Translate this page into:
Understanding non-compliance with WHO-multidrug therapy among leprosy patients in Assam, India
Address for correspondence: Prof. Ranabir Pal, Department of Community Medicine, Sikkim-Manipal Institute of Medical Sciences, 5th Mile, Tadong, Sikkim, Gangtok -737 102, India. E-mail: ranabirmon@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objectives:
The study was undertaken to assess the adherence to World Health Organization (WHO)-multidrug therapy (MDT) and its successful completion by the leprosy patients and the extent of such defaulting, its correlates and reasons.
Design:
Retrograde cohort analysis was conducted during the first quarter of 2007 from the cases registered for WHO-MDT treatment during 2002 to 2005 in Kamrup district of Assam, India.
Results:
A total of 254 leprosy cases reflected the treatment seeking behavior of registered cases during the study period. Majority of the cases were from urban areas and defaulter rate higher in urban areas. The study group consisted of 60.63% males and 39.37% females.. Both the compliance and default was higher in the age group of 16 to 30 years. Majority of defaulters (32.28%) had passed the high school leaving certificate examination had per capita monthly income between Rs 500 - 749 (30.71%) and belonged to social class IV (33.86%) and V (30.71%). Significant statistical association was found between gender, literacy status, per capita income per month and socioeconomic status with treatment outcome. On analysis for the reasons of defaulting treatment; majority (33.07%) defaulted treatment due to loss of occupational hours when they come for receiving drugs at health center, 25.98% defaulted due to adverse reactions of drugs and 18.11% feared social stigma among major causes.
Conclusions:
The causes of defaulting treatment were related to gender, educational status, income as well as social class, or some combination of these. Recommendations, on strategic interventions to obviate the cause for noncompliance, were presented.
Keywords
Compliance
default
leprosy
multi-drug therapy
Introduction
Leprosy is a disease of public health concern because of the case load and the social stigma attached to the disease. Leprosy is a disease known to be a great scourge for the suffering humanity from time immemorial. In the year 1955, the Government of India first launched a national leprosy control program. Those were the days when Dapsone was the sole cure for leprosy. During the 1970s multidrug therapy (MDT) was identified as having potential to cure leprosy and subsequently in 1982, MDT came into use. Based on this, the national leprosy eradication program was launched in 1983. Initially started in a phased manner, it took 13 years for MDT to be available countrywide.[1]
MDT has proven to be a powerful tool in the control of leprosy, especially when patients report early and start prompt treatment. Adherence to and its successful completion are equally important. Unfortunately, due to a number of personal, psychosocial, economic, medical and health service factors, a significant number of patients become irregular and default from MDT.[2]
The success of the current WHO key strategy for leprosy elimination (i.e. multidrug therapy [MDT] regimen) depends largely on the efficiency of health care delivery services and patient compliance. A high rate of noncompliance with this regimen has serious implications for the leprosy control program because it can set the stage for the emergence of drug resistance, eventually resulting in treatment failure and failure of the program.[3]
Research works on drug compliance have indicated that if a patient understands his /her disease and its treatment well, he /she is more likely to be motivated to take the whole prescribed course of treatment properly. It is widely believed that the understanding and behavior of patients in relation to drug compliance are largely influenced by their socio-economic condition and level of knowledge.[4] In 1981, a WHO study group recommended that multibacillary (MB) leprosy patients should be given multidrug therapy (MDT) for at least two years and, wherever possible, until skin-smear becomes negative.[5] To improve operational efficiency as well as to improve patient compliance in leprosy programs, Danish development assistance (DANIDA) introduced blister-calendar packs (BCP) to deliver MDT in four MDT districts in India in 1987.[6]
The study was undertaken to assess the adherence to WHO-MDT therapy and its successful completion by leprosy patients and the extent of such defaulting, its correlates and reasons.
