Translate this page into:
Traumatic Posterior Fossa Hematoma, A Rare Entity: Study of 21 Cases
Vinod Sharma, MBBS, MS, MCh Room No. F 13, Resident Doctors Hostel, SMS Hospital, Jaipur, Rajasthan India neurovinod@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Background Traumatic posterior fossa hematoma is a rare entity. Traumatic posterior fossa hematomas are associated with considerable morbidity and mortality and their surgical management remained controversial.
Methods From August 2011 to August 2017, approximately 5,100 patients with head injury were managed. Authors reviewed clinical and radiological findings, management criteria, and outcome of posterior fossa hematoma in 21 patients.
Results Out of 21 cases, 13 survived with our management. The Glasgow Coma Scale (GCS) on admission was higher in favorable group than in poor outcome group. Factors associated with Glasgow Outcome Scale in two groups were status of fourth ventricle, basal cisterns, subarachnoid hemorrhage (SAH), hematoma volume, and their location (hemispheric or midline). Similarly, associated supratentorial lesions, age, gender, lesions in other parts of body, and timing from injury to reporting to hospital were taken into consideration.
Conclusion The factors correlated with patient outcome were age, sex, mode of injury, GCS at admission, associated intracranial hematomas, associated SAH, hematoma volume, hematoma location, basal cisterns, status of fourth ventricle, and associated multiple injuries on other body parts. It is hereby concluded that timely surgical intervention should be employed whenever indicated without delay. Posterior fossa hematomas were rarely observed in the pediatric age group.
Keywords
traumatic posterior fossa hematoma
subarachnoid hemorrhage
Glasgow Coma Scale
Introduction
Traumatic posterior fossa hematoma is very less as compared with spontaneous hematomas associated with hypertension. They are associated with significant mortality and morbidity. They constitute a small subset of total head injury patients.1 As we know, posterior fossa have small volume, and any increase in volume due to any cause may cause increase intracranial pressure, herniation, and deterioration. Traumatic posterior fossa hematomas account for < 1% in all head injury patients.2 3 Liu4 reported the incidence of traumatic posterior fossa hematoma to be 3.7% of total intracranial hematomas. These hematomas may be totally asymptomatic, with a sudden increase in size can lead to rapid deterioration of neurological status.5
Traumatic cerebellar hematoma may be isolated or may be associated with subdural hemorrhage (SDH), extradural hemorrhage (EDH), and subarachnoid hemorrhage (SAH) in posterior fossa. They may present acutely or in delayed manner. The hematoma location, volume, initial Glasgow Coma Scale (GCS) score, status of fourth ventricle, and basal cisterns are important in final outcome. Management of these hematomas nowadays have changed from all surgery to conservative management.1
Authors evaluated outcome of patients on GCS score at admission, location, volume, status of cisterns, fourth ventricle, SAH, and supratentorial lesions. The surgical indications were posterior fossa hematoma with mass effect, midline shift, size greater than 3 cm, effaced basal cisterns, fourth ventricle compression, and associated supratentorial lesions with significant mass effect with midline shift.
Similarly, patients were managed conservatively with respect to hematoma location, size less than 3 cm, normal basal cisterns, and fourth ventricle. In some of these hematomas, early surgical intervention is deemed necessary.5 6 7 9 9 The early results of surgery are good, so surgical intervention if required should not be delayed. The course and prognosis of midline hematoma is worse, so evacuation should be done early.
Methods
From August 2011 to August 2017, approximately 5,100 patients with head injury were admitted in our institute. This study was focused on 21 patients (0.41%) with traumatic posterior fossa hematomas. The clinical findings, mode of injury, initial GCS, various radiological parameters, and final outcome were evaluated in 21 patients using Glasgow Outcome Scale (GOS). GOS was graded into good recovery (GR), moderate disability, severe disability (SD), vegetative state (VS), and death (D).
Initial computed tomography (CT) head was obtained at admission of patient and repeat CT head was done at 6 hours if the patient deteriorated more than 2 points of initial GCS score at admission. On CT scan, hematoma location, size, status of basal cisterns (normal or compressed), status of fourth ventricle (normal or compressed), associated SAH, and supratentorial lesions were evaluated. Hematoma volume was assessed by using formula A*B*C/2, where A is maximum transverse diameter of hemorrhage on CT, B is anterioposterior diameter, and C is number of CT slices showing hematoma.10
Hematomas were classified as type 1 vermian hematoma (Fig. 1) and type 2 hemispheric hematoma involving superficial two-thirds of the hemisphere (Figs. 2 and 3). Injury is classified as coup, countercoup, and acceleration-deceleration type. Time to reach hospital is important as it affects overall morbidity and mortality of patient.
