Translate this page into:
The retrospective and observational study of catatonia – Diagnosis, course of illness, and the response to lorazepam – in a tertiary health-care center
*Corresponding author: Astik Mane, Department of Psychiatry, HBTMC and Dr. RN Cooper Hospital, Mumbai, Maharashtra, India. kitsaenam@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Latke R, Sinha D, Miskin T, Mane A. The retrospective and observational study of catatonia – Diagnosis, course of illness, and the response to lorazepam – in a tertiary health-care center. J Neurosci Rural Pract 2023;14:258-63.
Abstract
Objectives:
In patients with catatonia, it has been discovered that benzodiazepines (BZD) have a remarkable impact. However, there is not much evidence reflecting the long-term treatment with only BZDs before considering electroconvulsive therapy.
Materials and Methods:
One-year retrospective data of patients obtained from the health management information system (HMIS) portal and records of the department of psychiatry with the diagnosis of catatonia. This data was then analyzed for adequate history, presenting complaints, treatment taken, substance use, and was organized into five groups depending on the primary diagnosis as per the Diagnostic and Statistical Manual of Mental. The scores of Bush-Francis Catatonia Rating Scales of day 1 and subsequent follow-ups were secured. Categorical variables were analyzed with the Chi-squared test. The response overtime for all the groups and its correlation with the number of visits was compared using repeated measures analysis of variance.
Results:
We found that the lorazepam challenge test versus improvement after 1 week of oral lorazepam had Pearson’s correlation of 0.604, this correlation decreased in the following weeks. In the 3 week, the correlation was 0.373, which was statistically significant. This shows that the highest correlation was seen in the 1st week. Hence, our study suggested that lorazepam challenge test is a good predictor of response in the 1st week alone. We observe negative correlation which is significant in the 3rd week (P = 0.048) and not in the 1st and 2nd week.
Conclusion:
Our study analyzed the patients with catatonia in psychiatric diagnostic categories, history, and the outcome after treating them with lorazepam at every visit over 3 weeks. The correlation in the level of improvement of symptoms at subsequent visits was noteworthy and had a strong association with the lorazepam challenge test. When dose of lorazepam was tapered, on an average dose was reduced in the 2nd week. Suggesting that at least 3 week treatment would be ideal.
Keywords
Catatonia
Benzodiazepines
Lorazepam challenge test
INTRODUCTION
Catatonia is a clinical syndrome characterized by bizarre motor behavior and disturbances in volition. In his article “Die Katatonie: Or das Spannungsirresein, eine klinische Form psychischer Krankheit,” published in 1874, Kahlbaum provided the first detailed description of the condition.[1] This view always had its critics who observed the presence of catatonic symptoms in patients who did not fit into the diagnostic criteria of schizophrenia. However, the association of catatonia with schizophrenia continued till 2013, when the Diagnostic and Statistical Manual of Mental 5 (DSM-5) finally coded catatonia as a separate clinical entity and added specifiers in various diseases to denote the presence of catatonic symptoms.
Recent studies have shown that there is a greater prevalence of catatonic symptoms in patients suffering from mood disorders as compared to those suffering from schizophrenia and other related disorders.[2] There has been evidence that the symptoms of catatonia are related to the underlying psychopathology. Stereotypy, posturing, negativity, automatic obedience, and waxy flexibility are among the abnormal movements and mannerisms that patients with schizophrenia are more likely to exhibit; in contrast, catatonic excitation, and catatonic retardation are more common in patients with mania and depression, respectively.[3]
The Bush-Francis Catatonia Rating Scale [often abbreviated as BFCRS], the most widely used diagnostic tool for assessing catatonia, only needs two of its first 14 items to be present to confirm a diagnosis of catatonia.[4] This scale also helps in measuring the severity of the symptoms.