Materials and Methods
This retrograde cohort analysis was conducted with no interventions during the first quarter of 2007 from the cases registered for WHO-MDT treatment during 2002 to 2005 in Kamrup district of Assam, India, based on both quantitative as well as qualitative parameters with review of relevant documents, records and literature. It was decided to interview patients with treatment compliance, and defaulters, using a pre-designed and pre-tested schedule. Information about type of disease, duration of disease, duration of treatment, type of treatment and patient compliance was collected from patients’ O.P.D. tickets and surveillance register. Main outcome measures were the correlates of treatment compliance and defaulters of leprosy patients.
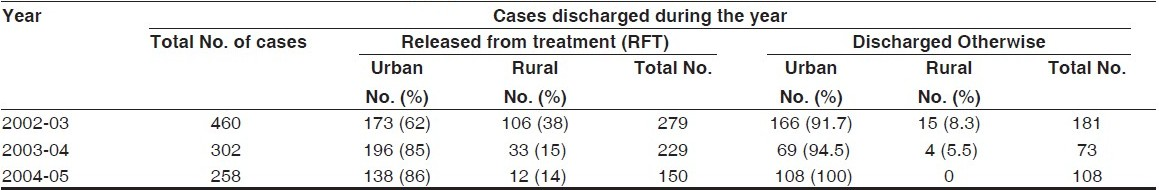
The sample was selected from the cases discharged from treatment during 2002 to 2005 in Kamrup district of Assam; the total number was 1020 among which 362 were defaulters. Year wise, 460 cases were discharged during 2002-03 of which 181 (39.35%) were defaulters. Similarly during 2003-04, among 302 cases discharged 73 (24.17%) were defaulters and during 2004-05, among 258 cases discharged 108 (41.86%) were defaulters. The time of registration of the cases defaulting treatment were variable. Only those defaulters who could not be traced back during treatment for a period of 6 months were finally discharged from treatment and reflected as discharged otherwise. Taking an average of the defaulter rate which was 35.13%, the sample size was calculated. Among 362 defaulters, 127 were selected (35.13%) randomly. To allow comparison, equal number of controls was selected from cases having treatment compliance. Pre-tested close-ended questionnaires that contained questions linking to correlates of treatment compliance and default of leprosy patients in relation with the socio-demographic situation prevailing in India. By initial translation, back-translation, re-translation followed by pilot study, the questionnaire was custom-made for the study. The pilot study was carried out on the general patients of other diseases from the same area following which some of the questions from the interview schedule were modified. The data collection tool used for the study was an interview schedule that was based on at the institute with the assistance from the faculty members and other experts developed on information provided by the global experts prior to the study for ensuring feasibility, acceptability, time management, validity and reliability.
Institutional ethical committee approved the study. All the patients or their caregivers were explained the purpose of the study and were ensured strict confidentiality. Written informed consents were taken from each patient / caregiver prior to the study. They were given the option not to participate in the study if they wanted. The principal investigator then collected the data using the interview technique. The collection of the data was from the January 15 till the March 30, 2007. On an average, five to six interviews were conducted in a day. Details of the questionnaire can be provided, if required. Information on leprosy was disseminated to the patients their and caregivers in health education sessions to complement the findings of study.
The data collected were thoroughly cleaned and entered into MS-Excel spread sheets for analysis. The procedures involved were transcription, preliminary data inspection, content analysis and interpretation. The statistical analyses were done using Graph Pad In Stat “version 3” soft ware. Percentages and Chi square tests were used in this study to analyze epidemiological variables.
Results
Among the total number of cases discharged in the period from 2002 to 2005, the percentage of defaulters was very high. Defaulter rate was higher in urban areas 91.7%, 94.5% and 100% in respective years of study even in presence of more accessible health services and more educated and stabilized communities.
A total of 254 leprosy cases reflected the treatment seeking behavior of the registered cases during study period. Majority of the cases were from urban areas [Table 1].