Results
Clinical and Radiological Findings
Out of 21 patients, 18 were male and the rest females. Most of the patients were in the age range of 30 to 60 years. The mode of injury was road traffic accident (15 patients) and fall (6 patients). Duration between sustaining injury and reporting to hospital was 4 hours in 11 patients and 5 to 8 hours in 10 patients. GCS score on admission ranged from 3 to 15 as shown in Table 1. The location of hematoma was type 1 (8 patients) and type 2 (13 patients). Nine patients had isolated posterior fossa hematoma and 12 patients presented with associated intracranial lesions.
Intracranial lesions were supratentorial contusion (11), SDH (2), EDH (2), SAH (9), IVH (1), diffuse axonal injury (DAI) (1), hydrocephalus (HCP) (2), and SDH in posterior fossa in 1 patient (Fig. 3C). Basal cisterns were compressed in 9 and normal in 12 patients. Fourth ventricle had intraventricular hemorrhage (IVH) in 3, was compressed in 3, and normal in 15 patients. Associated injuries were found in 8, and skull fracture was seen in 15 patients. Out of 8 patients, only 1 had splenic injury which was managed conservatively and 1 patient had hemothorax which was managed by intercostal tube drainage.

-
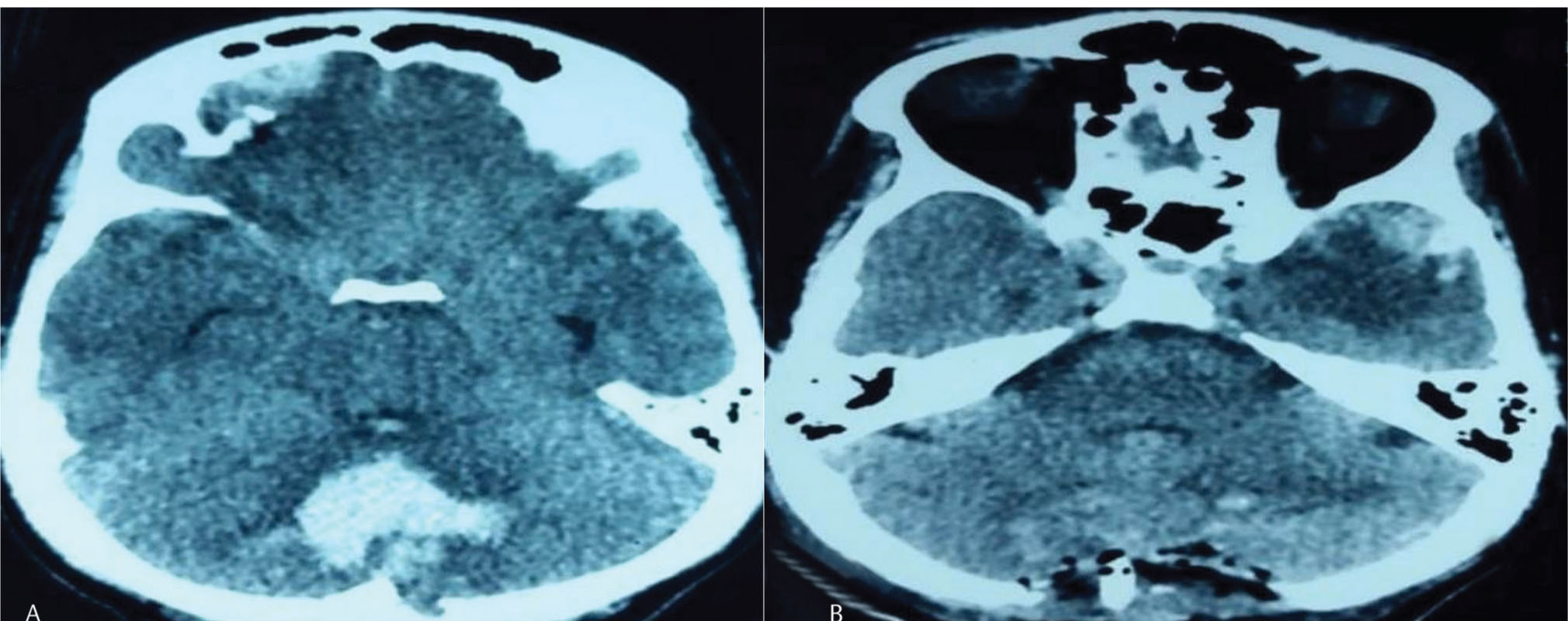
Fig. 1 (A) Computerized tomography scan revealing vermian hematoma (type 1). (B) Postoperative scan after suboccipital craniectomy and hematoma evacuation (type 1).
