Translate this page into:
Wallenberg's syndrome
Address for correspondence: Dr. Shishir Shetty, Department of Oral Medicine and Radiology, A.B Shetty Memorial Institute of Dental Sciences, Nitte University, Deralakatte, Mangalore- 575 018, India. E-mail: drshishirshettyomr@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
The lateral medullary syndrome may be total or partial depending on the involvement of vessels supplying lateral medulla.[1] It is most often secondary to intracranial vertebral artery or posterior inferior cerebellar artery occlusion due to atherothrombosis or embolism and sometimes due to spontaneous dissection of the vertebral arteries.[2] Embolism can also be seen in cocaine abuse, medullary neoplasms, radionecrosis, hematoma, neck manipulation, and trauma and bullet injury to the vertebral artery.[2] A 52-year-old male patient presented to the department of oral medicine and radiology with the complaint of pain of the back tooth region of the lower-left jaw and swelling in the lower-left-half of the face since 2 days. He also complained of difficulty in swallowing and speech along with weakness of the limbs on the right side. The patient was hypertensive and diabetic, and had stopped medications without physician's consult since 1 year. He was a chronic smoker for past 35 years and occasionally consumed alcohol. The patient was immediately referred to the medical hospital where a thorough clinical examination was performed. Patient was admitted and routine blood investigations were carried out that revealed the high-fasting blood sugar level (143 mg/dl), high cholesterol level (230 mg/dl). Echocardiography and carotid doppler revealed no abnormalities. Magnetic resonance (MR) scan was carried out and reported by a qualified radiologist as hyperintense lesions seen on T2 W and fluid attenuation inversion recovery sequences (FLAIR) involving the posterolateral aspect of left medulla with swelling of the left-half of the medulla, suggestive of infarct [Figure 1a]. Few focal T2 and FLAIR hyperintensities seen in the centrum semiovale of the left frontal and parietal lobes suggestive of ischemic changes [Figure 1b]. MR angiography revealed focal loss of flow void seen in the left vertebral artery just before the formation of the basilar artery and involving the left PICA origin, suggestive of thrombosis/occlusion [Figure 1c]. An emergency endodontic therapy was initiated with intravenous antibiotics. Oral hypoglycemics, antihypertensives, and blood thinners (aspirin) were administered to the patient by the physician. Speech therapy was initiated a week later, following which patient was discharged. The endodontic treatment was completed. Periodic follow up of the patient every week for a period of 6 months revealed a gradual but remarkable improvement in the speech and motor activity of the patient.
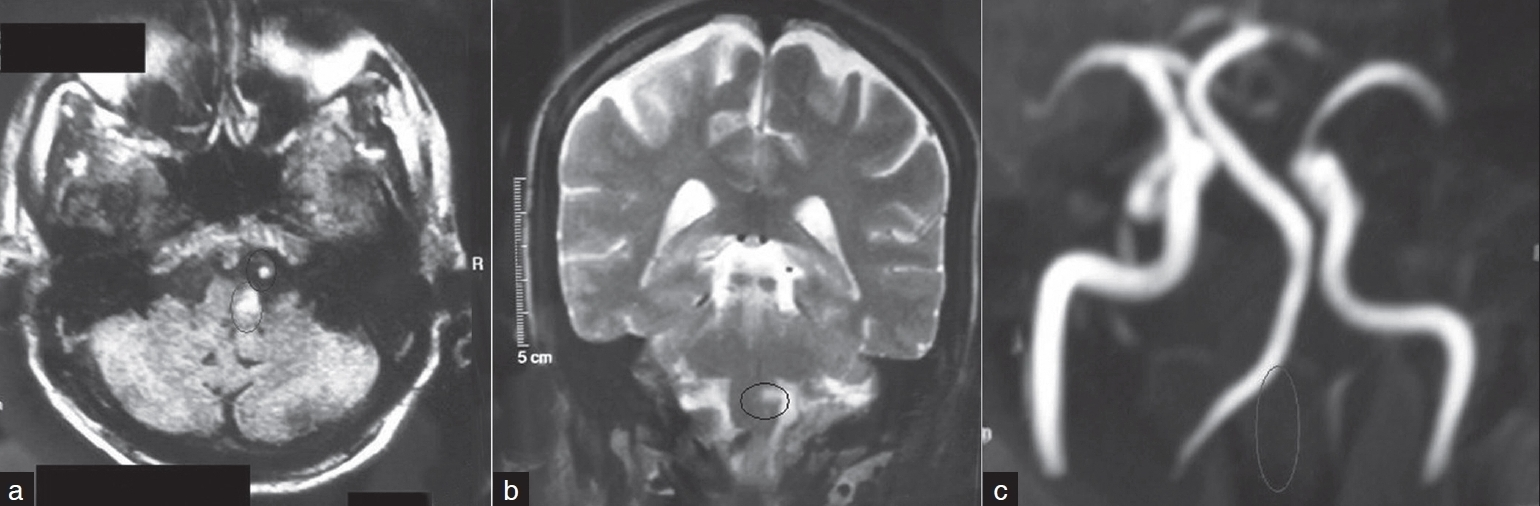
- (a) A FLAIR image showing a high signal in the left postero lateral medulla suggestive of an infarct (circle in image) and there is a white round lesion immediately in front of the medulla indicative of the thrombosed left vertebral artery (circle in image), (b) Image shows a coronal T2 weighted MRI in which there is high signal (hyperintensity) in the left medulla which is suggestive of an infarct (circle in image). (c)-MRI angiography sequence (3D Time of Flight (TOF) sequence). This shows absence of the normal left vertebral artery (shown with circle in image)
The triad of Horner's syndrome, ipsilateral ataxia, and ipsilateral hyperalgesia clinically identify patients with the lateral medullary syndrome. Nevertheless, the manifestation is broad and includes numbness, dysphagia, vertigo, nausea-emesis, hoarseness, hiccups, facial pain, visual disturbance.[3] A comprehensive study on patients with main clinical findings associated with swallowing dysfunction in patients with Wallenberg's syndrome revealed 85% of dysphonia, 30% difficulty in bolus control, 35% palatal paresis, 15% facial weakness, and 60% accumulation of saliva.[4] While the lateral medullary syndrome remains a clinical diagnosis based upon a characteristic history and constellation of physical findings, MRI offers improvement in visualization of the medullary infarction. In addition, MRI can demonstrate coexisting cerebellar infarction that may have previously been clinically unsuspected and undetected by CT. Visualization of such infarctions by MRI can alert the clinician to the potential for serious complications associated with large cerebellar lesions.[5]
References
- Role of electrical stimulation of palate in patients of lateral medullary syndrome with dysphagia. Ind J Phys Med Rehabil. 2006;17:45-8.
- [Google Scholar]
- An unusual presentation of lateral medullary syndrome with ipsilateral UMN facial palsy – an anatomic postulate. Ann Indian Acad Neurol. 2005;8:37-40.
- [Google Scholar]
- Dysphagia in lateral medullary infarction (Wallenberg's syndrome): an acute disconnection syndrome in premotor neurons related to swallowing activity? Stroke. 2001;32:2081-7.
- [Google Scholar]
- Magnetic resonance imaging in Wallenberg's lateral medullary syndrome. Stroke. 1986;17:542-5.
- [Google Scholar]





