Translate this page into:
Unilateral hydrocephalus due to membranous occlusion of the foramen of Monro following extraventricular drainage and ventriculoperitoneal shunt for hydrocephalus after subarachnoid hemorrhage
*Corresponding author: Kengo Kishida, Department of Neurosurgery, Saiseikai Shiga Hospital, Ritto, Shiga, Japan. kkishida@koto.kpu-m.ac.jp
-
Received: ,
Accepted: ,
How to cite this article: Kishida K, Oka H, Sakamoto M. Unilateral hydrocephalus due to membranous occlusion of the foramen of Monro following extraventricular drainage and ventriculoperitoneal shunt for hydrocephalus after subarachnoid hemorrhage. J Neurosci Rural Pract. 2024;15:600-2. doi: 10.25259/JNRP_370_2024
Abstract
We present a case of unilateral hydrocephalus caused by membranous occlusion of the foramen of Monro in a 56-year-old male. The patient was initially treated with external ventricular drainage and a ventriculoperitoneal shunt for secondary hydrocephalus due to subarachnoid hemorrhage. However, unilateral hydrocephalus with enlargement of the left lateral ventricle subsequently developed. Imaging revealed membranous obstruction at the left foramen of Monro, and the patient was successfully treated with endoscopic septostomy and foraminoplasty. This case highlights the importance of considering membranous occlusion of the foramen of Monro in similar clinical scenarios and supports the efficacy of endoscopic surgery as a therapeutic option.
Keywords
Endoscopy
Isolated lateral ventricle
Secondary hydrocephalus
Foraminoplasty
INTRODUCTION
Hydrocephalus due to the occlusion of the foramen of Monro is a rare condition. The causes include congenital anomalies, tumors, hemorrhagic events, infections, and post-shunt procedures, with most cases being congenital and occurring in children.[1] Both unilateral and bilateral forms occur, with bilateral cases being more common.[2] Unilateral cases in adults with identifiable membranous structures on imaging are exceedingly rare. There is no established treatment for this condition, but the usefulness of endoscopic surgery has been reported in recent years.
Here, we present a case of unilateral hydrocephalus due to membranous occlusion of the foramen of Monro following extraventricular drainage and ventriculoperitoneal shunt for hydrocephalus after subarachnoid hemorrhage, successfully treated with endoscopic surgery.
CASE REPORT
A 56-year-old male presented with posterior neck pain and altered consciousness and was transferred to our hospital. Plain computed tomography (CT) revealed diffuse subarachnoid hemorrhage and acute hydrocephalus [Figure 1a]. Contrast-enhanced CT showed a dissecting aneurysm at the right vertebral artery distal to the posterior inferior cerebellar artery. External ventricular drainage was performed through bilateral frontal horns of the lateral ventricles, followed by parent artery occlusion. The ventricular drains were placed in the right lateral ventricle and the third ventricle through the left foramen of Monro [Figure 1b]. After the right ventricular drain was removed on the 3rd post-operative day, only the left lateral ventricle became slit-like [Figure 1c]. One month later, following the removal of the left ventricular drain, secondary hydrocephalus developed. A ventriculoperitoneal shunt was placed through the occipital horn of the right lateral ventricle [Figure 1d]. The patient was transferred to a rehabilitation hospital without any infection.