Fig. 1 (A) Computerized tomography scan revealing vermian hematoma (type 1). (B) Postoperative scan after suboccipital craniectomy and hematoma evacuation (type 1).
-
Fig. 2 (A) Computerized tomography scan revealing preoperative image type 2 hematoma. (B) Postoperative scan showing complete removal of hematoma.
Fig. 2 (A) Computerized tomography scan revealing preoperative image type 2 hematoma. (B) Postoperative scan showing complete removal of hematoma.
-
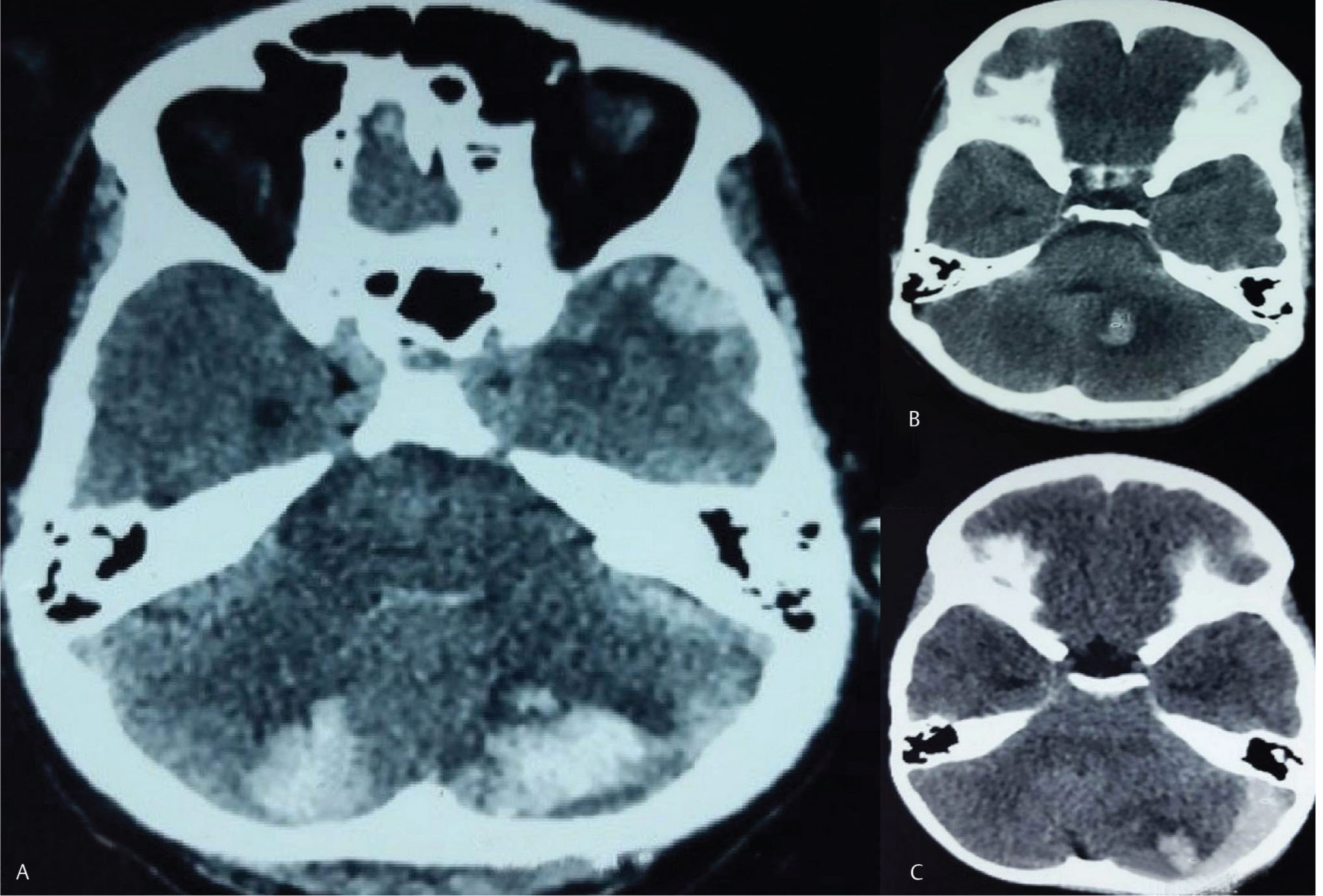
Fig. 3 (A) Computerized tomography scan revealing bilateral type 2 hematoma. (B) Computerized tomography revealing type 2 hematoma. (C) Computerized tomography revealing type 2 hematoma with subdural hemorrhage.
