Translate this page into:
The Current State of Rural Neurosurgical Practice: An International Perspective
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Rural and low-resource areas have diminished capacity to care for neurosurgical patients due to lack of infrastructure, healthcare investment, and training programs. This review summarizes the range of rural neurosurgical procedures, novel mechanisms for delivering care, rapid training programs, and outcome differences across international rural neurosurgical practice.
Methods:
A comprehensive literature search was performed for English language manuscripts with keywords “rural” and “neurosurgery” using the National Library of Medicine PubMed database (01/1971–06/2017). Twenty-four articles focusing on rural non-neurosurgical practice were included.
Results:
Time to care and/or surgery and shortage of trained personnel remain the strongest risk factors for mortality and poor outcome. Telemedicine consults to regional centers with neurosurgery housestaff have potential for increased timeliness of diagnosis/triage, improved time to surgery, and reductions in unnecessary transfers in remote areas. Mobile neurosurgery teams have been deployed with success in nations with large transport distances precluding initial transfers. Common neurosurgical procedures involve trauma mechanisms; accordingly, training programs for nonneurosurgery medical personnel on basic assessment and operative techniques have been successful in resource-deficient settings where neurosurgeons are unavailable.
Conclusions:
Protracted transport times, lack of resources/training, and difficulty retaining specialists are barriers to successful outcomes. Advances in telemedicine, mobile neurosurgery, and training programs for urgent operative techniques have been implemented efficaciously. Development of guidelines for paired partnerships between rural centers and academic hospitals, supplying surplus technology to rural areas, and rapid training of qualified local surgical personnel can create sustainable feed-forward programs for trainees and infrastructural solutions to address challenges in rural neurosurgery.
Keywords
Access to care
feasibility
mobile neurosurgery
neurosurgical training
resource allocation
rural neurosurgery
telemedicine
time to surgery
INTRODUCTION
Rural and low-resource areas across the developing world have diminished capacity to care for neurosurgical patient's due to lack of infrastructure, health-care investment, and training programs. Nearly 2 billion people worldwide lack access to even basic surgical services – this problem is compounded when examining the specialized technology necessary for neurosurgical procedures.[1] In 2009, 6.8 million people died from neurological disease including traumatic brain injury (TBI), neurodegenerative disease, and congenital conditions – a number approximating the mortality burden from acquired immunodeficiency syndrome, tuberculosis, and malaria combined. The global economic burden of neurological disease is estimated at 12.3 trillion United States (US) dollars between the years 2015 and 2030 and is rising.[2] Hence, a stable, well-equipped, and well-funded neurosurgical practice and teaching infrastructure is critical to the long-term survival of any health-care system.
Regions in the developing nation have a median ratio of about one neurosurgeon for every 100,000 people;[3] the US ratio is 1:63,000.[4] This ratio drops to one neurosurgeon for every 3,000,000 people in low-income countries; the North Eastern Indian ratio is 1:2,500,000, and the African ratio is 1:4,000,000.[356] Undersupply of neurosurgeons to rural areas is an ongoing issue[367] unsurprisingly neurosurgical capacity is centralized in metropolitan regions, leaving sparse quality and access to rural neurosurgical care.[8] Some factors that prevent surgeons from entering rural practice include lack of preparation for the types of cases presenting to rural regions, compounded by lack of resources, technology, and personnel support required to effectively manage such cases.[9] The dilemma of operating on emergent cases, a large proportion comprising traumatic injuries[6] where “time is brain and/or spine,” beyond a neurosurgeon's current skill set is an additional factor barring the entry of younger trainees to the rural setting. On the other hand, rural neurosurgery is not without promise, as the opportunities of clinical triage, surgical management, and critical decision-making can provide rapid training in a relatively condensed timeframe for the motivated and well-supported trainee – hence worthy of further characterization.
The difference in resources and access significantly hinder successful neurosurgical outcomes in rural areas compared to their urban counterparts. Due to the disproportionate distribution of neurosurgical specialists, prehospital transport times are often shorter for patients in metropolitan areas whereas a larger proportion of the rural patients die before reaching advanced medical care.[10] While this may serve as a reason for higher rates of mortality in rural neurosurgical centers, a lack of literature explores this to any detail.[11] The aim of this review is to highlight the common neurosurgical procedures performed in rural settings worldwide, and to evaluate differences in outcome between rural and metropolitan neurosurgical care, to inform infrastructure development, resource allocation, and international awareness for a sustainable and evolving international rural neurosurgical practice.
METHODS
Study selection
The literature search was performed using the National Library of Medicine, PubMed database. To guide our search, we hoped to study all English language manuscripts with the key words “rural” and “neurosurgery” in the title or abstract. The following search criteria were used “([Rural (Title/Abstract)] AND Neurosurgery [Title/Abstract]) AND English (Language).” This search yielded 47 unique articles. Three study authors (P.S.U., J.K.Y., J.Y.) independently reviewed each article and associated references to determine their relevance to the practice of rural neurosurgery, indications for neurosurgical intervention, common neurosurgical procedures, technological advancements, comparative outcomes, or guidelines for emerging approaches. Any discrepancies for determining article inclusion/exclusion were adjudicated by the senior author (J.D.C.).
