Translate this page into:
Ventriculoperitoneal Shunt Disconnection, Shunt Migration, and Silent Bowel Perforation in a 10-Year-Old Boy
Address for correspondence: Dr. Rajendra Kumar Ghritlaharey, Department of Pediatric Surgery, Gandhi Medical College and Associated, Kamla Nehru and Hamidia Hospitals, Bhopal - 462 001, Madhya Pradesh, India. E-mail: drrajendrak1@rediffmail.com
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Wolters Kluwer - Medknow and was migrated to Scientific Scholar after the change of Publisher.
Abstract
A 10-year-old boy was admitted with chest wall infection around the implanted ventriculoperitoneal shunt (VPS) catheter of 5 days. He had received a right-sided, medium pressure, whole-length VPS for hydrocephalus, following tubercular meningitis at the age of 3 years. Seven years, 9 months following VPS implantation, he was admitted with shunt tract infection at the chest area for 5 days. He had neither fever nor features of meningitis, raised intracranial pressure, or peritonitis. His clinical examination and radiological investigations revealed that the VPS catheter was disconnected at the cranial site, and it was migrated downward up to the upper chest. He was managed well with the removal of the entire VPS catheter. The removed peritoneal catheter along with the shunt chamber was loaded with fecal matter and was presumed that the peritoneal catheter was within the colon. His postoperative recovery was excellent. This is a rare case of VPS catheter disconnection, shunt migration, and silent bowel perforation by peritoneal catheter, and all the above-mentioned complications were detected in a child at the same time and were managed well with the removal of the entire VPS catheter.
Keywords
Hydrocephalus
infection
silent bowel perforation
ventriculoperitoneal shunt
ventriculoperitoneal shunt complication
ventriculoperitoneal shunt disconnection
INTRODUCTION
Ventriculoperitoneal shunt (VPS) insertion for the treatment of hydrocephalus is associated with several complications, including infections, mechanical failure, obstruction, bowel perforation with or without extrusion through natural orifices, nonvisceral perforation, shunt migrations, and shunt disconnection.[123] Colon is the most common site for hollow viscus perforation by the peritoneal catheter, but perforation of the small bowel, stomach, and other hollow viscus has also been reported.[1345] Disconnection of VPS catheter is also a well-known complication and is observed more in multicomponent shunt systems.[67] This present case is a report of VPS catheter disconnection, downward shunt migration, and silent bowel perforation by peritoneal catheter occurred in a child at the same time.
CASE REPORT
A 10-year-old boy was admitted with infected ulcers in the chest wall around the implanted VPS catheter for 5 days [Figure 1]. At the age of 3 years, a right-sided, medium pressure, whole-length VPS (Chhabra slit n spring hydrocephalus shunt system) was implanted for hydrocephalus following tubercular meningitis. Five years, 8 months following VPS implantation, he was admitted with vague abdominal pain for 2 weeks, and malfunctioning of peritoneal part of the VPS catheter was detected. He was managed well with exteriorization of peritoneal part of the VPS catheter and followed by delayed revision of peritoneal part of the VPS catheter. Ten months following revision of the peritoneal catheter, he was admitted with shunt tract infection/redness around the VPS catheter at the chest and abdomen area for 3 days and was managed well with broad-spectrum antibiotics. Seven years, 9 months following VPS implantation (25 months after revision of peritoneal part of the VPS catheter), he was admitted again with shunt tract infection at the chest area for 5 days. He had neither fever nor features of meningitis, raised intracranial pressure, or peritonitis. His clinical examination revealed that there were multiple infected ulcers around the VPS catheter in the chest area. VPS catheter proximal to the chamber was also seen protruding out for few centimeters from the chest wound [Figure 1]. On palpation of the VPS catheter, the part of the shunt from the cranial to the upper chest was missing. Abdominal examination revealed two healed abdominal scars in the right hypochondrium [Figure 1], and the rest of the abdominal examination was normal. Digital anal examination was normal and only loaded fecal matter was noted. Other systemic examination was normal.