Fig. 3 (A) Computerized tomography scan revealing bilateral type 2 hematoma. (B) Computerized tomography revealing type 2 hematoma. (C) Computerized tomography revealing type 2 hematoma with subdural hemorrhage.
|
S. no. |
Age (y) |
Sex (M/F) Durationa |
Mode of injury, skull fracture |
Associated lesions |
Site of impact |
GCS (3-15) |
Volume, cm3, size (cm) |
Type of location (½) |
Basal cisterns (N/C) |
Fourth ventricle (N/C/IVH) |
Associated supratentorial lesions |
SAH (A/P) |
Intervention |
GOS |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Abbreviations: A, absent; C, compressed; D, death; DAI, diffuse axonal injury; EDH, extradural hemorrhage; F, female; GCS, Glasgow Coma Scale; GOS, Glasgow Outcome Scale; GR, good recovery; HCP, hydrocephalus; ICD, intercostal tube drainage; IVH, intraventricular hemorrhage; M, male; MD, moderate disability; MVA, motor vehicle accident; N, normal; P, present; SAH, subarachnoid hemorrhage; SD, severe disability; SDH, subdural hemorrhage; VS, vegetative state. Note: D-Site of impact could not be identified (acceleration-deacceleration injury), skull fracture (+, present;-absent). aDuration: Timing from injury to reporting to hospital in hours compared with type 1. SAH and supratentorial contusions were relatively higher in type 1 hematomas. There was no significant difference in other factors. |
||||||||||||||
|
1 |
40 |
M, 4 h |
MVA,- |
None |
Occipital |
14/15 |
16.8 (3.5 cm) |
2 |
N |
IVH |
No lesion |
A |
Suboccipital craniectomy |
GR |
|
2 |
40 |
M, 6 h |
MVA,+ |
None |
Frontal |
5/15 |
4 (2) |
1 |
C |
N |
Right frontal contusion |
P |
Conservative |
D |
|
3 |
30 |
F, 7 h |
MVA,+ |
None |
Fron tal, occipital |
6/15 |
19.2 (4) |
2 |
C |
N |
Right fron-to-tempo-ro-parietal acute SDH with IVH |
P |
Subocipital craniectomy |
D |
|
4 |
12 |
M, 2 h |
MVA,- |
None |
Occip ital |
15/15 |
2 (2) |
2 |
N |
N |
No lesion |
A |
Conservative |
GR |
|
5 |
65 |
M, 4 h |
Fall,+ |
Abdominal injury |
Occip ital |
12/15 |
15.4 (3.5) |
2 |
N |
N |
No lesion |
A |
Suboccipital craniectomy |
MR |
|
6 |
47 |
M, 2 h |
MVA,+ |
Fracture left ulna |
Occip ital |
13/15 |
40 (5) |
2 |
N |
C |
No lesion |
A |
Suboccipital craniectomy |
MR |
|
7 |
35 |
M, 3 h |
Fall,- |
None |
Occip ital |
13/15 |
15.4 (3.5) |
2 |
N |
N |
No lesion |
A |
Suboccipital craniectomy |
GR |
|
8 |
75 |
F, 6 h |
Fall,+ |
None |
Occiput |
7/15 |
19.2 (4) |
2 |
N |
C |
No lesion |
P |
Suboccipital craniectomy |
D |
|
9 |
22 |
M, 8 h |
MVA,+ |
Fracture femur |
Fron tal, occipital |
5/15 |
4 (2) |
1 |
C |
N |
Left frontal EDH, with bilateral temporal contusions, with hydrocephalus |
P |
Supratentorial craniectomy |
D |
|
10 |
79 |
M, 7 h |
Fall,+ |
None |
Occip ital |
7/15 |
15.4 (3.5) |
2 |
N |
IVH |
No lesion |
P |
Suboccipital craniectomy |
VS |
|
11 |
25 |
M, 1 h |
MVA,- |
None |
Occip ital |
15/15 |
1 (1) |
2 |
N |
N |
No lesion |
A |
Conservative |
GR |
|
12 |
55 |
M, 3 h |
MVA,- |
Fracture clavicle |
Occip ital |
14/15 |
5.2 (3), 5 (2.5) |
2 (bilateral) |
N |
N |
Left temporal contusion |
A |
Conservative |
GR |
|
13 |
55 |
M, 2 h |
MVA,+ |
Fracture humerus |
Occip ital |
13/15 |
15.4 (3.5) |
1 |
C |
IVH |
No lesion |
A |
Suboccipital craniectomy |
MR |
|
14 |
56 |
F, 6 h |
MVA,+ |
Fracture femur |
Fron tal, occipital |
