Translate this page into:
Vertebral artery dissecting aneurysm with subarachnoid hemorrhage treated by coil trapping: A case report
*Corresponding author: Ashari Bahar, Division of Neurointervention and Endovascular Therapy, Department of Neurology, Hasanuddin University, Makassar, Indonesia. asharibahar@med.unhas.ac.id
-
Received: ,
Accepted: ,
How to cite this article: Hawari I, Bahar A, Halim W. Vertebral artery dissecting aneurysm with subarachnoid hemorrhage treated by coil trapping: A case report. J Neurosci Rural Pract. doi: 10.25259/JNRP_70_2025
Abstract
Vertebral artery dissection (VAD) is one of the most common causes of stroke, especially in young ages. It was found in 20% of ischemic strokes in young people and causes 2% of ischemic strokes. Dissecting intracranial pseudoaneurysm (IP) is a rare disorder that is associated with VAD that often leads to subarachnoid hemorrhage. We report a 43-year-old male presented with right vertebral artery dissection at the V4 segment and associated ruptured IP. The patient is treated with coil trapping at the dissected segment and maintained on nimodipine 60 mg/6 h and acetazolamide 250 mg bid. The patient was discharged with a slight improvement in muscle strength in the left and right arms. Endovascular treatment is considered the main interventional management of VAD. No established guidelines exist in the treatment of VAD. The choice of treatment is based on anatomical factors, clinical conditions, and potential risks and benefits associated with each treatment procedure.
Keywords
Case report
Coiling
Dissecting aneurysm
Subarachnoid hemorrhage
INTRODUCTION
Vertebral artery dissection (VAD) is one of the most common causes of stroke in young ages, especially in people under 45 years of age. VAD was found in 20% of ischemic stroke in young people. In general, it causes 2% of ischemic stroke, with middle-aged and younger patients as high as 10–25%. The diagnosis is often difficult with subtle symptoms and signs, while symptoms of stroke may evolve in the following days after acute dissection. The majority of dissections are intracranial with high mortality and morbidity unless treated appropriately.[1] The mortality, as high as 19–83%, is caused by subarachnoid hemorrhage (SAH), with a 70% risk of rebleeding in the first 24 h.[2]
Dissecting intracranial pseudoaneurysm (IP) is a rare disorder that is associated with VAD. It has a high risk of rupture caused by a disruption in the vessel wall, especially along the thin tunica intima of the vertebral artery (VA). The rupture often leads to SAH and ischemic complications caused by a thromboembolic lesion from the dissecting segment.[3]
The management of dissecting IP in intracranial VAD remains controversial. No established guidelines exist to date in treating this complication. The treatment is now based on several case series or case reports.[4] Treatment relies heavily on endovascular management instead of surgical treatment. The main goal of treatment of VAD is to prevent the rupture of IP or rebleeding in ruptured IP and to minimize embolic events and neurological deficits. Endovascular treatment consists of stenting, coiling, or flow diversion with or without assisted coiling. We report successful treatment of ruptured dissecting IP in the segment V4 VA with coiling.
CASE REPORT
Patient information and clinical findings
A 43-year-old male developed a severe headache and sudden-onset right extremity weakness. He developed weakness in four extremities two days later. On physical examination, he was awake with positive nuchal rigidity. Further examination showed left facial and hypoglossal nerve palsy with reduced strength in all 4 extremities.
Diagnostic assessment
Computed tomography (CT) showed SAH in falx cerebri and tentorium cerebelli, and intraventricular bleeding in the fourth ventricle and foramen Luschka [Figure 1]. Digital subtraction angiography (DSA) demonstrated dissection of the right VA in the V4 segment marked by string sign and associated IP with duplication of posterior inferior cerebellar artery (PICA) distal to the dissected segment [Figure 2a].
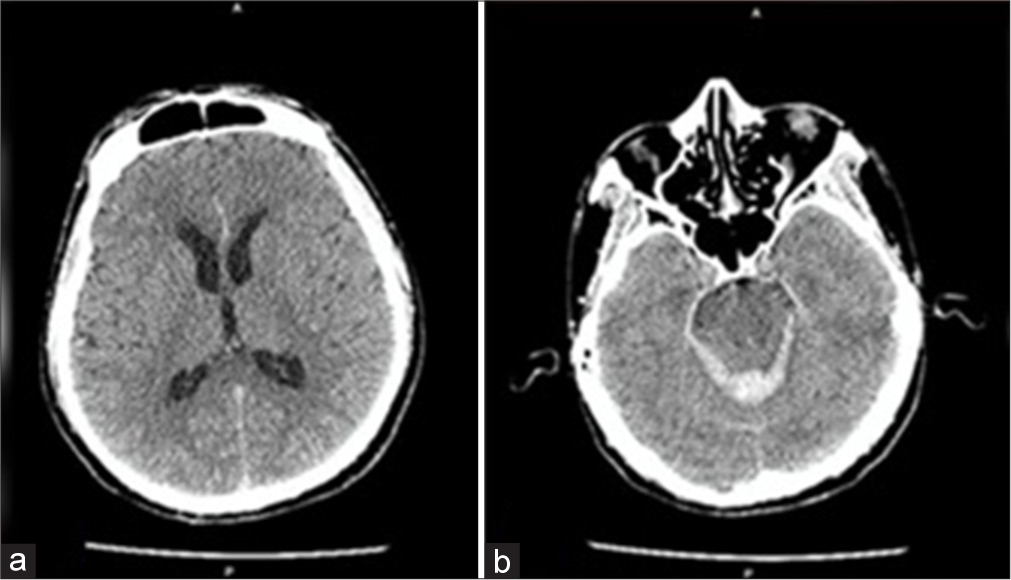
- (a) Non-contrast axial computed tomography of the head showed subarachnoid hemorrhage in the falx cerebri and tentorium cerebelli. (b) Intraventricular bleeding in the fourth ventricle extended to the foramen Luschka.