Over decades, the everchanging views on diagnostic criteria and the actual prevalence illuded the clinicians by the fact that catatonia was a relic of the past and the advances in antipsychotics had led to its total extinction in the modern era. However, majority of the studies cross-examined the reliance and harbored the fact that it was merely underdiagnosed.[5,6]
Catatonia is a complex neuropsychiatric disorder and if not diagnosed in the earlier phase can cause serious and even lethal complications. By and large, patients with catatonia have shown exceptional response to benzodiazepines (BZDs) particularly lorazepam and electroconvulsive therapy (ECT).[7-9] There is a limited evidence on the effectiveness of only BZDs for a prolonged period as studies have highlighted its benefits during the initial few hours to days and have emphasized the ECTs as an alternative treatment option for desirous results.[8]
According to studies, the effects of lorazepam wear off after few hours, and the symptoms then come back.[10,11] However, in this study, we tried to track the efficiency of lorazepam over a long length of time in treating catatonia symptoms, as well as the relationship between the test’s reaction and the symptoms’ improvement over time.
MATERIALS AND METHODS
This study was done from September 2020 to September 2021 which was a retrospective and observation study.
Inclusion criteria
All patients diagnosed with catatonia as per the DSM-5 either visited the outpatient department or had indoor management from September 1, 2020, patients whose records were available for at least three subsequent follow-ups, and patients who were treated exclusively with lorazepam were included in the study.
Exclusion criteria
Patients with the organic cause of catatonia, patients with catatonia who were started on ECTs, and patients who had a history of being prescribed BZDs 2 weeks before presenting to the outpatient department were excluded from the study.
After the ethical approval from IEC, we acquired the hospital records from September 2020 to September 2021. A total of 38 patients with catatonia visited the psychiatry department. Further, a total number of 31 patients were selected for the final study. We accessed their records and noted their history, predominantly the duration of current symptoms, total duration of illness, and history of catatonia. We also noted the BFCRSs on record for every visit and the dose of lorazepam that was administered. The details were tabulated and then analyzed through Statistical Package for the Social Sciences software version 26.0.
RESULTS
Sociodemographic details
[Table 1] shows distribution of socio-demographic variables of the patients. From the sample, 19 were males and 12 were female. The mean age of 25.71 years for bipolar disorder, 28.67 years for MDD, 17 years for brief psychotic episode, and 27.5 years for Schizophrenia. Regarding occupational status, nearly 61.3% of patients were unemployed.
| Bipolar disorder | MDD | Brief psychotic episode | Schizophrenia | Chi-square/ANOVA | |
|---|---|---|---|---|---|
| Age | 25.71 (SD=8.09) | 28.67 (SD=4.13) | 17.00 (SD=1.00) | 27.50 (SD=8.85) | 0.163 |
| Gender | 0.203 | ||||
| Male | 6 | 4 | 3 | 6 | |
| Female | 8 | 2 | 0 | 2 | |
| Education | 7.86 (SD=3.72) | 6.50 (SD=5.12) | 8.33 (SD=3.51) | 6.62 (SD=3.85) | 0.820 |
| Occupation | 0.002 | ||||
| Unemployed | 7 | 4 | 0 | 7 | |
| Unskilled | 2 | 1 | 1 | 1 | |
| Semiskilled | 5 | 1 | 0 | 0 | |
| Student | 0 | 0 | 2 | 0 | |
| Past history | 0.033 | ||||
| No | 4 | 5 | 3 | 3 | |
| Yes | 10 | 1 | 0 | 5 | |
| History of Catatonia | 0.275 | ||||
| No | 12 | 4 | 3 | 8 | |
| Yes | 2 | 2 | 0 | 0 | |
| Family history | 0.840 | ||||
| No | 9 | 5 | 2 | 6 | |
| Yes | 5 | 1 | 1 | 2 |
MDD: Major depressive disorder, ANOVA: Analysis of variance, P value < 0.05
Clinical and psychiatric history
Among the 31 patients, 45.16% (n = 14) Mania; 19.35% (n = 6) depressive disorder, 9.68% (n = 3) brief psychotic disorder, and 25.80% (n = 8) had schizophrenia [Figure 1].