- Clinical photograph showing ventriculoperitoneal shunt tract infection, and migrated end of the shunt catheter at the chest area, and healed abdominal scars
Skiagram of the head showed that the ventricular part of the VPS catheter with a connector was seen, and the chamber and the rest of the shunt catheter were not visualized [Figure 2a and b]. Skiagram of the chest and abdomen revealed that the VPS chamber was migrated downward and seen at the upper chest area. This skiagram also revealed that there was coiling of part of the peritoneal catheter in the upper part of the abdominal cavity [Figure 3]. There were no fluid levels or free gas shadow under the diaphragm. Ultrasonography examination of the abdomen revealed that there was no fluid collection within the peritoneal cavity, and peritoneal part of the VPS catheter was seen in the peritoneal cavity. Computed tomography (CT) scan of the head delineated the ventricular catheter with the connector well in place, and the tip of the ventricular catheter was lying at anterior horn of the left lateral ventricle without ventricular dilatation [Figure 4]. The shunt chamber and upper part of the shunt catheter were missing in cranial CT. The VPS catheter was disconnected from the connector that was used to connect the ventricular catheter to the chamber of the VPS catheter and which was also migrated downward. His hemoglobin, total and differential white blood cells counts, platelets counts, urea, creatinine, bilirubin, and electrolytes values were within normal limits.
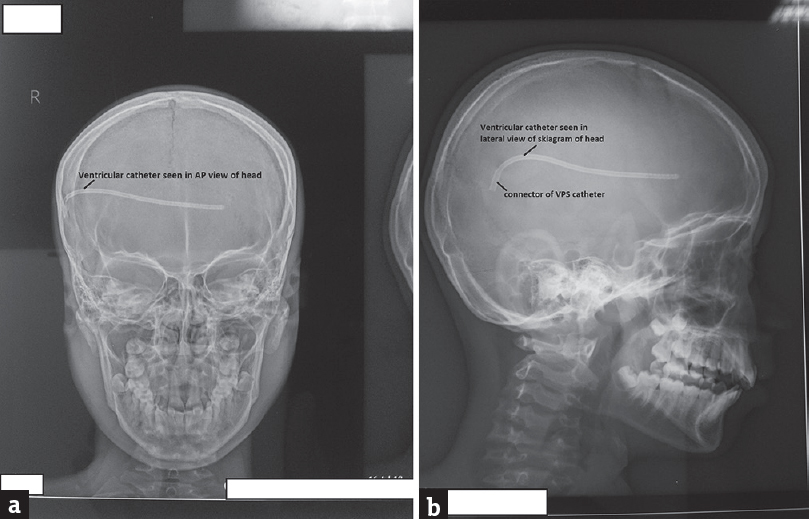
- (a) Skiagram of the head (anteroposterior view) showing ventricular part of the ventriculoperitoneal shunt catheter. (b) Skiagram of the head (lateral view) showing ventricular catheter and connector
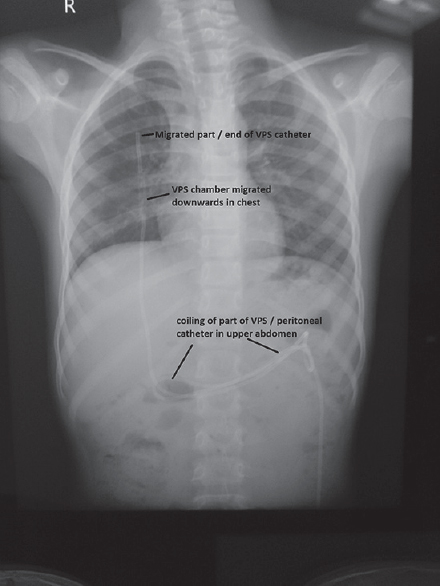
