Translate this page into:
Caregiver's Psychosocial Concerns and Psychological Distress in Emergency and Trauma Care Setting
Address for correspondence: Dr. T. R. Kanmani, Department of Psychiatric Social Work, National Institute of Mental Health and Neurosciences, Bengaluru, Karnataka, India. E-mail: kanmani.raju@gmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Traumatic brain injury (TBI) will be the third largest killer by the year 2020 in the world. It creates the great amount of morbidity, disability, mortality, and reduces the psychosocial well-being of the patients and their caregivers. Hence, the current paper aimed to explore the psychosocial distress and caregivers’ concerns in emergency and trauma care (ETC) setting.
Methodology:
This study adopted qualitative research design. All caregivers of TBI survivors were considered as a universe of the study. A total of 50 caregivers were recruited, and the predesigned questionnaire was administered. Depression, anxiety, stress scale was used to identify the caregivers’ depression, stress, and anxiety. The simple thematic analysis was used to derive the themes from the verbatim data. Data were analyzed using SPSS version 21.0 (SPSS South Asia Pvt. Ltd, Bengaluru, Karnataka, India).
Results:
In the quantitative analysis, caregivers’ mean age was found to be 45 (mean = 45.00 ± 13.83) years. Caregivers had experienced mild depression (13.36 ± 3.07), moderate anxiety (13.70 ± 3.03), and minimum stress (13.66 ± 2.98) levels. Qualitative results identified the following themes: difficulty in accessing timely care, uncertainty about the prognosis and future, family concerns and financial constraints, personal feelings and personal needs, and supportive care. Chi-square test revealed that there was no significant association between gender and depression (χ2 = 2.381 P < 0.12), anxiety (χ2 = 0.01 P < 0.92), and stress (χ2 = 0.235 P < 0.61) levels of caregivers.
Conclusion:
To accomplish, providing psychosocial care in ETC setting, the role of psychiatric social workers is pivotal.
Keywords
Caregiver
distress
psychosocial concerns
INTRODUCTION
Road traffic accidents (RTA) are the public health issue.[1] Traumatic brain injury (TBI) creates emergency situation at any point of time and patients may approach to the hospital for emergency management. When they reach the hospital caregivers may able to remember the previous period of admission, time, day, and month, and if it is direct visit, they have to prepare themselves to give the right information for the immediate medical attention.[2] The emergency setting has multiple challenges, and caregivers face unfamiliar environment. In India, caregiving is left to the family members.[3] In the process, caregivers experience physical, emotional, psychological problems, caregiver burden, dissatisfaction, and psychosocial needs are unmet during hospitalization after TBI.[45] Crisis, stress and coping, and communication theories are commonly used in addressing the psychosocial problems of caregivers of TBI survivors.[67] To meet the caregivers’ psychosocial problems, the role of medical and psychiatric social workers (MPSWs) in emergency and trauma care center is emphasized in the clinical practice.[8] Quantitative and qualitative publications on TBI research are low, and little attention was given to explore the in-depth caregivers experiences mental health, psychosocial issues in emergency, trauma care (ETC)setting.[9] Therefore, the current study aimed to understand the psychological distress, psychosocial concerns of caregivers of persons with TBI in ETC setting.
METHODOLOGY
The study adopted mixed methodology research design. Mixed method is the intentional integration or combination of the two methods, that is quantitative and qualitative, to draw on the strengths of each to answer real-life research questions.[1011]
Adult male and female caregivers providing care for persons with TBI in ETC setting, The National Institute of Mental Health and Neurosciences (NIMHANS), Bengaluru, had considered as the universe of the study. Fifty (n = 50) samples were recruited using convenience sampling technique, and inclusion and exclusion criteria were followed. All adult caregivers, who were providing care for persons with TBI and who could speak English and Kannada, were recruited in the study. Caregivers who were not willing to give written informed consent and reported to have major medical and psychiatric disorders were excluded from the study.
Data had been collected during hospitalization. The participants were informed orally about the aim and purpose of the study. Information sheet also handed over to each participant. Predesigned data tools were administered in a face-to-face interview in a separate room over 6 months from August to November 2016. Data were collected in two phases.
In the first phase, sociodemographic details such as caregiver's age, marital status, domicile, education, and occupation were collected. In addition, to identify the presence of psychological distress (depression, anxiety, and stress) among caregivers, depression anxiety and stress scale (DASS-21, Lovibond and Lovibond, 1995) were administered to recruited participants. DASS is a set of three-domain self-report scale designed to measure the significant negative emotional states of depression, anxiety, and stress. Each domain (depression, anxiety, and stress) contains seven items divided into subscales of 2–5 items with similar content. The severity is measured on 0–3; 0 – did not apply to me at all, 1 – a good part of the time, 2 – applied to me to some degree or sometimes, and 3 – applied to me very much or most of the time. The scale was widely used in the Indian context. Each interview lasted between 30 and 45 min.