Of the 47 total articles, 23 were excluded due to inapplicability to the focus of the current study (18 lacked focus on neurosurgery, 3 unrelated to neurosurgical diagnoses, 1 focused on nonrural practice, 1 was purely historical). A total of 24 manuscripts were selected based on the inclusion criteria [Figure 1].
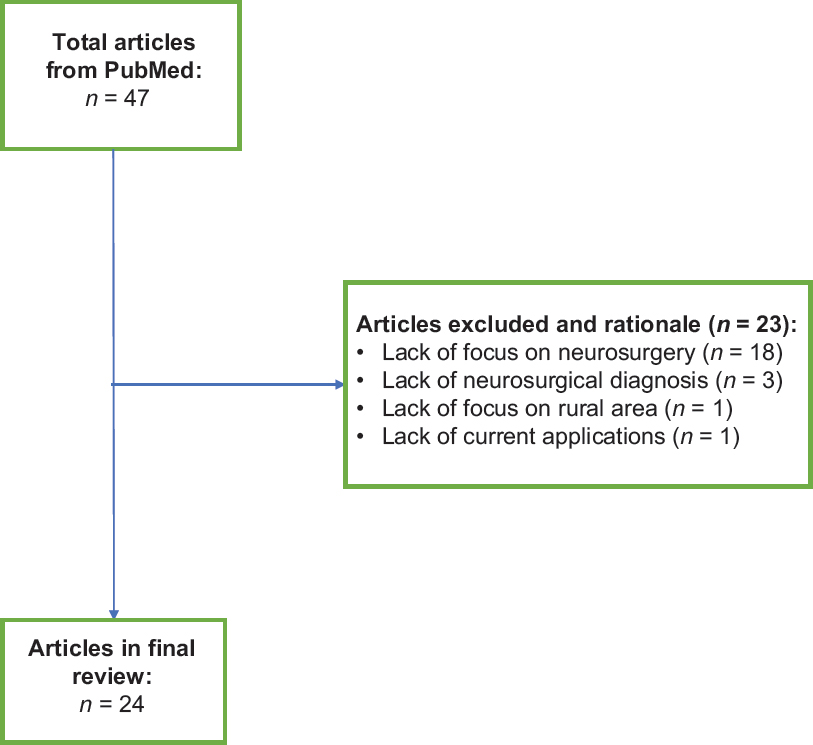
- Flow diagram of included articles
RESULTS
Practice and challenges of rural neurosurgery
Many successful neurosurgical programs exist in the developing world – our aim is to highlight common elements, successes, and challenges faced by these programs. India and Australia presents two prototypical cases for the successes and challenges facing rural neurosurgery over the last 40 years.
Ganapathy et al. outline the particular challenges faced by India's neurosurgical system. Since 1961, India has institutionalized a doctorate in neurosurgery program for students with either a Master's level training in surgery (e.g., surgery residents) to be completed in 3 years, or a Bachelor's of Medicine and Bachelor's of Surgery (MBBS; e.g., medical students) to be completed in 5–6 years.[8] Of 330 recognized medical colleges in India, 59 now have neurosurgery training programs for a total of 1800 neurosurgeons nationwide. However, with 190 new graduates each year serving a population of 1.2 billion, large areas of the country are devoid of neurosurgical practice. Despite this shortage, urban health centers such as the Apollo Hospitals (Chennai, India) and the India Institute of Medical Science (Delhi, India), deemed “centers of excellence,” offer proficient services across all neurosurgical procedures from endovascular neurosurgery to stereotactic radiosurgery. The immense wealth difference and geographical distance between rural and urban populations, however, has limited the accessibility of these centers to subpopulations living in specific locales. An estimated 800 million Indians living in suburban/rural areas have limited access to general neurosurgery as a vast majority of India's 1800 neurosurgeons live in urban centers such as Delhi, Mumbai and Chennai.[8]
This lack of access is not unique to the developing world. Byrne et al. describe a prospective study in Cook County, Illinois (US) from 01/2005 to 02/2005. As many as 66% of neurosurgical transfers to academic institutions in this region occurred because the primary hospital had no neurosurgical coverage. This mean time to transfer patients was just over 5 h with close to 10% of patients experiencing a decline in Glasgow Coma Scale (GCS) scoring during transfer.[12]
These two examples highlight challenges faced by rural communities worldwide. Nevertheless, novel solutions to the major barriers to care, such as lack of well-equipped neurosurgical centers, dearth of teaching and training hospitals, low ratio of new trainees to patient population served, and long travel distances to care centers, continue to be developed and implemented as described below.
