Translate this page into:
Unilateral contiguous two level thoracic ossified hypertrophied facet joints with compressive myelopathy
Address for correspondence: Dr. Amit Kumar Thotakura, Department of Neurosurgery, NRI Academy of Sciences, Chinakakani, Mangalagiri, Guntur - 522 503, Andhra Pradesh, India. E-mail: doctoramitkumar@gmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Ossified hypertrophy of the facet joints in the thoracic region is very uncommon. We present a rare case of thoracic unilateral ossified hypertrophied facet joints with compressive myelopathy in a patient with scoliosis. The diagnosis is made with computed tomography and magnetic resonance imaging studies of the dorsal spine. Decompressive laminectomy and medial facetectomy was performed. Patient improved neurologically to normal status within 2 months. We present the review of the literature on the facet joint hypertrophy producing dorsal myelopathy.
Keywords
Facetal hypertrophy
compressive myelopathy
ossified facet arthropathy
Introduction
Thoracic compressive myelopathy results from compression of the dorsal spinal cord and can cause motor and sensory dysfunction of the lower limbs as well as bowel and bladder dysfunction. Hypertrophy of the posterior spinal elements in the thoracic region is uncommon unlike in cervical and lumbar regions. Ossified yellow ligament is seen occasionally causing compressive myelopathy in endemic fluorosis patients.[1] Facet joint ossified hypertrophy is very uncommon and there were a few case series and reports earlier.[2–8] This report is to signify the importance of the facet joint arthropathy in the differential diagnosis of dorsal compressive myelopathy.
Case Report
A 37-year-old male patient who was hailing from fluorotic region in Andhra Pradesh was apparently asymptomatic till he had trivial trauma when he slipped and fell down on the ground. He was brought in a wheel chair with complaints of weakness of both lower limbs, left lower limb more weak compared to right lower limb, numbness of the body below chest level and constipation since he fell down 10 days back. There was no history of urinary disturbances. On examination, he had spastic paraparesis of Grade 3/5 in left lower limb and Grade 4/5 in right lower limb. Knee and ankle reflexes were exaggerated in both lower limbs. Plantar reflexes were extensor bilaterally. There was sensory loss below T4 level bilaterally. Clinically there was asymmetrical D2 spinal compressive myelopathy left side more than right side.
He was admitted, evaluated with serum calcium, phosphate levels and then with computed tomography (CT) thoracic spine along with other routine surgical workup. The serum calcium and phosphate levels were normal. CT scan thoracic spine revealed scoliotic curvature of the dorsal spine with convexity to left. Cursor stone of the curvature is D1 vertebra. Fusion of C7 and D1 vertebra noted suggestive of block vertebra. Extensive hypertrophy of left facet joints of D2-D3 and D3-D4 vertebrae with dense calcification was noted with intraspinal extension and severe canal stenosis. Magnetic resonance imaging (MRI) scan thoracic spine was showing hypointensity on the left of the thecal sac extradurally involving the the facet joints at D2-3 and D3-4 levels with severe compression on the cord. There was no evidence of ossified yellow ligament. [Figures 1–3]
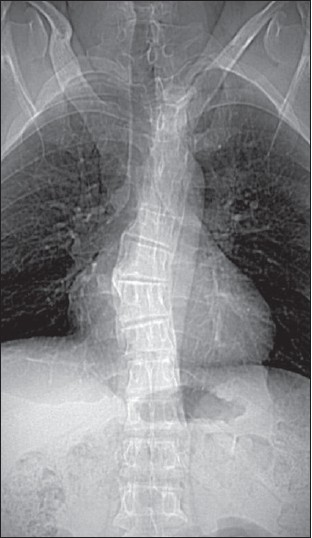
- Topogram of the computed tomography (CT) scan dorsal spine revealing scoliotic curvature with convexity to left

- CT scan dorsal spine sagittal view (a) and axial sections at D2-3 level (b) and D3-4 level (c) showing ossified hypertrophied left D2-3 and D3-4 facet joints with canal stenosis
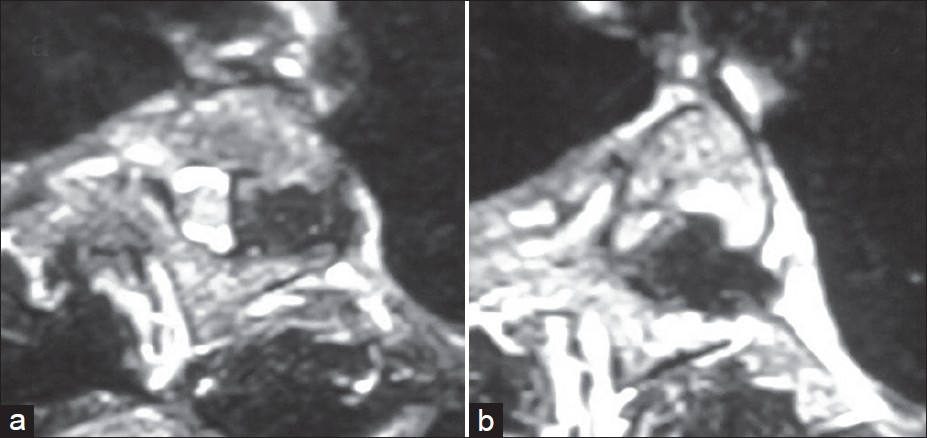
- Magnetic resonance imaging (MRI) study dorsal spine axial sections at D2-3 (a) and D3-4 (b) levels showing hypointensity at the left facet joint region compressing the the cal sac pushing it to the right side
He was operated by D2, D3 decompressive laminectomy and excision of medial half of the ossified D2-3, D3-4 left facet joints using high speed drill. The histopathological examination of the specimen revealed bone, cartilage, and synovial tissue. Postoperatively, he was taught physiotherapy after which he improved gradually and was able to walk without support at the time of discharge. By 2 months time, the power in lower limbs became normal and he returned to his normal duties. Later he was referred to the orthopedician for the treatment of the scoliosis. His last follow-up was 2 years later at which time he did not develop any further complaint.