- Skiagram of the chest and abdomen showing migrated ventriculoperitoneal shunt chamber at the upper chest and coiling of the part of peritoneal catheter in the upper abdomen
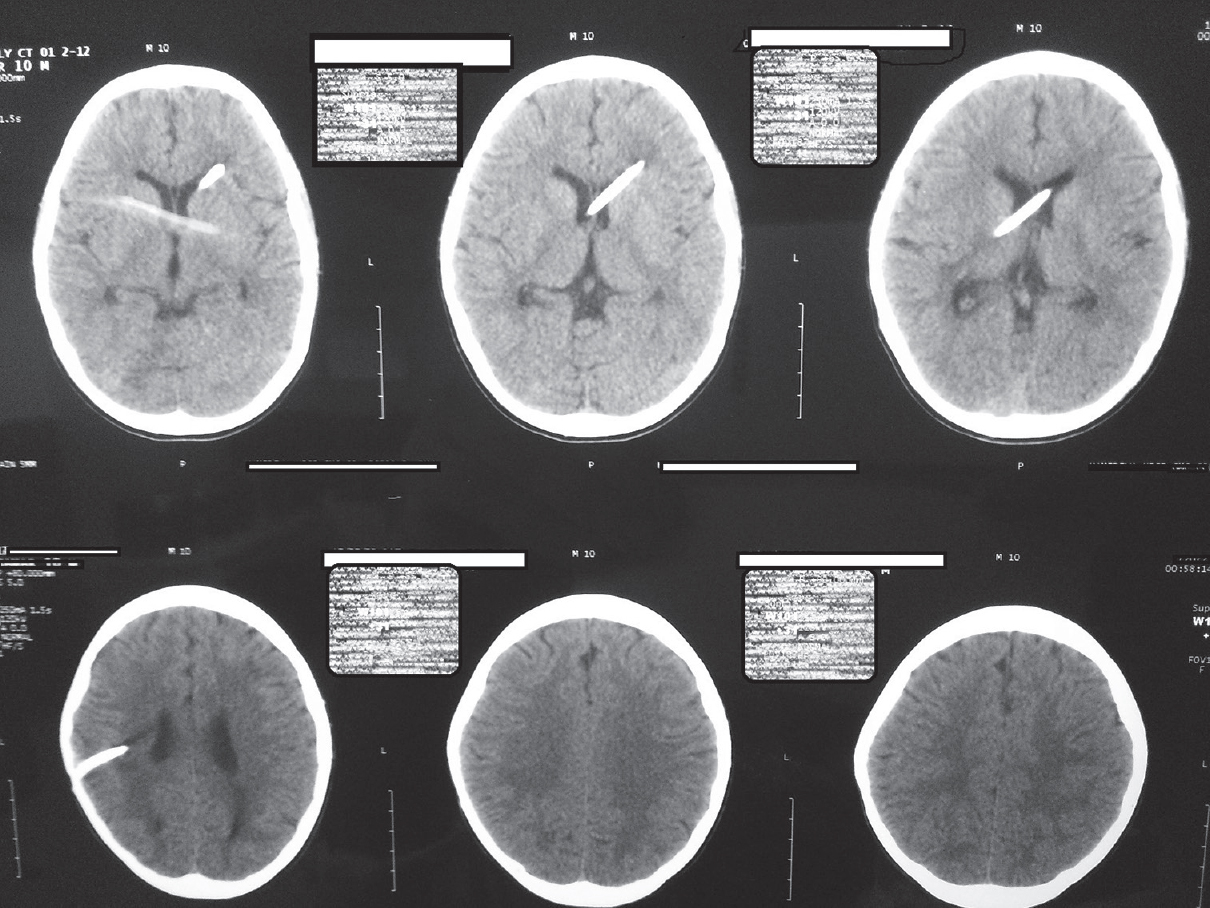
- Computed tomography scan of the head showing ventricular catheter in place and without ventricular dilation
He was managed with the removal of the entire VPS catheter under sedation. The VPS chamber along with the peritoneal catheter was removed easily from the chest area [Figure 5a]. During the removal of the VPS chamber and peritoneal catheter, it was observed that the chamber and the entire peritoneal catheter were loaded with fecal matter, and it was presumed that the peritoneal catheter was within the large bowel [Figure 5b], although digital rectal examination felt to palpate the catheter. The ventricular catheter along with the connector was removed through a separate scalp incision and was removed with some difficulty. During the removal of the ventricular catheter, cerebrospinal fluid (CSF) aspiration was tried but failed, and CSF was also not drained from the old craniotomy site after the removal of the ventricular catheter. The scalp wound was closed primarily. He was kept nil orally for 72 h and was observed for the development of peritonitis. His pus was sent for bacteriological culture, and sensitivity from the chest wound was sterile. He received injectable ceftazidime and tazobactam combination, amikacin, and metronidazole for 10 days. His postoperative period was excellent, and his chest and other wounds also healed well, and he was discharged on the 10th postoperative day. As he was without symptoms and sign of raised intracranial pressure, and his CT scan head also revealed no ventricular dilatations, he was not advised reinsertion of VPS. He lost to follow-up after discharge.