Telemedicine
In India, 80% of medical professionals live in urban areas while 70% of the overall population lives in rural areas, underscoring a paradoxical distribution of resources.[13] Ganapathy and Ravindra describe a massive effort to bridge this gap from 2000 to 2009. During this time, 75,000 telemedicine consults were completed, and the number is growing as telecommunication capabilities to rural areas have increased. Although of limited utility in emergency settings, these consults have enabled neurosurgical follow-up and case review of previously inaccessible patients, and even allowed general surgeons to evacuate subdural hematomas (SDH) remotely with confidence knowing specialist consult was readily available.[13] Zanaboni and Wootton describe the utilization of telemedicine for outpatient neurosurgical consults in Norway as reaching 2.2% of total outpatient neurosurgical consultations in 2013. At this rate, neurosurgical telemedicine consults represented the subspecialty with the highest utilization of telemedicine across Norway-which has a 75% adoption ratio of telemedicine services across all regional hospitals. The low activity necessary during consultation makes telemedical neurosurgical consultation widely applicable to the rural context.[14]
The state of New Mexico in the US faces similar issues. New Mexico has only one-third the numbers of neurosurgeons as other states with comparative population sizes, and only one Level I trauma center statewide at the University of New Mexico Hospital (UNMH). A Level I trauma center by definition has 24 h in house coverage by general surgeons along with immediate access to all specialties of surgical care.[15] To ameliorate this shortage, a web-based computer imaging program was developed for image transfer from referring hospitals to the Level I trauma center. In a retrospective study from 11/2007 to 10/2008, 39 consultations from seven referring hospitals were received by UNMH. After neurosurgeon review of case and imaging, 44% of transfers were avoided; in patients who were not being transferred, 44% received changes to management at the direction of UNMH neurosurgeons. Beyond simply improving time to surgery, this telemedicine program optimized resource utilization and medical management.[16]
Angileri et al. performed a retrospective review of 733 patients with spontaneous intracerebral hemorrhage (ICH) admitted to small peripheral hospitals in Messina, Italy between 06/2003 and 06/2011, who received telemedicine neurosurgical consultation from the University of Messina. The use of a Telbios system allowed virtual real-time analysis of standardized Digital Imaging and Communications in Medicine images, and the time between hospital admission and neurosurgical consult decreased from a mean of 160 to 38 min. Following evaluation of clinical characteristics, hematoma location, and presence/absence of mass effect, patients were promptly transfer to surgical center for treatment if indicated. Of the 733 patients, 24% were initially transferred to the University of Messina for neurosurgical evaluation and 13% received surgical evacuation at the surgical center. Of the patients not initially transferred, 3.5% had clinical deterioration and were secondarily transferred. The authors interpret this 3.5% as the group for which initial head computed tomography (CT) scan was incorrectly read, or the percent for which telemedicine consultation was insufficient.[17]
Robust, specialized, and supported application of telemedicine in countries across three continents (India, US, Italy) demonstrate the role of technological advancement in connecting remote areas with prompt neurosurgical evaluation, with often significant improvements in care quality and trajectory. This approach is complemented by the next topic: the mobile deployment of neurosurgeons.
Mobile neurosurgery
Australia's mobile neurosurgery program illustrates efforts to bridge distances between rural and metropolitan health-care centers. Australia's vast size and relatively sparse population often preclude treatment for neurosurgical cases in rural areas, as 84% and 39% of rural surgeons expect a 2- and 4-h transport time for a neurotrauma patient to a neurosurgical center.[18] A prospective study by Simpson et al. examined 153 consecutive cases of patients with head or spinal injuries in two Australian States. In this case series, they found distance to be a critical source of delay in 77% of patients with many having to travel >50 km to receive care.[19]
To address this issue, the mobile neurosurgery program utilizes road, rotary, and fixed wing vehicles to deploy a stationed board-certified medical doctor (MD) and a specialist intensive care nurse to rural areas for operation. With the program, 254 rural hospitals can reach previously inaccessible neurosurgeons, with reports of up to a 5-h reduction in neurosurgical intervention time.[20] Owler et al. describe a prospective clinical study of nine patients with acute extradural hematoma (EDH) or ICH where mobile neurosurgery decreased the mean time to operation from 6:16 h (interquartile range [IQR] 2:30–7:22 h) to 3:55 h (IQR 3:29–5:20 h), with an estimated median time saved of 3 h.[20] The study outlines in detail three cases in which time-critical emergency neurosurgery was required. Although it is uncertain if trauma was the cause of presentation, two cases outlined in detail presented with headaches to their rural clinic and one case due to TBI. Nine of nine patients who received emergency burr holes in regional and rural hospitals survived with confirmed hematoma evacuation. Eight eight achieved full neurological recovery or marked improvement in neurological deficit.[20] Certainly, outcomes would be significantly different without rapid access to the mobile unit, as patients requiring neurosurgery who were delayed by 4:46 h were more likely to die compared to those directly presented to neurosurgical service.[20] Hence, Australia's mobile neurosurgery program not only saves many presurgical hours but also moreover proves that remote urgent neurosurgical interventions can be performed timely and safely when traversing across large distances.