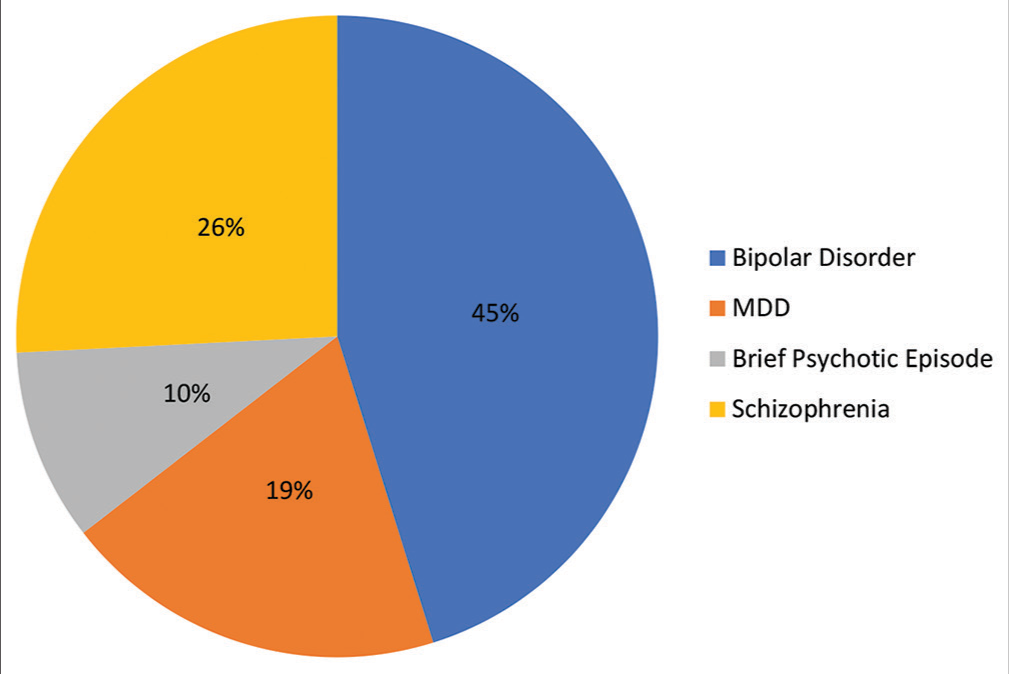
- The primary psychiatric diagnosis in the patients presented with catatonia.
The clinical improvement of symptoms in subsequent follow-ups
[Table 2] shows the score of BFCRS at four subsequent visits in all the groups of disorders. Repeated analysis of variance measures show a significant difference in the scores of BFCRS obtained over time (P = 0.00). There was no other significant finding with regards to the diagnosis, time duration, and response to the treatment (P = 0.216).
| Mania | Depression | Brief psychotic episode | Schizophrenia | Repeated measures ANOVA (Over Time) | Repeated measures ANOVA (Time×Diagnosis) | |
|---|---|---|---|---|---|---|
| Visit 1 | 14.79 (SD=3.12) | 11.33 (SD=2.88) | 14.67 (SD=4.04) | 13.13 (SD=3.27) | 0.000 | 0.216 |
| Visit 2 | 7.43 (SD=3.59) | 5.33 (SD=4.48) | 6.67 (SD=1.15) | 8.63 (SD=2.92) | ||
| Visit 3 | 4.14 (SD=3.48) | 3.50 (SD=3.21) | 5.33 (SD=2.31) | 5.50 (SD=3.21) | ||
| Visit 4 | 2.00 (SD=2.75) | 2.17 (SD=1.33) | 2.67 (SD=2.31) | 3.13 (SD=2.75) |
BFCRS: Bush-Francis Catatonia Rating Scale, ANOVA: Analysis of variance. P value significant at <0.05
Associations
No sociodemographic parameters were found to be significantly associated with the nature of illness except the occupational status (P = 0.002). Interestingly, both the family history (P = 0.840) and any history of catatonia in past (P = 0.275) were not significantly associated with the psychiatric diagnosis. Patients had a measurable improvement in their catatonic features [Figure 2].