7/15 |
15 (3) |
1 |
C |
C |
Left frontotemporal contusion |
P |
Suboccipital and supratentorial craniectomy |
D |
|
15 |
25 |
M, 5 h |
MVA,+ |
Fracture tibia |
Temporal |
9/15 |
1 (1) |
2 |
N |
N |
Right basifrontal contusion, right temporal EDH, and left temporal contusion, right fron-to-tempo-ro-parietal SDH |
P |
Conservative |
SD |
|
16 |
47 |
M, 4 h |
Fall,+ |
None |
Frontal |
3/15 |
2 (2) |
1 |
C |
N |
Right frontal contusion with right frontotemporal acute SDH |
P |
Conservative |
D |
|
17 |
53 |
M, 6 h |
MVA,- |
None |
Frontal |
6/15 |
5 (2.5) |
1 |
C |
N |
Bilateral basifrontal contusions, diffuse axonal injury |
P |
Conservative |
D |
|
18 |
42 |
M, 6 h |
MVA,+ |
None, chest injury |
Frontal |
10/15 |
15.8 (3.5) |
2 |
N |
N |
Right frontal contusion with mild hydrocephalus |
A |
Suboccipital craniectomy, ICD |
SD |
|
19 |
54 |
M, 8 h |
Fall,+ |
None |
Temporal |
5/15 |
12 (3) |
2 |
C |
N |
Left temporoparietal contusion |
A |
Conservative |
D |
|
20 |
43 |
M, 4 h |
MVA,+ |
None |
Occipital |
9/15 |
4 (2) |
1 |
C |
N |
Bilateral frontal contusion |
P |
Conservative |
SD |
|
21 |
32 |
M, 4 h |
MVA,+ |
None |
Occipital |
15/15 |
5.2 (3) |
1 |
N |
N |
Right frontal contusion |
A |
Conservative |
GR |
Type 1 and Type 2 Hematoma Outcome
Comparison between type 1 and 2 hematomas is shown in Table 2. Age range in type 1 was 22 to 56 years, while in type 2 hematomas it was 12 to 79 years. In type 2 hematomas, age varied over a wider range as compared with type compared with type 1. Volume of hematoma was higher in type 2 hematomas as compared with type 1. SAH and supratentorial contusions were relatively higher in type 1 hematomas. There was no significant difference in other factors.
Treatment and Outcome
In our study, 10 patients were treated conservatively and 11 patients underwent surgery. All patients with surgical indications were operated immediately without any delay. Out of 11 patients, 10 patients underwent suboccipital craniectomy and hematoma evacuation, and 1 patient underwent both supratentorial and suboccipital craniectomy. CT head (Fig. 3) suggestive of type 2 hematomas were managed conservatively and those suggestive of type 2 hematoma (Fig. 1) managed by suboccipital craniectomy with hematoma evacuation. Outcome of 21 patients was GR in 6, MR (moderate recovery) in 3, SD in 3, VS in 1, and D in 8 patients. The incidence of poor outcome was 61.9% (13/21).
Prognostic Factors
Frequency, age (range), sex, mode of injury, GCS, hematoma location, basal cisterns, fourth ventricle, SAH, supratentorial contusions, SDH, EDH, IVH, DAI, lesion in posterior fossa, and their relationship with outcome are shown in Table 3. Agewise distribution shows that there were no females in the favorable group and all females were in the poor outcome group suggesting that females had higher mortality in posterior fossa hematoma.
In our study, GCS at admission was higher in the favorable group as compared with the other group. Brainstem cisterns were compressed in 2 patients in the favorable group as compared with 7 in the poor outcome group. Fourth ventricle was compressed in 1 patient in the favorable group. There was significant presence of SAH in the poor outcome group as compared with the favorable group.