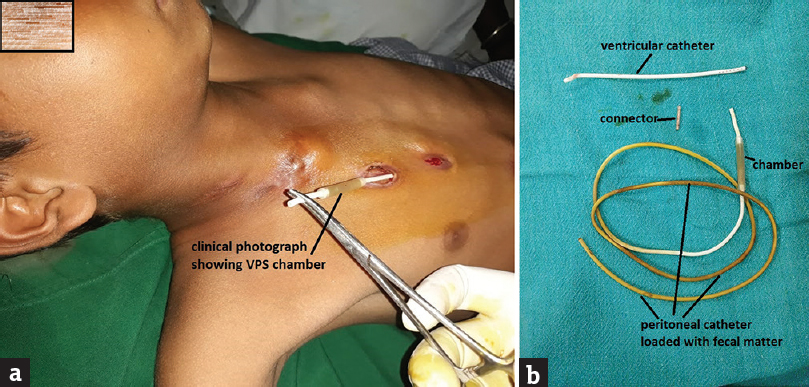
- (a) Ventriculoperitoneal shunt chamber along with the peritoneal catheter was removed by pulling it out from the chest wall wound. (b) Removed ventriculoperitoneal shunt catheter showing fecal matter within the shunt chamber and peritoneal catheter
DISCUSSION
Complications relating to VPS implantation are reported to occur in 24%–47% of the cases. Many of these complications occurring following VPS implantation require shunt revisions, and the requirement of revisions is significantly more in pediatric patients compared to adults.[13] The requirement of shunt revisions varies from 6 months to 20 years after the VPS insertion or last shunt revision.[123] Bowel perforation is also occurring in up to 2% of the cases, and most of the time, the bowel perforation is without peritonitis. Colon is the most common site for hollow viscus perforation by peritoneal catheter, although perforation of the small bowel, stomach, and other hollow viscus has also been reported.[13456] Majority of the cases of bowel perforation and nonenteric hollow viscus perforation by the peritoneal catheter of VPS occurred in children, and most of them presented with extrusion of the peritoneal catheter from the natural orifices.[1345]
Disconnection of the VPS system is also a well-recognized complication following VPS implantation done for hydrocephalus and reported for about 15% of the cases of malfunction of the shunt. VPS disconnection is most frequently observed following the use of multicomponent/multipiece shunt system as compared to one-piece shunt systems.[78] In multisegment VPS systems, the weakest points for shunt disconnection are connector site, connector to ventricular catheter, and connector to chamber site. The causes for shunt disconnection in multisegment VPS system are excessive traction movements at the cranial end, poor fixation at the cranial site, and break in ligatures. VPS disconnection is not always associated with shunt malfunction, and in such cases, the entire VPS system can be safely removed. VPS system disconnection associated with other complications that occurred in the same patient at the same time has also been reported in literature.[910]
In the present case, a multisegment VPS was implanted for hydrocephalus that developed as a complication of tubercular meningitis. He had no symptoms and signs of shunt malfunction/raised intracranial pressure. The part of the catheter just proximal to the chamber, which was connected to the connector and then connected with distal part of the ventricular catheter, was disconnected. The connector was remained connected with the ventricular catheter. During VPS implantation, 3–0 silk was used for securing the connector in place and tied both the ends again for extra security for the connector to the ventricular and peritoneal catheters. The connector was then fixed at appropriate place to the periosteum with absorbable sutures to prevent the shunt migration. In the present child, after disconnection of the shunt, it was migrated downward and was migrated up to the upper part of the chest. Shunt tract infection that occurred in the present case was probably due to the intraluminal, upward migration of fecal matter, fecal spillage, and soiling of the pericatheter space with fecal matter. His