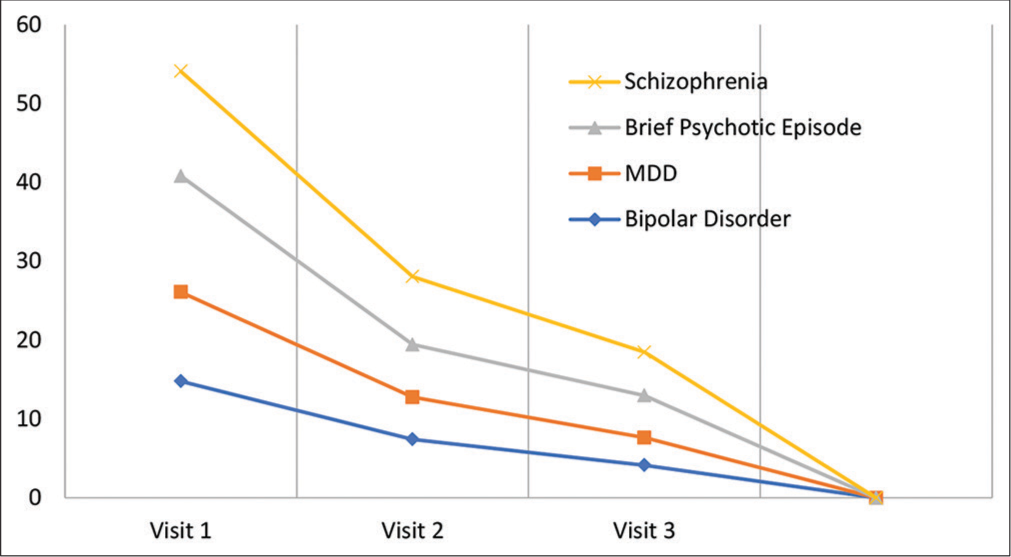
- The reduction in the Bush-Francis Catatonia Rating Scale scores over the course of treatment with lorazepam.
[Table 3] shows the correlation between improvement in BFCRS after lorazepam challenge test and improvement in BFCRS scores after oral lorazepam in the following weeks. on calculating the difference in the total BFCRS scores at the following visits the patients showed slow response over time, that is, the difference in the score at visits 1 and 2 is greater than that of the visit 1 and visit 4.
| Pearson correlation | 2-tailed significance | |
|---|---|---|
| Between lorazepam challenge and Visit 2 | 0.604 | 0.000 |
| Between lorazepam challenge and Visit 3 | 0.473 | 0.007 |
| Between lorazepam challenge and Visit 4 | 0.373 | 0.039 |
| Lorazepam dose in 1st week versus Improvement after 1st week | −0.185 | 0.319 |
| Lorazepam dose in 2nd week versus Improvement after 2nd week | −0.473 | 0.614 |
| Lorazepam dose in 3rd week versus Improvement after 3rd week | −0.373 | 0.048* |
In [Table 3], we see correlation between the dose of lorazepam and improvement in catatonia symptoms. Here, we observe negative correlation which is significant in the 3rd week (P = 0.048) and not in the 1st and 2nd week.
DISCUSSION
In our hospital records in the stipulated time, we found a total of 38 patients that fulfilled the diagnostic criteria for catatonia as per DSM-5.[12] of those two were started on ECTs as they had refusal to eat and one had serious neurological symptoms and was referred to a Neurology unit on an urgent basis however our final data comprised of 31 patients after eliminating a few who did not satisfy the inclusion criteria. Among these patients, bipolar disorder was the most common primary diagnosis. About 10% of psychiatric patients have catatonia, which has been seen to be more common in those with mood disorders than in people with schizophrenia.[13]
In the analysis of the sociodemographic variables, only the variables for the occupational status of patients came out to be statistically significant. A study on etiological factors concluded that catatonia was more common in females preferably housewives, low educational levels, urban population, Hindu religion, and patients from urban areas.[14] Almost equal prevalence in both married and unmarried groups is suggestive of no significant role of marital status.