In the second phase, seven focused group discussions (FGDs) were organized in a systematic manner based on predesigned FGD interview guidelines. FGD is a good way to gather people from similar backgrounds or experiences to discuss on specific objective. FGD can be used to explore the meanings of a particular participant which cannot be explained statistically.[12] In the present study, FGDs were conducted to explore the psychosocial concerns of caregivers in trauma care setting. In the process, caregivers were invited to participate in FGDs after obtaining oral and informed consent. Seven FGDs were conducted on weekly basis. In each FGD, 7–10 caregivers were participated during hospitalization. FGDs were guided by predesigned open-ended questions based on the objective of the study. For example, how did you feel when you heard your relative's accident? What were the difficulties that you faced to get trauma care treatment after the accident? What made you feel more worried during hospitalization? What were your concerns with respect to the patient/family members and yourself? Closed and leading questions were used appropriately to bring the context to understand the person in the situation. FGDs were conducted by trained professional psychiatric social workers (PSWs) from NIMHANS, who had mental health work experience in trauma care setting. FGD participants’ verbatim responses and interaction pattern within the groups were manually recorded in the summary form immediately after FGDs by PSWs.
Data analysis
For quantitative continuous data, mean (standard deviation) for categorical variables percentage was calculated. Chi-square test was computed to find the association between gender and the subdomains of DASS, i.e., depression, anxiety, and stress.
For qualitative data analysis, the simple descriptive thematic analysis was used. In the process, the vernacular verbatim interview summaries (Kannada) were transcribed and translated into English. All transcriptions were read a number of times to achieve an understanding of the data as a whole and then coded. Following which, repeated words or phrases were coded, relevant codes were collated, and then, themes were generated. Data were triangulated with clinical observations, daily notes, and memos. The data saturation was ensured. Institute Ethical Clearance was obtained.
RESULTS
Data results showed male (72%) and female caregivers (28%) participated in the study, respectively. Of which, son or daughter (44%), brother or sister (28%), spouse (16%), father or mother (8%), and in-laws were (4%) took the caregiving responsibility during hospital stay at trauma care center. Majority of the caregivers studied up to secondary education (62%), belong to Hindu religion (70%), hailing from the rural background (60%). Table 1 explains the sociodemographic details of caregivers.
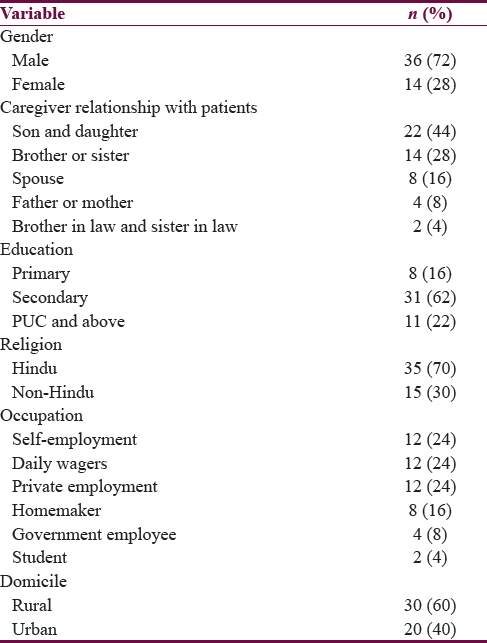
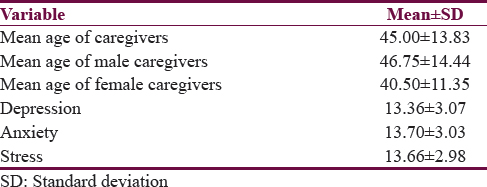
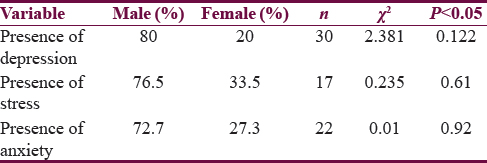
Table 2 shows age and depression, anxiety, and stress levels of caregivers. Descriptive results (mean and standard deviation) revealed caregivers’ mean age was 45 (mean = 45.00 ± 13.83) years. Among them, male caregivers’ average age was 46 (46.75 ± 14.44) years whereas female caregivers average age was 40 (40.50 ± 11.35) years. Results also indicated that caregivers experienced mild depression (13.36 ± 3.07), moderate anxiety (13.70 ± 3.03), and minimal stress (13.66 ± 2.98). Table 3 shows the association between caregiver gender and caregivers’ depression, anxiety, and stress. Chi-square test revealed that there was no significant association between gender and depression (χ2 = 2.381 P < 0.12), anxiety (χ2 = 0.01 P < 0.92), and stress (χ2 = 0.235 P < 0.61) between caregivers.