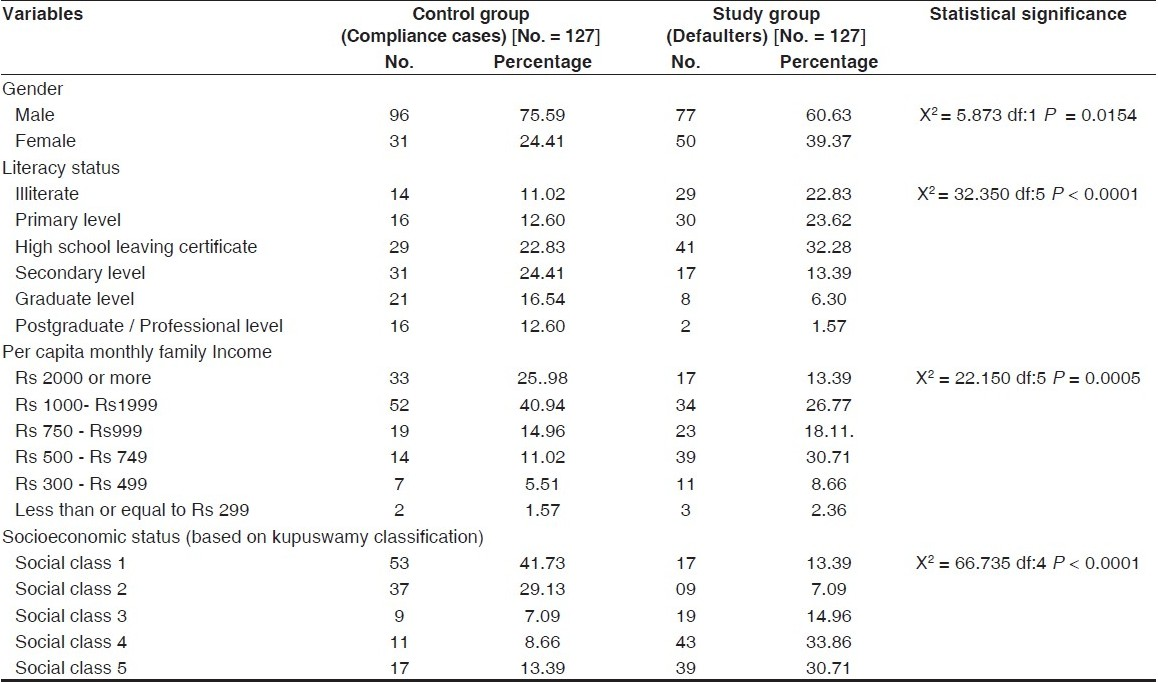
The study group consisted of 60.63% males and 39.37% females whereas the control group had 75.59% males and 24.41% females. Both the compliance and default was higher in the age group of 16 to 30 years. Significant statistical association was found between gender and treatment completion status.
The distribution of defaulters on basis of literacy status, per capita monthly income and socioeconomic status in comparison to control group reflected that majority (32.28%) had passed the high school leaving certificate examination and per capita monthly income between Rs 500- 749 (30.71%) and belong to social class IV (33.86%) and V (30.71%). There is significant statistical association between literacy status, per capita income per month and socioeconomic status with treatment outcome [Table 2].
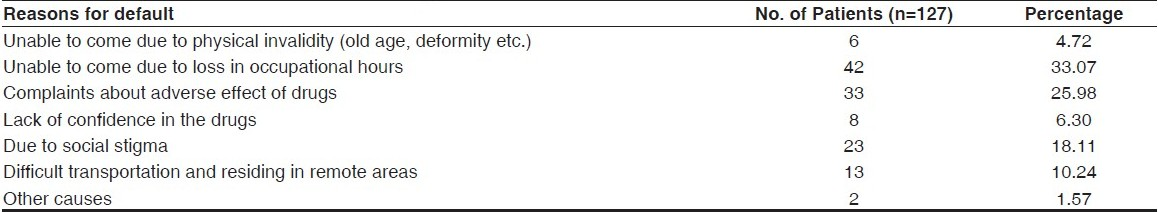
On analysis of the reasons of defaulting treatment, majority (33.07%) defaulted treatment due to loss of occupational hours when they had to receive drugs at the health center, 25.98% defaulted due to adverse reactions of drugs, 18.11% feared social stigma, 10.24% were unable to continue due to difficult transportation from their residing area, 4.72% could not come due to physical inability and rest 1.57% could not give any valid reasons [Table 3].
