Translate this page into:
Intraoperative changes in capnography during transnasal pituitary surgery: Cause may be trigeminocardiac reflex
*Corresponding author: Shalvi Mahajan, Department of Anaesthesia and Intensive Care, Postgraduate Institute of Medical Education and Research, Chandigarh, India. drshalvimahajan@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Raj VP, Kaur K, Mahajan S, Goyal A. Intraoperative changes in capnography during transnasal pituitary surgery: Cause may be trigeminocardiac reflex. J Neurosci Rural Pract, doi: 10.25259/JNRP_273_2023
Dear Sir,
Real-time capnography monitoring is the standard of care for safe anesthesia practice. With the “Shark fin” appearance on the capnography, we as anesthesiologists have the propensity to look at causes related to anesthetic drugs and ventilator circuits. However, we tend to forget the surgical causes involved in its appearance while contemplating surgery. The Kratschmer reflex and peripheral trigeminocardiac reflex (TCR) are one such understated cause for the “Shark fin” appearance during transnasal endoscopic pituitary surgery, and herein, we report a similar presentation. Informed written consent was obtained from the patient for the same.
A 57-year-old, 70 kg, non-smoker, American Society of Anesthesiologist-II (controlled hypertension) male patient was posted for pituitary macroadenoma resection through transnasal endoscopic approach. Pre-operative workup was unremarkable. Inside the operating theater, standard monitors were attached. For induction of anesthesia, morphine, propofol, and vecuronium were used. At a train of four (TOF) counts of 0, the trachea was intubated with an 8.5-mm endotracheal tube. The volume-controlled mode of ventilation was targeted to end-tidal carbon dioxide between 35 and 40 mmHg. Background infusion of propofol, dexmedetomidine, and intermittent vecuronium was initiated to achieve a bispectral index of 40–50 and TOF count of <2, respectively. The nostrils were packed with betadine and adrenaline-soaked meroseal. The surgeon introduced a nasal endoscope, and within 1 min of its insertion, heart rate (HR) dropped from 76/min to 39/min, peak airway pressure rose to 40 cmH2O from 15 cmH2O, and the capnogram showed up sloping of the third phase of capnogram without change in hemodynamics [Figure 1a]. The surgeon was informed, and the nasal endoscope was removed. Over a period of 10 min, HR and capnogram became normal and peak airway pressure dropped [Figure 1b]. With 0.2% incidence of intraoperative bronchospasm, routine causes such as mechanical (kinking of ETT, water trap clogging, obstruction of sampling line), physiological (light plane of anesthesia, analgesia, inadequate muscle relaxation), and pathological (respiratory tract infection, asthma, chronic obstructive pulmonary disease, pneumothorax, air embolism, pulmonary edema) for the changed capnogram were ruled out as [Figure 1c].[1] A similar event re-occurred when the nasal endoscope was re-introduced. Surgeons were asked to infiltrate nasal mucosa with 3 mL of xylocaine. Thereafter, the entire procedure was uneventful.