Qualitative results
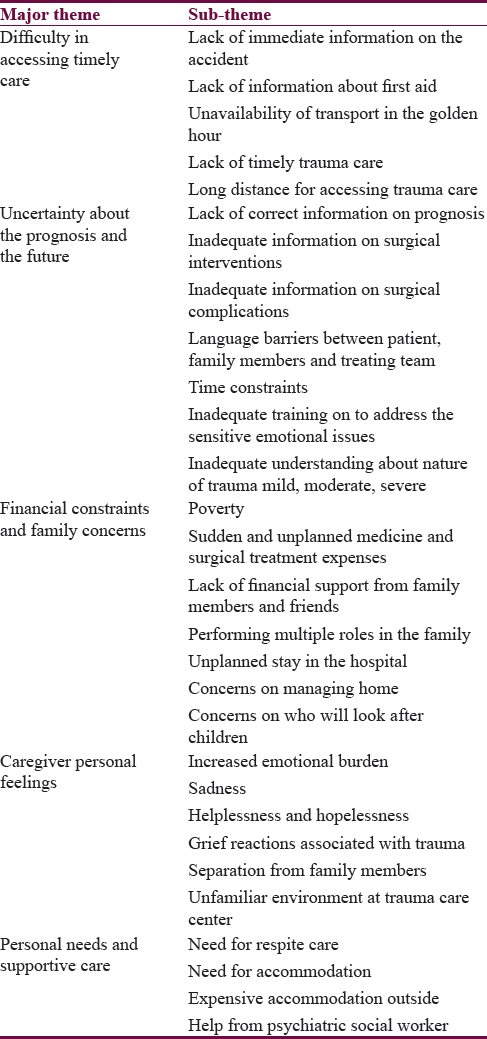
The following themes were derived from the FGD.
Difficulty in accessing timely trauma care
Most of the caregivers had expressed immediate information on the accident and first-aid services for the TBI survivor was challenging. Emergency services, such as the accessibility of ambulance soon after the accident, were still far from reach during golden hour. For the immediate medical help or surgical intervention, they need to travel a long distance. This is evident from the following illustration;
“My husband sells milk in villages while crossing the road he was hit by four-wheeler. We heard the accident news and rushed to the spot. It took more than 2 h to reach the accident place since it had happened in the remote rural area. After that, we made several calls to 108 ambulances it reached after an hour. We went to the local hospital where only first aid was provided and they referred to tertiary trauma care center for further care” (Group 1- Participant 5).
Uncertainty on prognosis and traumatic brain injury survivors’ future
In the emergency setting, the environment is always unfamiliar, uncertain, and transition takes place quickly. The uncertainty was related to the prognosis, and surgical complications were inadequate. The possible reasons were language barriers and time constraints, and many health-care professionals were not specialized in addressing emotional issues in the acute phase. Most of the time, caregivers were apprehensive and unaware of the condition of their kith and kin admitted in the emergency room including treatment and outcome. One of the participants said that;
“Treating team did inform me about patient condition, but I do not know about the condition of the patient and future since I did not understand completely due to language barrier.” (Group 2-Participant 2).
Financial constraints and family concerns
Majority of the caregivers and their TBI survivors were from below poverty line (BPL). The sudden accident and treatment cost had increased financial burden. The existing social support system could not extend financial support during the crisis. Negative life events, such as RTA had increased caregiver burden, perform multiple roles such as managing home, children, and hospital stay.
This was evident from the following;
“After the accident, we are undergoing financial crisis and also had difficulty to manage home. I had spent almost more than a lakh, we borrowed money from known relatives for interest, now they also withdrew” (Group 4- Participant 1).
Personal feelings
Caregivers were emotionally disturbed; cry, sadness, helplessness, and hopelessness were observed among caregivers. Emergency environment, TBI survivor condition after the accident, separation from children, and elderly people at home were persistent concerns. One of the participants said that;
“He is the only son for us. His engagement had taken place one month back. We do not know what is going to happen…to my son's life…… (cried….)” (Group 3-Participant 6).
Personal needs and supportive care
Caregivers expressed the need for the alternative care-to-care themselves. The existing rest homes provided by hospital authority within hospital premises were always full, lodges were expensive and unaffordable outside. Further, they added that periodical counseling services, timely information about the patient condition by mental health professionals such as PSWs would be of help during the hospital stay at emergency and trauma care center.