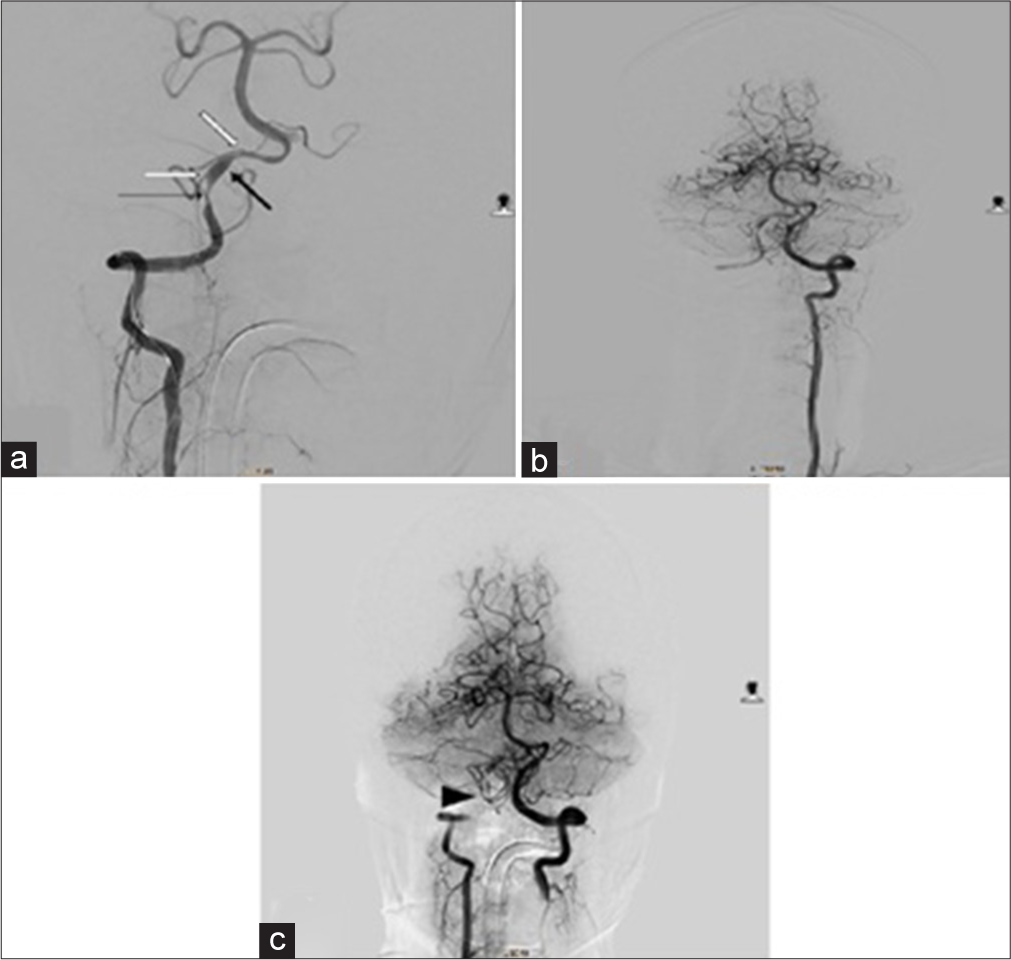
- (a) Digital subtraction angiography of right VA injection shows pseudoaneurysm (thick black arrow) as dilatation of right vertebral artery at V4 segment, stenosis (thin black arrow) of the same segment, and duplication of origin of PICA (white arrows). (b) Left VA injection demonstrates adequate blood flow to the right PICA from the contralateral (left) VA. (c) Simultaneous right and left VA injection shows occlusion of right VA with coil mass (arrowhead) with preservation of blood flow to right PICA from left VA.