skiagram of the chest and abdomen also revealed that there was coiling of the peritoneal catheter, and it is difficult to predict whether that occurred during revision of his peritoneal catheter or afterward. His bowel/colon perforation by peritoneal catheter was detected during shunt removal, as the entire peritoneal catheter along with shunt chamber was filled with fecal matter. He had neither features of peritonitis before the shunt removal nor developed during postoperative period, and therefore, it was managed well without any further surgical intervention. His CT scan head that was done before the shunt removal did not report ventricular dilatation, and he also did not develop any symptoms and signs of raised intracranial pressure during postoperative period, and therefore, reshunt placement was not advised.
The possible reasons for shunt disconnection in the present case may be excessive neck movements, fixation of the connector at the cranial end, growth of the child, weak point at the connector site, ligature break, excessive traction at the abdomen site, and shortening of catheter length due to shunt coiling. The simplest and safest way to prevent/eliminate the shunt disconnection is the use of single/one-piece VPS system.[8]
CONCLUSION
Complications following VPS implantation for hydrocephalus are more frequently observed during the first 12 months, but late complications are also serious and therefore needing long-term follow-up. Multiple complications may occur at the same time in patients following VPS implantation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Ventriculoperitoneal shunt complications: A review. Interdiscip Neurosurg. 2018;S13:66-70.
- [Google Scholar]
- Late pediatric ventriculoperitoneal shunt failures: A Singapore tertiary institution's experience. Neurosurg Focus. 2016;41:E7.
- [Google Scholar]
- Ventriculoperitoneal shunt complications needing shunt revision in children: A review of 5 years of experience with 48 revisions. Afr J Paediatr Surg. 2012;9:32-9.
- [Google Scholar]
- Trans-anal protrusion of ventriculo-peritoneal shunt catheter with silent bowel perforation: Report of ten cases in children. Pediatr Surg Int. 2007;23:575-80.
- [Google Scholar]
- Review of the management of peroral extrusion of ventriculoperitoneal shunt catheter. J Clin Diagn Res. 2016;10:PE01-6.
- [Google Scholar]
- Complications of peritoneal shunts. In: Di Rocco C, Turgut M, Jallo G, Martínez-Lage J, eds. Complications of CSF Shunting in Hydrocephalus: Prevention, Identification, and Management. Switzerland: Springer International Publishing; 2015. p. :187-202.
- [Google Scholar]
- Complications of ventriculoperitoneal shunts in children in Dar es Salaam. East Cent Afr J Surg. 2005;10:55-9.
- [Google Scholar]
- Disconnection as a cause of ventriculoperitoneal shunt malfunction in multicomponent shunt systems. Pediatr Neurosurg. 1990;16:309-11.
- [Google Scholar]
- Ventriculoperitoneal shunt disconnection associated with spontaneous knot formation in the peritoneal catheter. BMJ Case Rep 2013 2013 pii: bcr2013009590
- [Google Scholar]
- Ventriculoperitoneal shunt disconnection associated with loss of consciousness in a child patient: A case report and review of intra-abdominal complications of VP shunts. J Neurol Stroke. 2017;7:00237.
- [Google Scholar]