The Ostfold county of Norway faces similar obstacles as distance to the only neurosurgical department at Oslo University Hospital range between 45 and 160 km.[21] To mitigate the issue of distance, Hov et al. outline Norway's implementation of a mobile stroke unit (MSU) staffed with an anesthesiologist, a paramedic, and a certified paramedic nurse to make clinical diagnosis of stroke and interpret neuroimaging. With the MSU, acute ischemic stroke patients are transported directly to a regional neurosurgical care center for thrombolysis without presenting to the local hospital. In 68 prehospital brain CTs performed by the MSU, two cases exhibited high suspicion for subarachnoid hemorrhage (SAH).[21] Both patients were transported directly to the regional neurosurgical department with estimated 2–2.5 h of presurgical time saved by bypassing the local hospital and achieved full recovery of function.[21]
The mobility of care paradigms in Australia and Norway demonstrates the benefit of presurgical time saved in providing life-saving surgery and optimizing outcomes. One-third method of improving rural neurosurgical access involves training nonneurosurgical health-care workers in common uncomplicated neurosurgical procedures.
Rapid neurosurgical training programs
Ellegala et al. describe a intensive neurosurgical teaching program in Tanzania prioritizing hands-on training of MDs and paramedical personnel.[22] The teach-forward program was deployed at Haydom Lutheran Hospital (HLH) in Tanzania in 2005 and required a 6-month commitment from a trained neurosurgeon to live in the community of interest. At the time, HLH provided medical care for nearly two million people and did not have a trained MD on site. A singular non-MD medical paraprofessional worker was taught professional neurosurgical techniques by an American Neurosurgeon through hands-on bedside teaching techniques. This health professional went on to teach two more individuals (one MD and one non-MD medical paraprofessional) at the HLH these skills through the apprenticeship program. Eighteen neurosurgical procedures in 2005 increased to an average of 92 annually from 2008 to 2010. By training local health professionals who understand disease patterns to operate as neurosurgical care providers, sustainable neurosurgical practices can develop in remote areas. This study is a proof of concept than an intensive 6-month neurosurgical course can prepare nonneurosurgical MDs and health-care workers to develop proficiency with a range of common neurosurgical techniques (e.g., shunts, burr holes, hematoma evacuations, spina bifida repairs, craniotomies, laminectomies, and tumor excisions).[22]
A two-tiered neurosurgical training program was proposed in 2004 by Park and others, in which medical school graduates could become “Fellows of the College of Surgeons in Neurosurgery for East, Central and Southern Africa” after 5 years of training.[23] Park advocated for a “fast-track, competency-based” training process to increase the rate at which neurosurgeons could be deployed across the African continent while demonstrating proficiency in core surgical skills. Griswold et al., in a recent case report on the clipping of a ruptured aneurysmal SAH at the internal carotid artery bifurcation in remote Southern Iran, describes the feasibility and risks that may be encountered by two-tiered programs. In the remote setting with only a rudimentary microscope and microsurgery kit, and no ability to transfer the patient to a facility of higher care, the neurosurgeon operated based solely on a foundational understanding of anatomical landmarks. Although residents in Western programs operate on upwards of 25 aneurysms by end of training, the neurosurgeon in the Iran case had only performed 20 such surgeries. The ability to perform this complex surgery in a low resource setting highlights two facts:First, neurosurgical operations can be performed safely in rural areas, and second, any training program should involve mastery of neurosurgical anatomy. Tools such as web-based platform with 3D visualization can be utilized to train neurosurgeons to operate in challenging rural areas.[4]
Widespread adoption of such techniques to allow nonneurosurgical personnel to perform life-saving neurosurgical procedures in rural locales requires a thorough understanding of the causes of mortality in rural neurosurgery compared to urban neurosurgery. Understanding what procedures are performed in rural settings, and the outcomes associated with them will help define the problem that needs to be addressed by rural neurosurgical practice.
