Translate this page into:
Sudden death in patients with pineal cyst: Evidence from autopsy studies
*Corresponding author: Amit Agrawal, Department of Neurosurgery and Radiation Oncology, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India. dramitagrawal@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Atallah O, Kumar CR, Das S, Maurya VP, Agrawal A. Sudden death in patients with pineal cyst: Evidence from autopsy studies. J Neurosci Rural Pract 2023;14:593-8.
Abstract
Pineal cysts are usually benign, fluid-filled sacs and most pineal cysts are asymptomatic. Sudden death specifically related to pineal cysts is extremely uncommon. A literature review of the pertinent databases, including PubMed, Google Scholar, Scopus, and Web of Science, was carried out to review the existing literature describing sudden death in patients with pineal cysts. In the evaluation of 49 articles, it was found that four reports discussed the unexpected death of patients who had pineal cysts. A total of four cases of sudden death and a pineal cyst were reported. There were 75% females and a mean age of 29 (range: 20–45). Cyst size on average was 1.3 cm (1.2–1.5). In each case, the cause of death and the involvement of important brain structures were confirmed by autopsy results. A pathological analysis of the pineal region and the surrounding brain tissue revealed a variety of lesions. Vascular malformation was found in one case, adding another layer of complexity to the study of sudden death syndrome. In this research, the authors highlight the fact that patients with pineal cysts can experience serious, even fatal, complications. Increased vigilance and early detection through neuroimaging and neurological assessments are required due to the wide variety of clinical manifestations and underlying mechanisms. To explain the mechanism and enhance the management and prevention of sudden deaths associated with pineal cysts, additional research with larger sample sizes is required.
Keywords
Sudden death
Pineal cyst
Pineal gland
INTRODUCTION
The pineal gland is a small neuroendocrine gland situated at the posterior end of the third ventricle that regulates the sleep-wake cycle by producing melatonin.[1,2] Shaped like “cone of a pine tree,” pineal gland was first reported by Brastianos in 300 B.C.[3] In recent years, there has been significant interest and advances in pineal gland research considering the important role that it plays in the regulation of neuroendocrine functions including sleep-wake cycle, circadian rhythm, onset of puberty, and sexual function.[4] Pineal cysts are benign, fluid-filled sacs that originate in the pineal gland.[1,5] Most pineal cysts are asymptomatic and do not cause any health issues.[6,7] Sudden death specifically related to pineal cysts is extremely uncommon, and there is limited medical literature reporting such cases.[2,8-10] Due to their benign nature and lack of symptoms, pineal cysts are typically discovered during routine neurological imaging or at the time of autopsy. Pineal cyst incidence in the general population has been reported to range from 1.1% to 4.3% in adults.[11] While studies have shown that most cases do not pose any immediate symptoms and health risks, a small percentage of patients may exhibit signs such as persistent headaches, sensory impairment, and unconsciousness while also dying suddenly.[2,8-10] Bleeding into the cyst or rapid enlargement of the pineal body, resulting in compression of the midbrain and/or acute obstructive hydrocephalus, is both potential causes of sudden death in patients with pineal cysts.[10] Due to the pressure on the brainstem, there is a subsequent occurrence of respiratory or cardiovascular impairment that might ultimately end in fatality. Exertion, physical strain, or sexual activity can also exacerbate the compression on the midbrain, enlarge the pineal cyst, and cause sudden death.
MATERIALS AND METHODS
We conducted a comprehensive literature review of the existing literature describing sudden death in patients with pineal cysts, searching relevant databases such as PubMed, Google Scholar, Scopus, and Web of Science. The studies were selected by performing a keyword search using terms such as “sudden death,” “pineal cyst,” and “pineal gland.” It was determined that a total of 49 reports were obtained. Only four reports were found to discuss the unexpected death of pineal cyst patients. In each of the four studies, patients were included who had pineal cysts, which were only discovered following the unexpected death of the patient during an autopsy. The studies focused on patients who died suddenly and unexpectedly, with no apparent cause or indication of a life-threatening condition beforehand. The inclusion criteria for this study were research articles that were reported in the English language from the inception. Furthermore, an examination was conducted on the citations of the qualifying papers to identify any further research that had not been previously found. Following the elimination of duplicate and ineligible studies, a comprehensive examination of the full-text studies was conducted [Figure 1]. Patient sex, patient age, symptoms, histopathology, and autopsy findings were recorded. The pathological features of the pineal cysts and surrounding brain tissue were analyzed for each case.