The participant expressed “I do not have adequate sleep since last one week. I am the only person looking after my wife. I do not have any support from my relatives” (Group 5-participant 7).
Another participant reported that “My counsellor (Psychiatric Social worker) explained about my father's condition since then I know what is happening to my father in every day. I do not know what is happening to my father till I met him (PSW). Counsellor services helped to reduce my worries a lot in my case” (Group 7-Participants 6, 5, 7). Table 4 depicts the major themes and subthemes derived from qualitative data.
DISCUSSION
RTAs are increasing day-by-day due to motorization and industrialization. Caregivers play the major role to meet the day-to-day needs of TBI survivors during hospitalization. Literature review evidence shows caregivers experience a range of psychosocial issues which remain unexplored in India. There is a lack of research in the areas of psychological distress, psychosocial concerns, and caregivers’ experience in ETC setting.[13] In this context, the current study holds the significance. Most of the scientific studies emphasize TBI incidence is high in male population when compared to female. The current findings showed that the majority of the caregivers were male. Existing rules, in our ETC center, permit the same gender as a caregiver for the TBI survivors. For example, for male TBI survivor, male family member as a caregiver; for female TBI survivor, female family member as a caregiver. This would be the reason for having higher number of male caregivers in the study. Caregiving was left to family members in the Indian context.[3] In the current study predominately, son or daughter took the caregiving responsibility. Besides that brothers’, sisters’, spouse, father/mother, and bother/sisters-in-law were also actively participated in performing the caregiving responsibilities in less proportion. Caregiver's average age was 45 years which means they were in more productive and responsible position in the family. Caregivers engaged in different occupations; self-employment such as driving, tailoring, running petty shops; and private employment such as clerk, gardener, office boy, engineer and few go for coolie work for a daily wage. This shows that the loss of work, loss of pay, and sudden treatment expenses had increased economic burden in the family. The other finding was that majority of the caregivers were from rural background. The demographic details are similar in line with the previous studies reported elsewhere.[1415]
Qualitative results showed that accessing timely ETC was difficult to TBI survivors after the accident, especially in rural areas. This finding highlights the need to improve the golden hour care services and the establishment of ETC centers in the rural area. Poor budget allocation, varied topography, and inadequate infrastructure with respect to the management of emergency situation still persist in rural India.[16]
In addition, inadequate information on TBI, uncertainty about the prognosis, and recovery were a serious concern that consistently expressed by caregivers. Studies reveal caregivers and family members experience uncertainty and stress without understanding what is happening around them.[17] Health education services are not rendered up to the mark in many emergency and trauma care centers.[18] This finding highlights the need for caregiver/family education for TBI survivors and their family members.
The study findings showed that managing treatment expenses for TBI survivor in the emergency period was difficult to the caregivers in spite of concession received for surgical interventions under BPL category and minimal financial support received from family members. Only two individuals utilized the health insurance to meet the treatment expenses. Studies depict that maintaining health expenditure in the absence of health insurance increase the economic burden of caregivers to the families and community.[1920] This warrants research on awareness on health insurance in rural communities, economic burden, and utilization of health insurance schemes in general and in particular among families with TBI survivors.
The present study findings revealed crying, stress, anxiety, depression, helplessness, hopelessness, lack of social support, unmet psychosocial needs, need for respite care, and professional support for caregivers in the emergency and trauma care. Sudden accident, emergency center environment, severity of trauma, being away from young children, spouse, disruption in family routine activities, and lack of support from family members might have contributed to experience emotional distress. Quantitative results showed that there was mild depression, moderate anxiety, and minimal stress was experienced by caregivers. In ETC setting, caregivers generally experience high levels of emotional and psychological distress.[221]
Caregivers also expressed that need for counseling and psychosocial interventions were helpful to reduce their emotional and psychological stress, facilitate to access timely care, and up-to-date information on prognosis and recovery. This finding emphasizes the importance of the MPSWs’ therapeutic interventions in the emergency and trauma care unit.[81822] Review also reported that psychosocial interventions are recommended for TBI survivor and caregivers in ETC setting.[18]
Clinical implications
MPSWs work with TBI survivors, caregivers, and family members to understand the needs, knowledge, and psychological impact on physical health, psychosocial well-being, and mental health problems. It is observed that regular counseling services and psychosocial interventions are found to be useful regarding informational, psychoeducational, financial, emotional, physical, psychosocial healthcare, and felt needs. MPSWs facilitate medical and psychological information along with treatment care coordination. In ETC, the emphasis is predominantly on enhancing coping on medical condition, treatment procedure, surgical process, recovery, discharge, treatment adherence, and follow-up. Thus, the inclusion of MPSWs and mental health professionals would yield the fruitful results in providing better psychosocial care. However, psychosocial interventions need to be tested in stringent experimental conditions.