Discussion
Hypertrophy of the posterior spinal elements in the cervical and lumbar regions is a common condition, but the same process occurring in the thoracic region is rare.
Hypertrophy of the osseous elements is even rarer, limited to several case reports and series. Ossification of the yellow ligament, a closely related pathology which also produces dorsal myelopathy, is not uncommon and is prevalent in the endemic fluorotic population.[1] The reports of compressive myelopathy due to ossification of yellow ligament were not included in this review of literature.
Osseous hypertrophy of normal posterior elements causing symptomatic compression is rare. There are three case series with facet joint hypertrophy causing thoracic myelopathy. Barnett reported seven cases of thoracic spinal stenosis caused by thickening of the laminar arch and facet joints.[2] Marzluff described four patients with thoracic spinal cord compression as a result of bilateral articular process and facetal hypertrophy.[3] Yamamoto reported seven cases of thoracic spinal stenosis caused by thickening of the laminar arch and facet joints.[4]
A few case reports of facetal joint hypertrophy were present. A single-level bilateral facetal hypertrophy at C7-T1 level,[5] T3–4 level,[6] T10–11.[7] Deogaonkar reported patients with unilateral hypertrophy at T4–5 and unilateral T6–7 and T10–11 changes.[8] Unilateral canal stenosis as a result of osseous hypertrophy has been reported only by Deogaonkar earlier.[8] A precipitating minor traumatic event can be a trigger to the clinical presentation as reported by some authors.[27] Same thing occurred in our patient, and this may give a clue to the underlying etiology.
The role of scoliosis in the facet joint hypertrophy in our patient could not be explained as the bony changes were present on the convex side of the scoliosis rather than on the concave side. As per some researchers, the cartilaginous degeneration and more trabecular bone was observed in the concave side than in the convex side of the scoliosis due to asymmetric compression and tension shared between the two sides.[910]
CT and MRI studies remain the definitive diagnostic tests. Posterior decompression is the treatment of choice provided that this is laterally and longitudinally sufficient.[24] The medial facetectomy at one or two levels does not cause the spinal instability yet one should always keep the possibility of instability in long term after extensive dorsal unroofing. Though some authors did bony fusion and fixation after decompression, it is not mandatory in all patients. Fixation is to be considered when extensive laminectomy, total facetectomy, and bilateral facetectomy are done.
Source of Support: Nil
Conflict of Interest: None declared
References
- Thoracic myelopathy caused by osteophytes of articular processes. Thoracic spondylosis. J Neurosurg. 1979;50:779-83.
- [Google Scholar]
- Severe facet joint arthrosis caused C7/T1 myelopathy: a case report. Case Report Med. 2009;2009:481459.
- [Google Scholar]
- Single-level bilateral facet joint hypertrophy causing thoracic spinal canal stenosis. J Clin Neurosci. 2009;16:1363-5.
- [Google Scholar]
- Ultrastructural studies of articular cartilaginous degeneration in the facet joints in spinal scoliosis. Nihon Seikeigeka Gakkai Zasshi. 1994;68:184-95.
- [Google Scholar]
- Trabecular bone micro-architecture in adolescent idiopathic scoliosis compared between concave and convex site of the facet joints. Zhonghua Wai Ke Za Zhi. 2005;43:777-80.
- [Google Scholar]