Discussion
These hematomas approximately constitute one-fourth of all posterior fossa traumatic lesions,3 11 but their frequency is almost between SDH and EDH.9 12 Sato et al13 established 0.7% incidence of cerebellar contusions. Nagata et al reported their frequency to be between 0.6 and 0.82%. The incidence observed in our series was 0.41%, which correlates well with other figures. Various mechanisms are responsible for these hematomas but remain unclear. These could be coup and countercoup injuries. Coup injuries are thought to be the most frequent mechanism.1,7,14 Countercoup injuries are considered to be rare.15
|
Factors |
Type 1 |
Type 2 |
|---|---|---|
|
Abbreviations: A, absent; C, compressed; DAI, diffuse axonal injury; EDH, extradural hemorrhage; F, female; IVH, intraventricular hemorrhage; M, male; MVA, motor vehicle accident; N, normal; P, present; SAH, subarachnoid hemorrhage, skull fracture (+, present;−, absent); SDH, subdural hemorrhage. |
||
|
Total patients |
8/21 |
13/21 |
|
Age (range), y |
22–56 |
12–79 |
|
Sex (M/F) |
7/1 |
11/2 |
|
Mode of injury (Fall/MVA) |
1/7 |
5/8 |
|
Skull fracture (present/absent) |
7/1 |
8/5 |
|
Hematoma volume (cm3), mean |
6.8 |
14.1 |
|
Basal cisterns (N/C) |
1/7 |
11/2 |
|
Fourth ventricle (N/C/IVH) |
6/1/1 |
9/2/2 |
|
SAH (P/A) |
6/2 |
4/9 |
|
Contusion (P/A) |
7/1 |
4/9 |
|
EDH (P/A) |
1/7 |
1/12 |
|
SDH (P/A) |
1/7 |
1/12 |
|
IVH (P/A) |
0/8 |
1/12 |
|
DAI (P/A) |
1/7 |
0/13 |
|
SDH in posterior fossa (P/A) |
0/8 |
1/12 |
Another mechanism for traumatic intracerebellar hematoma involves acceleration and deacceleration injuries.16 In our series, 7/21 patients had coup (33.3), 4/21 (19.0) had countercoup injuries, and the rest (47.6) had acceleration-deacceleration injuries. So, this leads us to the conclusion that acceleration and deacceleration is a common cause as reported previously by Takeuchi et al.17
Delayed or evolving hematoma has been reported previ-ously.18 19 In our series, no cases of delayed or evolving hematoma was reported as repeat scan was done within 6 hours of admission as mentioned previously. However, repeat CT examination is necessary, as delayed hematomas can develop.
The incidence of poor outcome in previously published series were around 20 to 100% (average 60%),2 and in our series, it was 61.9%. The prognosis was better in good GCS patient and in patients who were promptly operated with surgical indication.20 Summary of published series of posterior fossa hematomas are depicted in Table 4.
D’Avella et al have described protocol for traumatic intracerebellar hematomas as follows:
-
Conservative approach is a treatment option for noncomatose patients with intracerebellar clots 3 cm, except when associated with other EDH or SDH of posterior fossa.
-
Surgery should be done for any patient with any clot > 3 cm.