Limitations of the study
The study participants were heterogeneous from different socioeconomic backgrounds. The study did not actively screen grief reactions which might have the potential impact on caregivers’ distress and unidentified psychopathology. The study did not provide structured psychosocial interventions to meet the psychological distress of caregivers. Therefore, the generalization of the study findings is cautioned to other settings.
CONCLUSION
Caregivers experience psychological distress, want for informational and educational support. There is a paucity of trained professionals to deal with mental health issues and less time to address high expectations of patients and their family members on prognosis and recovery in ETC setting. Hence, we suggest that psychosocial care regarding crisis intervention, distress management, systematic information, education, family communication, and supportive therapy are imperative in ETC setting. The above psychosocial interventions can be provided with the help of posters, pictorial diagrams, and audio-video material specially designed on the impact of TBI in vernacular language for family education purpose. This would allow literate and illiterate caregivers to understand the basics of anatomy of the brain, functions of the brain, difference between head injury and TBI, how TBI impacts individuals and families, need for emergency treatment, possible side effects, recovery process, long-term impact and importance of caregiver role, and family support for the TBI survivor. However, this information, communication, and education materials should be carefully designed and developed with the help of experts who have handhold work experience in ETC setting such as MPSWs, neurosurgeons, anesthesiologist, mental health educators, psychologist, and psychiatrist. To conclude, the placement of MPSW on 24 × 7 basis in ETC setting is the need of the hour in developing countries like India to address the mental health issues.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Outcome measures for traumatic brain injury. Clin Neurol Neurosurg. 2011;113:435-41.
- [Google Scholar]
- Patient expectations and the paradigm shift of care in emergency medicine. J Emerg Trauma Shock. 2011;4:163-7.
- [Google Scholar]
- Caring for the family caregivers. 2016. Indian J Soc Psychiatry. 32:1. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4181176/
- [Google Scholar]
- Historical and theoretical overview. Crisis Interv Crim Justice social Serv. 2002;3:3-31.
- [Google Scholar]
- Providing effective trauma care: The potential for service provider views to enhance the quality of care (qualitative study nested within a multicentre longitudinal quantitative study) BMJ Open. 2014;4:e005668.
- [Google Scholar]
- Experiences of care: Perspectives of carers of adults with traumatic brain injury. Int J Speech Lang Pathol. 2011;13:218-26.
- [Google Scholar]
- Quantitative research on traumatic brain injury in India: The travails and the new optimism. Neurol India. 2017;65:261-2.
- [Google Scholar]
- Clinically providing psycho-social care for caregivers in emergency and trauma care setting: Scope for medical and psychiatric social workers. Int J Crit Illn Inj Sci. 2016;6:206-10.
- [Google Scholar]
- A systematic review of quantitative research on traumatic brain injury in India. Neurol India. 2017;65:305-14.
- [Google Scholar]
- Application of mixed method approach in public health research. Indian J Community Med. 2016;41:93-7.
- [Google Scholar]
- Patient safety and job-related stress: A focus group study. Intensive Crit Care Nurs. 2008;24:90-7.
- [Google Scholar]
- Caregiver functioning following early childhood TBI: Do moms and dads respond differently? Neuro Rehabilitation. 2010;27:63-72.
- [Google Scholar]
- Traumatic brain injury: Does gender influence outcomes? Int J Crit Illn Inj Sci. 2016;6:70-3.
- [Google Scholar]
- Epidemiological study of ocular trauma in an urban slum population in Delhi, India. Indian J Ophthalmol. 2008;56:313-6.
- [Google Scholar]
- Family stressors in traumatic brain injury: A two-year follow-up. Arch Phys Med Rehabil. 1994;75:876-84.
- [Google Scholar]
- Addressing the growing burden of trauma and injury in low- and middle-income countries. Am J Public Health. 2005;95:13-7.
- [Google Scholar]
- Epidemiology of traumatic brain injuries: Indian scenario. Neurol Res. 2002;24:24-8.
- [Google Scholar]
- 2016. Awareness, coverage, practices and prospects for health insurance in the union territory of Chandigarh. Man & Development: March. Available from: https://www.researchgate.net/publication/303738596
- Medical social worker: Strengthening linkages between the hospital and the community. 2014. Int J Health Syst Disaster Manag. 2:130. Available from: http://www.ijhsdm.org
- [Google Scholar]