Therapeutic intervention
A 6 Fr sheath was placed in the femoral artery, and the right VA was sacrificed with coil trapping at the V4 segment using Axium Prime 3D bare platinum 3 mm × 8 cm coil, Microplex 10 hypersoft 3D 2 mm × 4 cm coil, and 3D 1 mm × 2 cm coil. The final DSA demonstrated total occlusion of the V4 segment [Figure 2b] and preservation of the PICA [Figure 2c]. The patient was alert and awake and maintained on nimodipine 60 mg/6 h and acetazolamide 250 mg bid.
Follow-up and outcomes
The follow-up CT scan three days after the procedure shows reduced subarachnoid (in falx cerebri and tentorium cerebelli) and intraventricular bleeding (in the fourth ventricle). The patient was discharged with moderate disability and a slight improvement of muscle strength in the right and left arms (graded 4+/5 and 5/5, respectively), while no improvement in the right and left legs (graded 4/5 and 4+/5, respectively). On 1 month follow-up, the patient remained well. He required some help and was unable to walk without assistance due to the prolonged dizziness he felt since his admission to the hospital. He was prescribed flunarizine 5 mg bid.
DISCUSSION
The incidence of dissecting intracranial artery with pseudoaneurysm is reported to be 5–40%. The aneurysms may manifest as saccular or fusiform aneurysms. Early investigation can be performed with a CT scan, CT angiography, or magnetic resonance angiography.[5] In one study conducted by Lee et al., 79% of VA dissection with IP presents with acute SAH. The IP carries a high potential for rebleeding with a re-rupture rate of 30–58% and brings poor outcomes with mortality rates as high as 46.7%.[6]
Endovascular treatment is considered the main interventional management of VAD due to being less invasive, relatively low procedure-related complications, and high efficacy. Until recently, no universally established guideline exists in the management of VAD. The choice of treatment is based on anatomical factors, clinical conditions, and potential risks and benefits associated with each treatment procedure. Deconstructive technique with occlusion of VA segment with coil is effective in preventing recurrent rupture and bleeding. The possibilities of occluding the VA segment must be performed with consideration of the collateral flow from the contralateral VA and its relation to the origin of PICA. If the lesion segment is proximal or distal to the origin of PICA, coiling with internal trapping can be performed without blocking the blood flow to the PICA, which vascularizes the cerebellum. If the segment is of PICA origin, internal trapping can be performed with additional PICA bypass surgery or PICA stenting.[7]
In our patient, the SAH involved the posterior fossa with dissecting lesion and IP at the V4 segment. The PICA is duplicated, with both ostium-originated distal to the dissecting and IP segment. With adequate collateral blood flow from the left VA to both origins of the PICA, this is the ideal case to perform a deconstructive technique with internal coil trapping at the dissecting segment.
The deconstructive technique offers several benefits compared to the reconstructive technique with stent-assisted coiling, flow-diverting stenting, or multiple stenting. This technique effectively prevents rebleeding, reduces the risk of recurrence, and allows other surgical procedures such as external ventricular drainage or decompressive surgery when indicated, and no antiplatelet medication is necessary.[8]
CONCLUSION
Our patient presented with VAD and IP at the V4 segment of the right VA with clinical manifestation of SAH. The origin of PICA is distal to the dissected segment so we choose coil trapping as the main interventional treatment supported with nimodipine and acetazolamide as pharmacological management. While there is still limited evidence in the literature regarding the best treatment for VAD, endovascular treatment is still a reasonable choice compared to traditional surgical intervention due to its high safety profile and effectiveness.
Ethical approval
The work has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Vertebral artery dissection In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441827 [Last accessed on 2023 Mar 20]
- [Google Scholar]
- Vertebrobasilar dissection with pseudo-aneurysm or subarachnoid hemorrhage: Intracranial stenting as the only treatment: A report of three cases. Interv Neuroradiol. 2009;15:87-91.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery dissection and associated ruptured intracranial pseudoaneurysm successfully treated with coil assisted flow diversion: A case report and review of the literature. Brain Circ. 2021;7:159-66.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery dissection managed by interventional radiology. BMJ Case Rep. 2022;15:e245914.
- [CrossRef] [PubMed] [Google Scholar]
- Dissecting pseudoaneurysm: Predictors of symptom occurrence, enlargement, clinical outcome, and treatment. J Neurosurg. 2016;125:936-42.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous dissecting aneurysm of the intracranial vertebral artery: Management strategies. Yonsei Med J. 2007;48:425-32.
- [CrossRef] [PubMed] [Google Scholar]
- Vertebral artery dissection from etiopathogenesis to management therapy: A narrative review with neuroimaging's case illustration. Egypt J Neurol Psychiatry Neurosurg. 2024;60:118.
- [CrossRef] [Google Scholar]
- Endovascular treatment strategies for vertebral artery dissection: A single-center experience and literature review. J Neurointensive Care. 2024;7:1-11.
- [CrossRef] [Google Scholar]