In our study, surgery was done in 11 patients, out of which 7 patients survived and 4 expired. In our series, type 1 hematomas were more frequent in the poor outcome group due to easy compression of brainstem or involvement of deep cerebellar nuclei which lead to bad prognosis.17
|
Factors |
Favorable outcome group |
Poor outcome group |
|---|---|---|
|
Abbreviations: A, absent; C, compressed; DAI, diffuse axonal injury; EDH, extradural hemorrhage; F, female; GCS, Glasgow Coma Scale; HCP, hydrocephalus; IVH, intraventricular hemorrhage; M, male; MVA, motor vehicle accident; N, normal; P, present; SAH, subarachnoid hemorrhage; SDH, subdural hemorrhage. aDuration: Timing from injury to reporting to hospital in hours, skull fracture (+, present; – absent). |
||
|
Frequency (patients), M/F |
13/21, (13/0) |
8/21, (5/3) |
|
Mode of injury (fall/MVA) |
3/10 |
3/5 |
|
Skull fracture (present/absent) |
8/5 |
7/1 |
|
GCS (range) |
7–15 |
3–7 |
|
Duration (timing from injury sustained to reporting to hospital), hours, mediana |
4–5 h |
6 h |
|
Hematoma location (½) |
3/10 |
5/3 |
|
Hematoma volume (mean) |
12.1 |
10.05 |
|
Basal cisterns (N/C) |
11/2 |
1/7 |
|
Fourth ventricle (N/C/IVH) |
9/1/3 |
6/2/0 |
|
SAH (P/A) |
3/10 |
7/1 |
|
Supratentorial contusion (P/A) |
6/7 |
5/3 |
|
HCP (hydrocephalus) |
1/12 |
1/7 |
|
Supratentorial EDH (P/A) |
1/12 |
1/7 |
|
IVH (P/A) |
0/13 |
1/7 |
|
DAI (P/A) |
0/13 |
1/7 |
|
SDH in posterior fossa |
1/12 |
0/8 |
Various factors influencing surgical decision were patients with poor GCS, advanced age, poor general condition, clinical signs of early brainstem damage, bilateral cerebral clots, and associated multiple supratentorial intracranial hemorrhages with evidence of coagulopathy. These factors reflect the peculiar heterogenecity of clinical radiological picture of this subset of posterior fossa hematomas.21
HCP is usually not associated with traumatic intracerebellar clots.11 18 Karasawa et al3 mentioned of acute HCP in 20% of intracerebellar hematomas, while in our series it was 9.52%. The timing of reaching hospital is important and affects overall morbidity and mortality of patients. Most of the patients in the favorable outcome group reported to hospital within 4 to 5 hours, whereas those in the poor outcome group had reported more than 4 to 8 hours. There was single case of posterior fossa hematoma with associated SDH in our series (Fig. 1C). This suggests that associated lesions in posterior fossa hematoma such as SDH and EDH are less.
Posterior fossa hematoma is rare in children and incidence of cerebellar hematoma is much rarer.22 Most frequent mode of injury is fall followed by road traffic accident.23 Trauma is a leading cause of childhood head injury, with Center for Disease Control, stating about half a million emergency department visits in the United States is for traumatic brain injury for children aged 0 to 14 years, with 0 to 4 years being the most vulnerable group.24 Although most cases are seen in young adults, Zuccarello et al25 reported traumatic posterior fossa hemorrhage in children also. Wright9 reported 6 cases and Tsai et al11 reported 2 cases of children in their series. Similarly, in our series, we had a single child. Management of such cases is similar to adult posterior fossa hematoma.
|
Author, year |
No. of cases |
Notes |
Poor outcome (%) |
|
|---|---|---|---|---|
|
Abbreviations: AEH, acute extradural hematoma; ASH, acute subdural hematoma; ICH, intracerebellar hematoma; SAH, subarachnoid hemorrhage. |
||||
|
Tsai et al, 1980 |
14 |
In 2 cases, associated with brainstem injury |
85 |
|
|
Pozzati et al, 1982 |
7 |
All isolated clots |
42 |
|
|
St John et al, 1986 |
3 |
One case associated with AEH, one with ASH |
60 |
|
|
Hamasaki et al, 1987 |
4 |
3 cases isolated with ASH and one with both ASH and AEH |
100 |
|
|
Sato et al, 1987 |
8 |
2 cases with concomitant diffuse cerebral contusions |
50 |
|
|
Zuccarello et al, 1982 |
5 |
All children |
20 |
|
|
Nagata et al, 1991 |
14 |
All delayed hematomas, one personal case, and literature review |
64 |
|
|
Karasawa et al, 1997 |
13 |
11 cases with associated supratentorial ICH, SAH, or ASH; 2 cases with associated infratentorial ASH |
54 |
|
|
D’Avella et al, 2001 |
18 |
8 cases of isolated intracerebellar clots |
50 |
|
|
Present series |
21 |
9 cases of isolated posterior fossa hematoma |
61 |
|
Suboccipital craniectomy with hematoma evacuation is the most preferred surgical approach in posterior fossa.26 27 Clinical with radiological features, types of hematomas, prognostic factors, and final outcome are discussed and mentioned in Table 1 Table 2 Table 3. In summary, patients who reported within 4 hours of trauma, with initial GCS score of between 9 and 15, absent SAH, normal basal cisterns, and normal fourth ventricle had better survival rate. However, older age group and females fared worse in our study as shown in Table 1 Table 2 Table 3. In severely ill subjects, surgery should be individualized for each patient with reasonable salvageability.
Conclusion
Traumatic cerebellar hematoma is a life-threatening condition that requires timely management. Nowadays, with wider availability of CT and intensive neuromonitoring, smaller hematomas can be managed conservatively and larger ones with surgical evacuation in clinically deteriorating patients.