Common neurosurgical procedures
As described by Ellegala et al. at HLH in rural Tanzania, four neurosurgeons serve a population of 46 million individuals. A training program was instituted in 2005 with one initial neurosurgeon, and by 2010, there were four Tanzanian MDs and 10 Tanzanian medical interns on staff. During this time, 372 neurosurgeries were performed, spanning 418 procedures. The most common procedures performed were shunt-related (n = 107, 25.6%), burr hole drilling and evacuation (n = 68, 16.3%), spina bifida repair (n = 57, 13.6%), bone elevation (34, 8.1%), craniotomy and evacuation (33, 8%), laminectomy (26, 6.2%), craniotomy (n = 24, 5.7%), burr hole biopsy (n = 20, 4.7%), and tumor excision (n = 19, 4.5%). Notably, some complex procedures such as craniotomies and tumor excision were not performed until pretraining.[22] Attebery et al. describes an audit conducted at HLH of initial results from an apprenticeship program between 01/2006 and 09/2006; 51 neurosurgical patients were identified: the most common neurosurgical cases were craniotomy (n = 11), burr holes (n = 7), and skull fracture repair (n = 4) for trauma-related injuries while ventriculoperitoneal shunt (VPS) placement (n = 13), myelomeningocele repair (n = 12), and laminectomy (n = 2) were the most common nontrauma cases.[3] VPS procedures were performed by connecting standard 5-mm intravenous tubing with suture materials, and cranial vault entry was performed with a standard hand drill and makeshift gigli saw.[3] So even with minimal resources, HLH still managed to treat hundreds of patients each day.
Bishop and Drummond describe a questionnaire sent to the Australian members of the Division of Rural Surgery of the Royal Australasian College of Surgeons. With a 91% response rate, this study represents a valuable overview of the neurotrauma practice of rural surgeons. One-hundred sixty-one rural surgeons were included, 90 of which carried out approximately 600 neurosurgeries over 5 years. Overall, 37% of all procedures were burr holes, 41% were craniotomies, and 22% were intracranial pressure (ICP) monitoring.[18] These procedures were rarely performed with a neurosurgeon present, as only 28% of rural surgeons had neurosurgery training more advanced than resident level.[18] As described previously, a significant number of Australian rural neurotrauma is surgically managed by rural surgeons due to distance and total transport time to neurosurgical centers.
In a retrospective review performed by Luck et al. at the Royal Darwin Hospital (RDH) of Western Australia, 161 patients with 167 admissions underwent 195 neurosurgical procedures performed by general surgery. Of these procedures, the most common were burr holes, craniotomy, cerebral and posterior fossa craniectomy, elevation of fracture site, and external ventricular drain placement.[24]
Campbell et al. reports procedures carried out by two general surgeons at Wimmera Base Hospital (WBH) in rural Australia from 06/2004 to 06/2009. WBH services an area of 61,000 km2 for a population of 54,000 people. A total of 8336 operations were performed, 227 of which were neurosurgical (225 carpal tunnels, 2 craniotomies). The authors illustrate the feasibility and value of independently performing peripheral neurosurgical procedures in emergency situations outside the field of general surgery, to achieve excellent outcomes in rural settings, given the undersupply of Australian-trained general surgeons in rural areas.[7]
Finally, Rabiu and Komolafe describes a prospective, observational study in a Southwestern Nigerian tertiary health center from 12/2010 to 05/2012 with a catchment area is 5 million people. Overall, the hospital managed 331 patients who underwent craniotomy, tumor excision, elevation of depressed skull fractures, laminectomy for decompression, burr hole for hematoma and/or abscess drainage, spinal stabilization, VPS, and spinal tumor excision. Trauma was the leading cause of presentation as 269 patients of the 331 underwent neurosurgical procedure due to a trauma-related event.[25]
Given the large proportion of acute trauma and/or tumor-related neurosurgical procedures (e.g., craniotomy/craniectomy, burr hole, fracture elevation, and intracranial monitoring), comparing outcomes from acute and/or significant intracranial injury between rural and urban areas is of paramount importance. To understand the impact that resource shortages and truncated training have on rural neurosurgery requires a thorough comparison of outcomes between rural and urban practice.
Comparison of neurosurgical outcomes
As described above, Attebery et al. performed an internal review of HLH, a 400-bed hospital in Tanzania, which was founded in 1953 by Norwegian Missionaries and receives upward of 60% of its budget from the Norwegian Ministry of Health. Patients during a 1.5 year period starting in 01/2006 who underwent neurosurgical procedures were identified. In the beginning of this internal review, no MDs were on staff. Equipment is basic with limited supplies, and ventilation is still performed by hand. Of 51 patients, 14 (27%) were confirmed deceased, 20 (39%) were confirmed living, and 33% were lost to follow-up. Of these procedures, 18 were to alleviate cranial fracture or intracranial bleed and 33 were to revise nontraumatic diagnoses (myelomeningocele, brain lesions). Notably, rates of all-cause nosocomial infection (11.7%) and mortality following VPS (28.6%) were not significantly different from rates in Sub-Saharan Africa. Thus, rural outcomes performed comparably to metropolitan neurosurgical outcomes in resource-rich areas with more access to medically trained neurosurgeons and higher levels of equipment. Furthermore, a Chi-squared analysis comparing outcomes between US neurosurgeons and Tanzanian nonmedical surgeons found no significant difference.[3]
