hypothesize that SBC may have a multicausal embryological origin which may be dependent on the location of the SBC in the spine. Future studies should be able to provide more clarification on the exact embryological origin of SBC.
Cystic lesions of the spine usually become symptomatic after secondary changes such as infection, rupture, increase in size, or after trauma to the spine. However, in the present case, there were no secondary changes in the cyst. Typically, SBCs are extremely slow growing due to the presence of tight junction in the epithelium. Thus, it is important to emphasize that SBC may become symptomatic by gradual increase in size of the cyst causing pressure symptoms on the surrounding neural structures. This fact is also corroborated in the review by Ma et al. who noted that none of the patients had a secondary change in the SBC at the time of the presentation.[8]
MRI is the diagnostic modality of choice to delineate the lesion from the overlying soft tissue and relationship of the SBC to the cord. The most commonly seen characteristics on MRI is the presence of T1-hypointensity and T2-hyperintensity, without contrast enhancement. In contrast to a recent paper, where lipomatous tissue was noted in the cyst wall in some cases, no such fat was noted in our case.[8] Surgical excision is the treatment modality of choice; however, complete excision is not always possible due to adherence of the cyst wall to the cord. Hence, only in 4/11 of the published cases, the cyst could be completely resected.[8] Therefore, patients need to be counselled regarding the need for a long-term radiological follow-up to detect recurrence.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Enterogenous cysts and congenital diverticula of the alimentary canal with abnormalities of the vertebral column and spinal cord. J Pathol Bacteriol. 1959;77:457-71.
- [Google Scholar]
- Cysts of the central nervous system: A clinicopathologic study of 145 cases. Neurol India. 2001;49:237-42.
- [Google Scholar]
- Thoracolumbar intradural extramedullary bronchiogenic cyst. Acta Neurochir (Wien). 2005;147:317-9.
- [Google Scholar]
- An acute case of paraplegia and spinal bronchogenic cyst. J Orthop Sci. 2015;20:923-6.
- [Google Scholar]
- Malignant transformation of bronchogenic cyst revealed by 99mTc-MIBI-SPECT. Asian Cardiovasc Thorac Ann. 2012;20:347-9.
- [Google Scholar]
- Intraspinal bronchogenic cyst: Series of case reports and literature review. J Spinal Cord Med. 2017;40:141-6.
- [Google Scholar]
- Developmental posterior enteric remnants and spinal malformations: The split notochord syndrome. Arch Dis Child. 1960;35:76-86.
- [Google Scholar]
- Bronchogenic intraspinal cyst – A rare case of spinal cystic space occupying lesion. Neurol India. 2016;64:1083-4.
- [Google Scholar]
- Thoracic myelopathy secondary to intradural extramedullary bronchogenic cyst. J Spinal Cord Med. 2009;32:595-7.
- [Google Scholar]
- Bronchogenic cyst of the conus medullaris with spinal cord tethering: A case report and review of the literature. Int J Clin Exp Pathol. 2015;8:3937-42.
- [Google Scholar]