However, a more in-depth evaluation is required to announce occupational status as one of the risk factors for catatonia. Some existing studies suggested that cognitive deficits could be a cause of unemployment or occupational inefficiency in patients with recent-onset psychosis.[15] According to a 20-year follow-up of the Suffolk County Mental Health Project, people with bipolar illness were more likely than people with schizophrenia to have meaningful employment and an independent lifestyle. Negative symptoms, obesity, and chair stand performance were significant contributors to the impairment of occupational status and quality of life in schizophrenia patients, whereas depression was a significant predictor of employment outcomes in bipolar disorders.[16,17]
Reasonable evidence aided to the fact that BZDs and ECT can treat catatonia explicitly. However, eventually identifying the underlying cause and the adequate treatment plan is the mainstay of long-term management. As per some Asian studies, the percentages of response and remission fall between 0% and 100%[13,18] and that in Indian population lies between 17% and 100%.[19,20] As per the studies, the cases which are diagnosed as catatonia under evaluation on admissions and get better with BZDs or ECTs without any underlying diagnosis are best treated with atypical antipsychotics. Avoid prescribing first generation antipsychotics (FGAs) to curtail the risk of extrapyramidal side-effects and neuroleptic malignant syndrome. Few studies mentioned the therapeutic efficacy of carbamazepine, 17,18 N-methyl-D-aspartate (NMDA) antagonist amantadine.[18,20]
In our study, we came across the fact that while there was a significant reduction in the BFCRS scores of patients while they were being given Lorazepam; however, no correlation was observed between the underlying diagnosis and treatment outcome. In contrast, numerous studies had reported poor response to BZDs with catatonia in chronic schizophrenia.[21] Coming to the dose of lorazepam, ranging from 12 mg to 24 mg is recommended to obtain complete remission.[22] Lower doses (3−6 mg) were found to be ineffective and the patient is then prescribed ECTs or antipsychotics which might have a delay in recovery.[23,24] Other factors such as biological framework, severity, chronicity of illness, drug compliance, frequency of evaluation, and duration of the study conducted should be also taken into consideration before commenting on the treatment results.[25] Exact duration of treatment with lorazepam is difficult to assess.
When the correlation in the response to the “Lorazepam Challenge Test” and overtime improvement on BZDs was found out to be statistically significant, it is not wrong to state that the “Lorazepam Challenge Test” is a good predictor while deciding the management for the patients with catatonia. A randomized, double-blind, placebo-controlled, and cross-over study successfully claimed that the “Lorazepam Challenge Test” was an indicator of Lorazepam sensitivity.[24] We found that the lorazepam challenge test versus improvement after 1 week of oral lorazepam had Pearson’s correlation of 0.604, this correlation decreased in the following weeks. In the 3rd week, the correlation was 0.373, which was statistically significant. This shows that the highest correlation was seen in the 1st week. Hence, our study suggested that lorazepam challenge test is a good predictor of response in the 1st week alone [Table 3].
Findings of [Table 3] suggest that patient requires at least 3 weeks of lorazepam treatment for persistent improvement in catatonia symptoms. The dose of lorazepam was reduced in the 2nd week and is shown by the negative correlation in the 3rd week (−0.373) with P < 0.05. Even after lowering the lorazepam dosage at the end of the 2nd week, the response persisted at the end of the 3rd week, demonstrating that even after the dose is lowered, the improvement persisted in the subsequent period of time.
Limitations
The sample was small in number and represented a single tertiary care setting. Long-term data were not available (more than 1 month).
CONCLUSION
To summarize, catatonia is a serious neuropsychiatric condition with a terrific prognosis if diagnosed at a primary stage and treated vigorously. Our study results showed an incredible response in the patients with catatonia only on lorazepam despite their distinct psychiatric diagnosis. We strongly support the effectiveness of other treatment options such as ECTs, Antipsychotic drugs (APDs), zolpidem, carbamazepine, and NMDA antagonist (Amantadine) but after an adequate trial with BZDs preferably lorazepam. If a patient had no or minimal response with BZDs, ECTs are the next best treatment modality and to be started without much delay. A trial of at least 3 weeks can be given when the lorazepam challenge test gives good result. It is recommended to continue lorazepam for at least 3 weeks to have a sustained improvement in their catatonia symptoms.
Declaration of patient consent
The authors certify that they have obtained all appropriate consent.