In a recent retrospective review by Kong et al. of 102 patients sustaining cerebral gunshot wounds from 01/2010 to 12/2014 in rural South Africa, 54% (n = 55) were urban located and directly transported to local trauma center.[26] In contrast, 46% (n = 47) were located rurally and were first transported to district hospital before referral to trauma center. Notably, the need for neurosurgery, need for Intensive Care Unit (ICU) admission, and hospital length of stay (HLOS) did not differ between rural and urban groups. There was however a significant four-fold increase in mortality (36% vs. 9%; P = 0.001) for rural patients. There also was a significant increase in mean time to hospital for rural patients (15 h vs. 6 h; P < 0.001). No differences in mean discharge GCS or median HLOS were noted.[26]
The rural tertiary center studied by Rabiu and Komolafe was the first full-time rural neurosurgery center in the southwest of Nigeria,[25] serving an estimated 5 million people without access to CT, or magnetic resonance imaging (MRI). In 331 patients who presented for neurosurgical procedures (269 trauma-related, 62 nontrauma related), most frequently following motor vehicle accidents (80.3%) and assault (7.1%), with a breakdown of 66.2% mild TBI, 14.7% moderate TBI, and 19.1% severe TBI, only 54 (16.3%) received operative interventions. Overall, 30 (9.1%) suffered an outcome of severe disability, and 30 (9.1%) died.[25]
As described previously, Luck et al. conducted a retrospective review of ICU and critical care trauma services at RDH in Western Australia where general surgeons undertake emergent neurosurgery due to travel distances exceeding 2000 km. In 161 patients who underwent emergent neurosurgical procedures between 2008 and 2013, trauma accounted for 70.8%. Evacuation of acute SDH (31%), acute on chronic SDH (19%), EDH (7%), and hydrocephalus (7%) were the most common indications for neurosurgery. Accordingly, common neurosurgical procedures included craniectomy/craniotomy and burr holes. Risk factors associated with mortality following surgery included remote location of injury, injury to operation time >24 hand neurosurgical diagnoses.[24]
Harsha et al. retrospectively reviewed outcomes for endovascular diagnostic and therapeutic procedures between 2013 and 2016 at a new rural tertiary neuro-specific hospital located in a remote region of Kerala, India. This hospital serves close to 6.5 million people across four rural districts. This facility has access to electrocardiography, X-ray, CT, and MRI. Of note, due to heat limitations procedures were scheduled a minimum of 2 h apart to allow X-ray tubes to cool down for CT angiography. Across 174 diagnostic procedures and 70 endovascular therapeutic procedures, the mortality rates were zero and 1.4%, respectively.
Guidelines
Rosenfeld et al. outline the best practices for surgeons operating in rural settings. The principle of damage control neurosurgery (DCNS), for example, minimizing brain time under pressure, focuses on reducing ICP, and prompt evacuation of intracranial hematomas and can be used in remote, military, or Level I trauma centers. Many studies document this principle in the context of EDH and SDH.[2728] Rosenfeld argues that since the majority of rural neurosurgical emergencies relate to hemorrhage or hematoma, a general surgeon with teleconsultation should be capable of decompressing the patient and buying time until further imaging or a higher level of care can be reached. DCNS thus highlights the three tenets of time to treatment, condensed neurosurgical training, and teleconsultation as critical to the future of rural neurosurgery.[29]
Haglund et al. summarizes DCNS in the setting of rural Uganda. Neurosurgical practice began in the 1960s and faced many challenges previously described, for example, lack of resources, poor training and teaching, and difficulty retaining specialists. Haglund et al. working with Duke University Medical Center (DUMC; North Carolina, US) to address these crucial issues. The philosophy focused on “4 T’s: Twinning, Technology, Training, Top-down.”[30] “Twinning” required a partnership between a rural hospital and a well-established neurosurgical teaching hospital. To address “technology,” Haglund organized refurbishment of surplus equipment and their provision to Mulago Hospital in Uganda. “Top-down” consisted of outfitting the hospital with neurosurgical equipment to positively impact all other surgical subspecialties, which was validated given a 100% increase in surgical caseload over 2 years. The collaboration between DUMC and Mulago Hospital helped create formal “Training” programs for native Ugandan neurosurgeons, who acquired expertise for sustainability of training for future trainees. Hence, the “4 T’s” guideline created a systematic and reproducible model to address the major setbacks of rural neurosurgery.[30]
DISCUSSION
Worldwide, rural neurosurgery faces numerous challenges. A skewed urban centralization of neurosurgeons, lack of access to state of the art equipment, and long travel times between rural residents and neurosurgically capable hospitals constitute the foremost key issues. However, enormous strides have been made over the past two decades. Novel and rapid training programs have increased the rate of mastery of common neurosurgical procedures, and technological advances have been implemented to bridge communications and triage across vast distances, leading to improved outcomes in rural locales to be in many instances comparable to urban treatment. Our review describes the breadth of these advancements as well as their nuances and implications for the future research and neurosurgical care.