Discussions
A total of 254 leprosy cases reflected the treatment seeking behavior of the registered cases during the study period. Majority of the cases were from urban areas and defaulter rate was higher in urban areas.
The study group consisted of 60.63% males and 39.37% females. Both the compliance and default was higher in age group - 16 to 30 years. Majority of the defaulters (32.28%) had passed the high school leaving certificate examination and per capita monthly income between Rs 500- 749 (30.71%) and belong to social class IV (33.86%) and V (30.71%). Significant statistical association was found between gender, literacy status, per capita income per month and socioeconomic status with treatment outcome. On analysis for the reasons of defaulting treatment, majority (33.07%) defaulted treatment due to loss of occupational hours when they come for receiving drugs at health centre. 25.98% defaulted due to adverse reactions of drugs and 18.11% feared social stigma among major causes.
According to researchers from New Delhi, in six leprosy mission hospitals, nearly half of the patients closer to the hospitals defaulted as compared to 60% who stayed beyond. Patients from outside the district had significantly higher default rate for all types of leprosy cases as compared to patients living close by to the centers.[2]
A community-based descriptive study conducted in 12 leprosy endemic areas in Cebu, Philippines, showed that the noncompliance rate with the WHO-MDT regimen among 233 study subjects was 30%. The causes of noncompliance are drug-related, health care provider-triggered, or patient-inducted, or some combination of these.[3]
In a non-intervention study carried-out in Dhanusha - a district in Nepal, among a total of 57 non-compliant leprosy cases, majority were illiterate, laborers by occupation and from poor economic class family background (73.7%).[4]
An analytic cross-sectional study was carried out in Dhanusha district, Nepal. There were 183 male (68.3% on MB-MDT) and 90 female (61.1% MB-MDT) leprosy patients. The study found that 79.2% of male patients completed treatment, while 34.4% female patients did not complete within the given time frame. The study found significant associations between treatment completion status and gender (adjusted OR 2.05, 95% CI: 1.07-3.94), educational status (adjusted OR 2.37, 95% CI: 1.12-4.99.[7]
A study from two districts in Cabo Delgado province in Northern Mozambique conducted during the period from 1993 to 1997 found that 548 (59.2%) of 926 MB patients completed treatment and 378 (40.8%) defaulted during the period. The percentage of defaulters fell steadily from 59.8% in 1993 to 23.2% in 1997. Of the 378 defaulters, 57.7% defaulted treatment within six months and 83.1% within one year of starting treatment. It was observed that patients tend to default early rather than late in the treatment period and that this pattern is maintained over time despite a fall in defaulter rates. Patients established early into a treatment routine were more likely to complete treatment.[8]
A study from Mumbai followed smear-positive leprosy cases registered at an urban leprosy center for three years to study the ‘drop-out’ pattern in them and judge the utility of some corrective measures for the same. The results were compared with ‘drop-out’ in smear-positive cases registered at the same centre in 1989, 1990, 1992 and 1993. By introduction of the special measures, the ‘drop-out’ rate was significantly reduced from 52% (for other years) to 36% (1991).[9]
Strength of study
The lack of positive attitude could be an important barrier to eradication of leprosy. The causes of non-compliance explored by us ranged from the relatively longer course of treatment to irregular supply of the drugs, health caregiver prompted, receiver inducted or an amalgamation of these.
Limitation of study
In our study we presented an analysis of primary data collected by recall method and therefore short memory and forgetfulness of the study population during interview may fail to give accurate information. Again, collection of secondary data was difficult to some extent because of reasons like frequent transfer of government officials and dependence on government records.