The factors correlated with patient outcome were age, sex, mode of injury, GCS at admission, associated intracranial hematomas, associated SAH, hematoma volume, hematoma location, basal cisterns, status of fourth ventricle, and associated multiple injuries on other body parts. It is hereby concluded that timely surgical intervention should be employed whenever indicated without delay. This study had some limitations, like sample size was relatively small to determine the actual prognostic factors. As these lesions are associated with higher morbidity and mortality, it should be evaluated further to explore pathophysiology for better clinical outcome of patients.
Conflict of Interest
None declared.
Funding None.
References
- Traumatic intracerebellar hemorrhage: clinicoradiological analysis of 81 patients. Neurosurgery. 2002;50(1):16-25. discussion 25–27
- [Google Scholar]
- Characteristics of diagnosis and treatment of traumatic intracerebellar hemorrhage [in Chinese] Zhonghua Wai Ke Za Zhi. . 1997;35(3):166-167.
- [Google Scholar]
- Le lesioni traumatiche espansive della fossa cranica posteriore. Su 4 casi di contusione-lacerazione cerebellare. Minerva Neurochir. 1967;11(3):230-239.
- [Google Scholar]
- Traumatic cerebellar hematoma without subdural hematoma. JAMA. 1976;235(5):530-531.
- [Google Scholar]
- The syndrome of traumatic intracerebellar hematoma with contrecoup supratentorial complications. J Neurosurg. 1953;10(2):122-137.
- [Google Scholar]
- Traumatic hematomas of the posterior cranial fossa. J Neurosurg. 1966;25(4):402-409.
- [Google Scholar]
- The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27(8):1304-1305.
- [Google Scholar]
- Computed tomography of posterior fossa trauma. J Comput Assist Tomogr. 1980;4(3):291-305.
- [Google Scholar]
- Traumatic haematomas.Brain Surgery: Complication Avoidance and Management. 1993. p. :1931-1952. In: ed. Vol. 2.
- [Google Scholar]
- Clinical study of traumatic cerebellar contusion [in Japanese] No Shinkei Geka. 1987;15(12):1285-1289.
- Traumatic hematomas of the posterior fossa. A clinicopathological spectrum. Surg Neurol. 1986;25(5):457-466.
- [Google Scholar]
- Hematoma in the posterior fossa secondary to a tangential gunshot wound of the occiput: case report and discussion. Neurosurgery. 1991;28(4):603-605. discussion 605–606
- [Google Scholar]
- The persistent vegetative state after closed head injury: clinical and magnetic resonance imaging findings in 42 patients. J Neurosurg. 1998;88(5):809-816.
- [Google Scholar]
- Traumatic intra-cerebellar haematoma: study of 17 cases. Br. J Neurosurg. 2011;25(1):62-67.
- [Google Scholar]
- Traumatic delayed intracerebellar hematoma [in Japanese]-Neurol Med Chir (Tokyo) . 1988;28(9):886-890.
- [Google Scholar]
- Delayed traumatic intracerebellar hematoma: correlation between the location of the hematoma and the pre-existing cerebellar contusion-case report. Neurol Med Chir (Tokyo). 1991;31(12):792-796.
- [Google Scholar]
- Traumatic intracerebellar hemorrhagic contusions and hematomas. J Neurosurg Sci. 2001;45(1):29-37.
- [Google Scholar]
- Traumatic cerebellar haematoma in paedratic patient- a case report and review of literature. Romanian Neurosurg. 2016;XXX(4):566-572.
- [Google Scholar]
- Injury surveillance in a pediatric emergency department. Am J Emerg Med. 1999;17(6):499-503.
- [Google Scholar]
- Traumatic brain injury in United States of America: Emergency Department Visits, Hospitalization and Deaths. 2002‒2006. :CDC2010.
- [Google Scholar]
- Traumatic posterior fossa haemorrhage in children. Acta Neurochir (Wien). 1982;62(1)Acta Neurochir (Wien). 1982;62(2):79-85.
- [Google Scholar]
- Indication to surgical management of cerebellar hemorrhage. Clin Neurol Neurosurg. 1998;100(2):99-103.
- [Google Scholar]
- Surgical management of intace-rebellar haemorrhage.Schmeidek and Sweet’s Operative Neurosurgical Techniques, Indications, Methods, Results. Philadelphia: Saunders/Elsevier; 2005. p. :1061-1074. In Vol. 2, 5th ed.
- [Google Scholar]