Reduction of time and distance barriers
Time to neurosurgery and distance of transport to appropriate medical center significantly predict mortality and poor outcomes.[212426] The current literature base supports the use of field neurosurgery and employment of emergent neurosurgical techniques in rural settings by medical personnel of sufficient training, when better options, for example, airlift, rapid transport, neurosurgeon on site are unavailable. Telemedicine has demonstrated efficacy in addressing this problem of distance and time. Telemedicine consults can help provide immediate neurosurgical feedback to the rural setting and can help instruct management in real time. This is particularly helpful for emergent indications such as subdural and epidural hematomas among others emergent indications.[1317] Moreover, through outpatient telemedicine consults, neurosurgical expertise can make its way into communities heretofore unreached.[14]
Similarly, mobile neurosurgical units, as deployed in Norway and Australia, allow for initial field evaluation to be made en route to a regional hospital with neurosurgical coverage. This solution incorporates the conventional wisdom that normal healthcare operations often cost patients valuable time, which is only compounded in remote settings. The clear association between time and poor outcomes provides support for programs of mobile neurosurgery as described by Hov, Owler et al., and telemedicine to provide rapid neurosurgical consults as described by Ganapathy and Ravindra, Moya et al., Zanaboni and Wootton, and Angileri et al.[13141617] These programs work to minimize the time before neurosurgical intervention and maximize patient outcomes.
The use of different techniques to decrease time and distance between patient and neurosurgical service is crucial to addressing the challenges of rural neurosurgery. Future studies regarding application to broader settings with different geography and terrains are necessary to determine the worldwide utility of telemedicine and mobile neurosurgical deployment.
Rapid neurosurgical training programs
A second major issue is the lack of neurosurgical training programs and neurosurgeons in rural areas. Most studies in rural communities focused on general surgeons, rather than neurosurgeons, performing neurosurgical procedures. The findings outlined in the outcomes section lend credence to the proposals by Park and Ellegala et al. that describe a shorter neurosurgical training program as the solution to the dearth of neurosurgeons in rural areas.[2223] Although this is a difficult topic to study, comparable outcomes suggest these programs are an ethical method to address the lack of health-care accessibility.
Without extensive training and board-certification, Attebery et al. demonstrate comparable outcomes between non-MD personnel and US neurosurgeons. Non-MD personnel with condensed training can safely perform a variety of common neurosurgical procedures in the rural setting and can serve as the foundation for rural neurosurgical emergencies. As Bishop and Drummond demonstrated through querying the Division of Rural Surgery of the Royal Australasian College of Surgeons, up to 72% of neurosurgical procedures in rural settings were undertaken without attending level supervision. A process of efficient triage to operative care through training general surgeons in basic and emergent neurosurgical procedures may represent an elegant solution to the barrier of neurosurgical expertise in rural areas.
Common rural neurosurgical procedures and associated outcomes
The unique challenges of rural neurosurgery force surgeons to prioritize procedures that are uncomplicated and can provide immediate therapeutic benefit. Factors that would force a surgeon to operate in a resource-poor setting are important considerations. Trauma is the overwhelming mechanism of injury, most likely due to motor vehicle accidents or assault.[25] Understandably, craniotomy/craniectomy, burr hole, hematoma evacuation, and VPS were among the most common procedures from various rural communities from Australia to Sub-Saharan Africa.[32225] These procedures were critical to managing ICP and preventing irreversible neurologic deterioration. Moreover, it is possible to perform these procedures safely without advanced imaging.
Both Kong et al. and Luck et al. showed that time to neurosurgical intervention was a significant predictor of mortality and outcomes.[2426] Rabiu and Komolafe prospective study of a new neurosurgical tertiary care center in Southwestern Nigeria demonstrates a 9.1% mortality rate even without basic diagnostic and/or treatment technology, for example, CT, MRI, and mechanical ventilation.[25] This prospective trial compares favorably to published neurosurgical mortality rates (9.7%) in the Mbarara regional hospital in Uganda[31] and also compares favorably to the mortality rate of 12.5% in rural patients presenting with EDH in Southern Australia.[32] The comparable metropolitan mortality rate for EDH was also 9.7%.[32] These findings show that with basic planning, training and infrastructure, and common neurosurgical emergencies can be managed safely across both rural and regional medical centers, with similar outcomes.
Limitations
Outcomes in rural neurosurgical practice are difficult to study in an ethical manner. Major limitations of this review and the encompassed studies exist, such as small sample sizes, limited prospective studies, and unique challenges faced by various rural areas worldwide. A majority of studies delineate associations between risk factors and outcomes and/or suggest guidelines for improvement. Until formal, consensus-based guidelines are synthesized across working groups and stakeholders, and the large scale adoption of such guidelines occurs, recommendations will likely be limited to small studies in heterogenous populations. Unique challenges faced, such as transportation distances across large nations with sparse populations and access to neuroimaging in new rural centers, warrant targeted solutions which are specific to each community. Thus, another major limitation is a lack of generalizability of the current review's findings to all rural communities.