Future directions of study
The success of the current WHO key approach for leprosy elimination schedule depends for the most part on the competence of health care delivery services and patient conformity. Research on post intervention knowledge and practice among patients and caregivers has to be repeatedly explored.
Conclusion
WHO-MDT has proven to be a commanding tool in control of leprosy, particularly when patients report early and start treatment without delay. Observance to and its successful completion are uniformly imperative. Unfortunately, due to a number of individual, psycho-social, financial, therapeutic and health service factors, a considerable quantity of patients become irregular and defaulting from WHO-MDT. Impetus, encouragement and regular contact with patients may help.
Recommendations
India is a multi-cultural multi-lingual and geographically uneven country. Any short term solution may not help us to reach the goal of eradication of leprosy in India in near future. Health professionals alone will not be able to deal with this mammoth task. Recommendations on strategic interventions to obviate the cause for noncompliance and to solve the problem, points to holistic responsibility of professionals, health services, governments and teaching institutions.
Health education
Health education system needs to improve knowledge about leprosy among the people with lesser educational level. It could be done by means of improving educational tools preferably based on audiovisual techniques. Preferably, school curriculum should include material to allay fears hovering around leprosy. The system should create wider awareness about the importance of continuation of full course of therapy for cure of leprosy.
Removal of myths and misconceptions
The information education and communication system should have some productive advertisements to motivate the general public for leprosy. Advertisements need to help clear the myths and misconceptions about leprosy.
Incentives of health care providers and people
To obviate the cause for noncompliance we have to train and re train health care workers of all levels with periodic random evaluation by health service research, and above the political will to remove this menace from the globe. The general public also has to be encouraged and motivated to help eradicate leprosy. There should be provision of incentives like help diagnosing patients in his/her wards/ relations/ friends. A non-monetary incentive in the form of certificates of recognition may also be another motivating factor.
Better facilities
Patient-friendly health services, spreading awareness about the advantages of eradicate leprosy not only for the patient but also for the citizen, could be motivating factors, making people aware of recent findings like association of WHO-MDT with a lower risk of relapse.
Source of Support: Nil
Conflict of Interest: None declared.
References
- National Leprosy Eradication Programme and progress towards elimination of leprosy in India. J Indian Med Assoc. 2004;102:674-6.
- [Google Scholar]
- A study on non-adherence to MDT among leprosy patients. Indian J Lepr. 2008;80:149-54.
- [Google Scholar]
- Noncompliance with the World Health Organization-multidrug therapy among leprosy patients in Cebu, Philippines: Its causes and implications on the leprosy control program. Dermatol Clin. 2008;26:221-9.
- [Google Scholar]
- Leprosy disease in Nepal: Knowledge and non-compliance of patients. J Nepal Med Assoc. 2005;44:39-43.
- [Google Scholar]
- Experience with WHO-recommended multidrug therapy (MDT) for multibacillary (MB) leprosy patients in the leprosy control program of the All Africa Leprosy and Rehabilitation Training Center in Ethiopia: Appraisal of the recommended duration of MDT for MB patients. Int J Lepr Other Mycobact Dis. 1991;59:558-68.
- [Google Scholar]
- Further observations on MDT blister-calendar packs in vertical leprosy eradication programmes: A multicentre study (phase II) Lepr Rev. 1993;64:250-4.
- [Google Scholar]
- Gender differences in epidemiological factors associated with treatment completion status of leprosy patients in the most hyperendemic district of Nepal. Southeast Asian J Trop Med Public Health. 2004;35:334-9.
- [Google Scholar]
- Defaulting patterns in a provincial leprosy control programme in Northern Mozambique. Lepr Rev. 2001;72:199-205.
- [Google Scholar]
- The pattern of ‘drop-out’ of smear-positive cases at an urban leprosy centre. Indian J Lepr. 1996;68:161-6.
- [Google Scholar]