Conflicts of interest
There are no conflicts of interest.
Financial support and sponsorship
Nil.
References
- Die Katatonie: Oder Das Spannungsirresein, Eine Klinische form Psychischer Krankheit (1st ed). Berlin: Hirschwald; 1874.
- [Google Scholar]
- Comparison of catatonia presentation in patients with schizophrenia and mood disorders in Lagos, Nigeria. Iran J Psychiatry. 2011;6:7-11.
- [Google Scholar]
- Factor analysis of the catatonia rating scale and catatonic symptom distribution across four diagnostic groups. Compr Psychiatry. 2003;44:472-82.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of the catatonic syndrome in an acute inpatient sample. Front Psychiatry. 2014;5:174.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia: Disappeared or under-diagnosed? Psychopathology. 2005;38:3-8.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia in clinical reality: Underdiagnosed and forgotten. MMW Fortschr Med. 2019;161(Suppl 7):7-11.
- [CrossRef] [Google Scholar]
- Phenomenology and treatment of Catatonia: A descriptive study from north India. Indian J Psychiatry. 2011;53:36-40.
- [CrossRef] [PubMed] [Google Scholar]
- Response rate of lorazepam in catatonia: A developing country's perspective. Prog Neuropsychopharmacol Biol Psychiatry. 2010;34:1520-2.
- [CrossRef] [PubMed] [Google Scholar]
- A clinical review of the treatment of catatonia. Front Psychiatry. 2014;5:181.
- [CrossRef] [PubMed] [Google Scholar]
- Benzodiazepines in the treatment of catatonic syndrome. Acta Psychiatr Scand. 1994;89:285-8.
- [CrossRef] [PubMed] [Google Scholar]
- Lorazepam as an adjunct in the treatment of catatonic states: An open clinical trial. J Clin Psychopharmacol. 1990;10:66-8.
- [CrossRef] [PubMed] [Google Scholar]
- Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Publishing; 2013.
- [CrossRef] [Google Scholar]
- Catatonia in a psychiatric intensive care facility: Incidence and response to benzodiazepines. Ann Clin Psychiatry. 2000;12:89-96.
- [CrossRef] [PubMed] [Google Scholar]
- Determinants of occupational outcome in recent-onset psychosis: The role of cognition. Schizophr Res Cogn. 2019;18:100158.
- [CrossRef] [PubMed] [Google Scholar]
- Comparison of psychotic bipolar disorder, schizoaffective disorder, and schizophrenia: An international, multisite study. Acta Psychiatr Scand. 2016;133:34-43.
- [CrossRef] [PubMed] [Google Scholar]
- Prediction of real-world functional disability in chronic mental disorders: A comparison of schizophrenia and bipolar disorder. Am J Psychiatry. 2010;167:1116-24.
- [CrossRef] [PubMed] [Google Scholar]
- Maximal response to electroconvulsive therapy for the treatment of catatonic symptoms. J ECT. 2007;23:233-5.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia in psychiatric classification: A home of its own. Am J Psychiatry. 2003;160:1233-41.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia in psychotic patients: Clinical features and treatment response. J Neuropsychiatry Clin Neurosci. 2011;23:223-6.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment use in a prospective naturalistic cohort of children and adolescents with catatonia. Eur Child Adolesc Psychiatry. 2015;24:441-9.
- [CrossRef] [PubMed] [Google Scholar]
- Catatonia in psychiatric illnesses In: The Medical Basis of Psychiatry. Netherlands: Springer; 2016. p. :517-35.
- [CrossRef] [Google Scholar]
- Catatonia as a risk factor for the development of neuroleptic malignant syndrome: Report of a case following treatment with clozapine. World J Biol Psychiatry. 2009;10:70-3.
- [CrossRef] [PubMed] [Google Scholar]
- Lorazepam for chronic catatonia: A randomized, double-blind, placebo-controlled cross-over study. Psychopharmacology (Berl). 1999;142:393-8.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation and treatment of catatonia. Am J Psychiatry. 1989;146:553-4.
- [CrossRef] [PubMed] [Google Scholar]