CONCLUSIONS
Protracted transport times, lack of resources and sufficient training, and difficulty retaining specialists are barriers to successful outcomes in rural neurosurgical practice. However, advances such as telemedicine, mobile neurosurgery, and training programs for urgent lifesaving operative techniques have been implemented efficaciously. Development of formal guidelines for paired partnerships between rural centers and university teaching hospitals, supplying surplus technology to rural areas, and rapid stepwise training of qualified local surgical personnel can create sustainable feed-forward programs for trainees and infrastructural solutions to address major setbacks in rural neurosurgery.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Global Surgery 2030: Evidence and solutions for achieving health, welfare, and economic development. Lancet. 2015;386:569-624.
- [Google Scholar]
- Enhancing neurosurgical education in low-and middle-income countries: Current methods and new advances. Neurol Med Chir (Tokyo). 2016;56:709-15.
- [Google Scholar]
- Initial audit of a basic and emergency neurosurgical training program in rural Tanzania. World Neurosurg. 2010;73:290-5.
- [Google Scholar]
- “To Operate” Versus “Not to Operate” in low-resource settings: Example of aneurysm surgery in rural Iran and impact of mastery of neurosurgical anatomy. World Neurosurg. 2017;100:628-31.
- [Google Scholar]
- Sources of delayed provision of neurosurgical care in a rural Kenyan setting. Surg Neurol Int. 2015;6:32.
- [Google Scholar]
- Posttraumatic Seizures in a Rural Nigerian Neurosurgical Service. World Neurosurg. 2017;104:367-71.
- [Google Scholar]
- Operative experience of general surgeons in a rural hospital. ANZ J Surg. 2011;81:601-3.
- [Google Scholar]
- Is a broadly based surgical residency program more likely to place graduates in rural practice? World J Surg. 2006;30:2089-93.
- [Google Scholar]
- Short-term outcome and differences between rural and urban trauma patients treated by mobile Intensive Care Units in Northern Finland: A retrospective analysis. Scand J Trauma Resusc Emerg Med. 2015;23:91.
- [Google Scholar]
- Neurosurgical emergency transfers to academic centers in Cook County: A prospective multicenter study. Neurosurgery. 2008;62:709-16.
- [Google Scholar]
- Adoption of routine telemedicine in Norwegian hospitals: Progress over 5 years. BMC Health Serv Res. 2016;16:496.
- [Google Scholar]
- Trauma Center Levels Explained – American Trauma Society. Available from: http://www.amtrauma.org/?page=traumalevels
- [Google Scholar]
- The impact of a telehealth web-based solution on neurosurgery triage and consultation. Telemed J E Health. 2010;16:945-9.
- [Google Scholar]
- Telemedicine-assisted treatment of patients with intracerebral hemorrhage. Neurosurg Focus. 2012;32:E6.
- [Google Scholar]
- Rural neurotrauma in Australia: Implications for surgical training. ANZ J Surg. 2006;76:53-9.
- [Google Scholar]
- Neurological injuries in South Australia: The influence of distance on management and outcome. Aust N Z J Surg. 1984;54:29-35.
- [Google Scholar]
- Mobile pediatric neurosurgery: Rapid response neurosurgery for remote or urgent pediatric patients. J Neurosurg Pediatr. 2015;16:340-5.
- [Google Scholar]
- Pre-hospital CT diagnosis of subarachnoid hemorrhage. Scand J Trauma Resusc Emerg Med. 2017;25:21.
- [Google Scholar]
- Neurosurgical capacity building in the developing world through focused training. J Neurosurg. 2014;121:1526-32.
- [Google Scholar]
- The African experience: A proposal to address the lack of access to neurosurgery in rural sub-Saharan Africa. World Neurosurg. 2010;73:276-9.
- [Google Scholar]
- Emergency neurosurgery in Darwin: Still the generalist surgeons’ responsibility. ANZ J Surg. 2015;85:610-4.
- [Google Scholar]
- Neurosurgery in rural Nigeria: A prospective study. J Neurosci Rural Pract. 2016;7:485-8.
- [Google Scholar]
- Civilian cerebral gunshot wounds in rural South African patients are associated with significantly higher mortality rates than in urban patients. Eur J Trauma Emerg Surg 2017 epub ahead of print
- [Google Scholar]
- Traumatic acute subdural hematoma: Major mortality reduction in comatose patients treated within four hours. N Engl J Med. 1981;304:1511-8.
- [Google Scholar]
- Prognosis and clinical relevance of anisocoria-craniotomy latency for epidural hematoma in comatose patients. J Trauma. 1996;41:120-2.
- [Google Scholar]
- Epidemiology and Characteristics of neurosurgical conditions at Mbarara regional referral hospital. World Neurosurg. 2017;102:526-32.
- [Google Scholar]
- Extradural haemorrhage: Strategies for management in remote places. Injury. 1988;19:307-12.
- [Google Scholar]