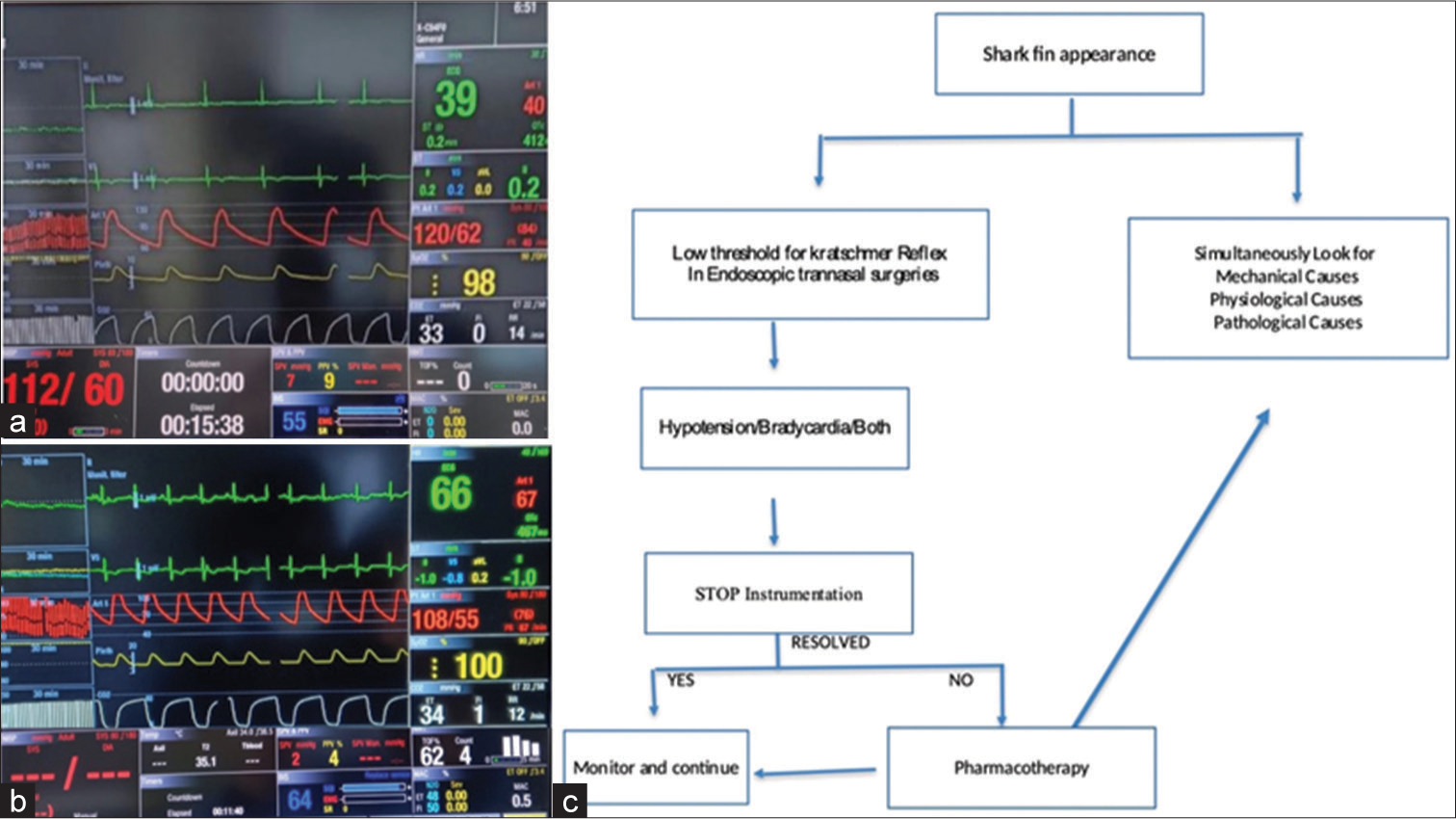
- (a) Shows hemodynamics during the event, (b) shows hemodynamics before extubation, (c) shows approach to shark fin appearance.
TCR occurs in 10% of patients undergoing endoscopic transnasal pituitary surgery.[2] The naso-cardio-respiratory reflex is a peripherally generated TCR following stimulation of mucosa of the respiratory tract starting from the nasal cavity. It is characterized by cardiorespiratory changes, including bradycardia, hypotension, and bronchospasm. The phylogenetic protective reflex arc has cranial nerve V as its afferent limb and cranial nerve X as its efferent. When stimulated, the richly innervated nasal mucosa can cause vagal-mediated parasympathetic activation and autonomic disturbances.[3]
For neurosurgical patients, the Kratschmer reflex can be undervalued and misinterpreted for raised intracranial pressures secondary to intracranial pathology. Inadequate depth of anesthesia, hypoxemia, and hypercapnia can precipitate the reflex.[4] With the intense discharge of parasympathetic activity, varied manifestations can occur, and all components of the reflex may not be seen simultaneously. In our patient, bradycardia and bronchospasm were noted but blood pressure remained stable. Removal of the precipitating stimulus can undo this response. Nasal infiltration with local anesthetic before instrumentation can be helpful, as seen in the indexed case. Pharmacological support with vagolytic drugs and adrenaline should be kept ready though not required every time.[5]
During transnasal endoscopic pituitary procedures, when trying to find the cause of the up-sloping of the capnogram curve, the possibility of the Kratschmer reflex should be borne in mind, because there is always more than what meets the eye.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Anaesthesia for patient with chronic obstructive pulmonary disease. Indian J Anaesth. 2015;59:574-83.
- [CrossRef] [Google Scholar]
- Functional outcome changes in surgery for pituitary adenomas after intraoperative occurrence of the trigeminocardiac reflex: First description in a retrospective observational study. Medicine (Baltimore). 2015;94:e1463.
- [CrossRef] [Google Scholar]
- Trigemino-cardiac reflex during transsphenoidal surgery for pituitary adenomas. Clin Neurol Neurosurg. 2005;107:468-74.
- [CrossRef] [Google Scholar]
- Nasocardiac reflex during aspiration and injection through a nasogastric tube: An infrequent occurrence. Indian J Crit Care Med. 2015;19:237-9.
- [CrossRef] [Google Scholar]
- Trigeminocardiac reflex: An overview. Rev Argent Cardiol. 2018;86:276-82.
- [CrossRef] [Google Scholar]