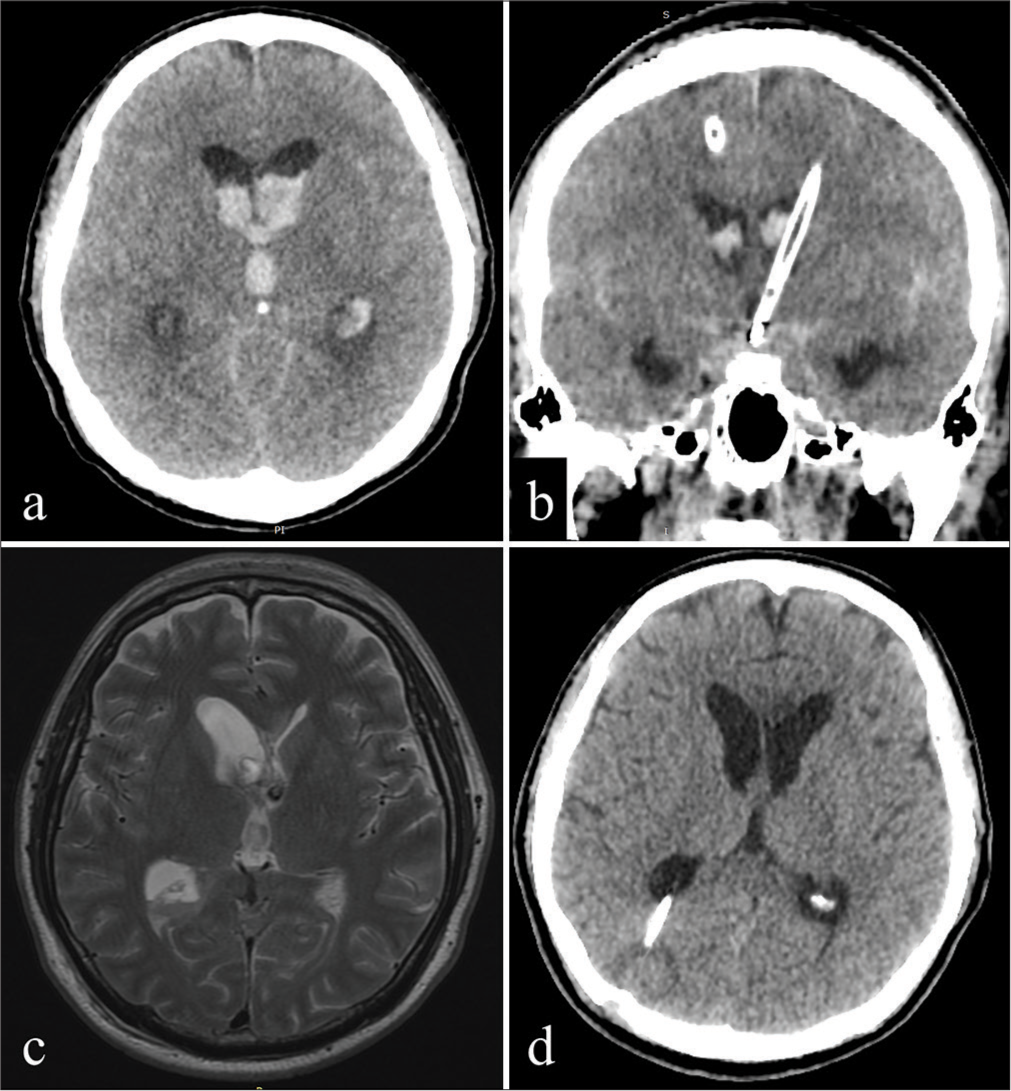
- (a) Plain computed tomography revealed diffuse subarachnoid hemorrhage and acute hydrocephalus. (b) External ventricular drainage was performed through bilateral frontal horns of the lateral ventricles and the ventricular drains were placed in the right lateral ventricle and the third ventricle through the left foramen of Monro. (c) After the right ventricular drain was removed, only the left lateral ventricle became a slit-like appearance. (d) One month later, secondary hydrocephalus developed and a ventriculoperitoneal shunt was placed through the occipital horn of the right lateral ventricle.
Three months later, the patient exhibited somnolence. CT revealed enlargement of only the left lateral ventricle, prompting readmission to our hospital [Figure 2a]. Shuntography ruled out shunt malfunction. Subsequent CT scans showed contrast filling the right lateral ventricle but not the left [Figure 2b]. Heavy T2-weighted images from magnetic resonance imaging revealed a membranous structure at the left foramen of Monro [Figure 2c and d]. We diagnosed unilateral hydrocephalus due to membranous occlusion of the left foramen of Monro, and endoscopic septostomy and foraminoplasty were performed [Figure 2e and f]. Postoperatively, the membrane of the foramen of Monro was fenestrated [Figure 2g and h]. After surgery, the asymmetry and enlargement of the lateral ventricles and the symptoms of hydrocephalus improved by adjusting the shunt pressure.

- (a) Two months later, computed tomography (CT) revealed enlargement of only the left lateral ventricle. (b) CT after shuntography showed contrast filling the right lateral ventricle but not the left. (c) The axial and (d) coronal view of heavy T2-weighted images from magnetic resonance imaging (MRI) revealed a membranous structure at the left foramen of Monro (arrow). (e and f) We diagnosed unilateral hydrocephalus due to membranous occlusion of the left foramen of Monro, and endoscopic septostomy and foraminoplasty were performed. (g) Postoperative axial and (h) coronal view of MRI showed that membrane of the foramen of Monro was fenestrated (arrowhead).
DISCUSSION
Membranous occlusion of the foramen of Monro is an extremely rare condition, especially in adults. Schultz and Leeds previously described intraventricular septations forming from microglial membranes extending from glial tufts through denuded ependymal areas post-meningitis.[3] Similar processes may occur in the foramen of Monro. In this case, the tip of the drainage tube was near the left foramen of Monro. We speculate that the primary cause of this condition was tissue damage from this drain placement near the foramen of Monro, which triggered an inflammatory response. However, it is noteworthy that, even in similar cases of hydrocephalus following hemorrhage and extraventricular drainage, membranous occlusion remains rare. Therefore, another factor must be considered: Cerebrospinal fluid dynamics. The drains created a slit-like appearance in the left lateral ventricle, suggesting impaired communication of cerebrospinal fluid among the left lateral ventricle and the other ventricles. Furthermore, the placement of a ventriculoperitoneal shunt in the right lateral ventricle may have altered cerebrospinal fluid dynamics. These factors may have contributed to the formation of membranous structures.[4]
Neuroendoscopic surgery, particularly foraminoplasty and septostomy, has been increasingly recognized as an effective intervention in such cases.[5,6] By reestablishing communication between the ventricles and restoring natural cerebrospinal fluid flow, endoscopic techniques can effectively resolve hydrocephalus while minimizing the need for permanent shunt placement. Such procedures offer a significant advantage, reducing the risks of long-term complications often associated with shunt dependence, such as infection or mechanical failure.
In this case, endoscopic surgery resulted in a successful outcome, with restoration of normal cerebrospinal fluid dynamics and resolution of the patient’s symptoms. The reestablishment of the anatomical pathway through fenestration of the membranous occlusion proved crucial in this patient’s recovery. This case underscores the importance of considering endoscopic interventions when membranous occlusion of the foramen of Monro is suspected, especially in adult patients following hemorrhagic events or external ventricular drainage.
CONCLUSION
Membranous occlusion of the foramen of Monro can occur after subarachnoid hemorrhage, ventricular drainage, or shunt surgery for hydrocephalus. Neuroendoscopic surgery, particularly foraminoplasty and septostomy, may be an effective intervention for these cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Adult idiopathic bilateral occlusion of foramen of Monro: Systematic review with illustrative case. Clin Neurol Neurosurg. 2024;241:108279.
- [CrossRef] [PubMed] [Google Scholar]
- Endoscopic strategy in surgical treatment of adult idiopathic bilateral occlusion of the foramen of Monro and review of the literature. World Neurosurg. 2018;115:e610-9.
- [CrossRef] [PubMed] [Google Scholar]
- Intraventricular septations complicating neonatal meningitis. J Neurosurg. 1973;38:620-6.
- [CrossRef] [PubMed] [Google Scholar]
- Etiological differences between the isolated lateral ventricle and the isolated fourth ventricle. Childs Nerv Syst. 2006;22:1080-5.
- [CrossRef] [PubMed] [Google Scholar]
- Neuroendoscopic foraminal plasty of foramen of Monro. Childs Nerv Syst. 2008;24:933-42.
- [CrossRef] [PubMed] [Google Scholar]
- Neuroendoscopic treatment of idiopathic occlusion of unilateral foramen of Monro presenting as chronic headache. J Neurosci Rural Pract. 2016;7:128-30.
- [CrossRef] [PubMed] [Google Scholar]