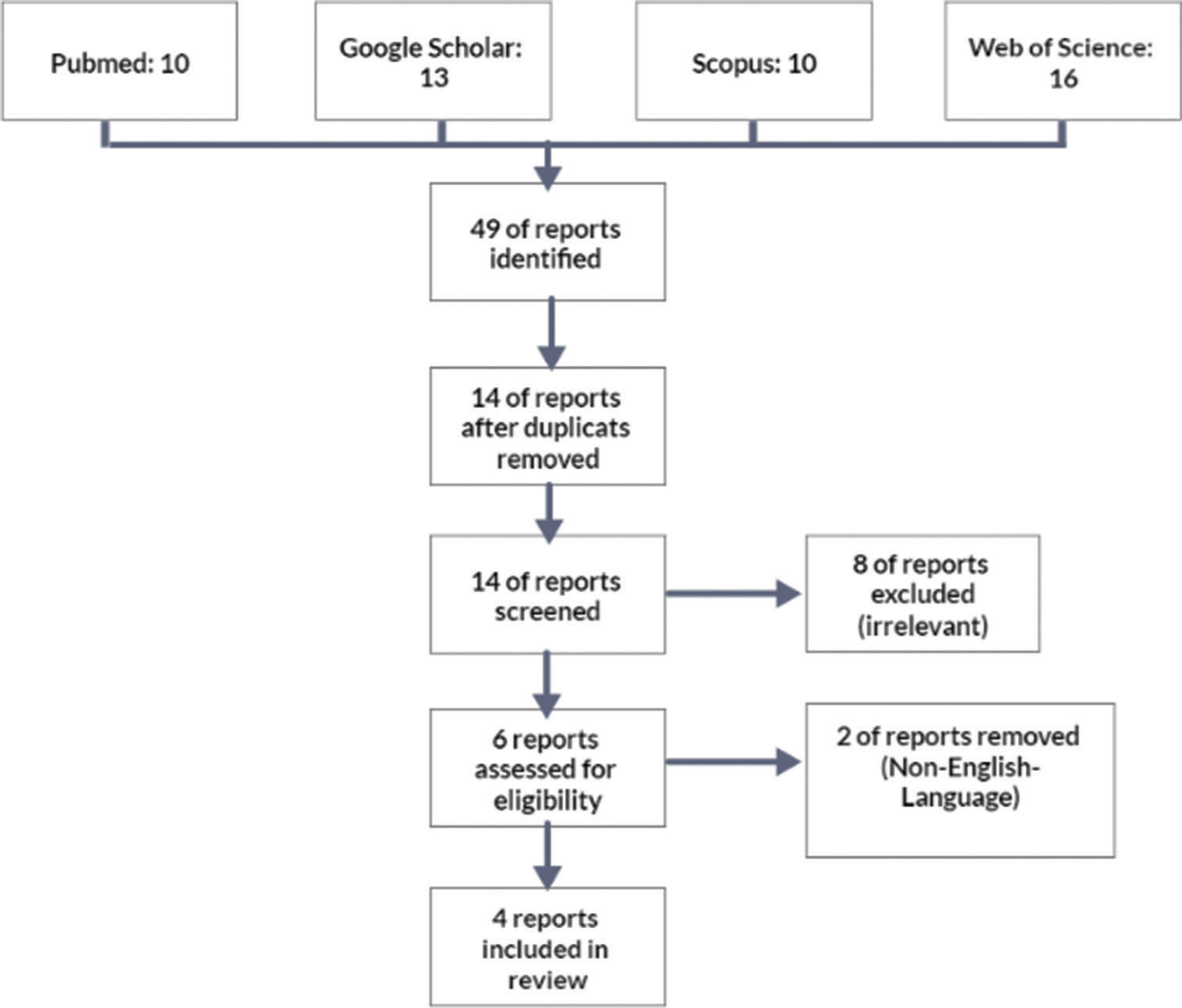
- Flow diagram of the literature review.
RESULTS
Four patients with pineal cysts who died suddenly were identified in our review.[2,8-10] The age distribution of the patients in the study spanned from 20 to 45 years, with a mean age of 29.2 years. In addition, the sample included three female participants. Remarkably, not a single patient had serious health concerns or risk factors. In the months preceding the sudden death, the headache was the most common symptom [Table 1]. The size of pineal cysts seen in the study varied between 1.2 and 1.5 cm, with an average size of 1.3 cm. Except for one case in which the pineal body compressed anteriorly the midbrain and there was also a vascular malformation, autopsies of three people showed no abnormalities in the internal organs or the brain.
| Case | Author/Year | Age | Gender | Risk factors | Clinical presentation | Cause of death | Symptoms | Duration of symptoms | Diameter | Time of death | Analysis of autopsy results | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Microscopic results | Macroscopic results | |||||||||||
| 1 | Richardson and Hirsch 1986[10] | 20 | Female | No significant medical history | Sudden death in bed | Compression of the midbrain by the pineal cyst | Previous fainting episode and headache | 3 months | 1.4 cm | Unknown | Numerous hemosiderin-containing macrophages in the cyst lining and vascular malformation | The pineal body compressed anteriorly the midbrain, producing a concave deformity in the dorsal surface of the midbrain and reducing the aqueduct of Sylvius, no abnormalities in the internal organs |
| 2 | Milroy and Smith 1996[8] | 22 | Male | No significant medical history | Collapse after a punching game | Probably due to the expansion of the pineal cyst | No previous symptoms | Not specified | 1.2 cm | Shortly after the punching game | Inner layer of glial tissue and outer layer of pineal tissue, Rosenthal fibers, no evidence of hemorrhage | No abnormalities in the brain except the pineal cyst, no external injury, no abnormalities in the internal organs |
| 3 | Na et al.2014[9] |
30 | Female | No significant medical history | Sudden death at a public toilet | Probably due to the expansion of the pineal cyst | Chronic headache | Not mentioned | 1.3 cm | Unknown | Unilocular cystic pineal lesion with glial tissue, Rosenthal fibers, calcified nodules, glial fibrillary acidic protein, synaptophysin | No abnormalities in the brain except the pineal cyst, no external injury, no abnormalities in the internal organs |
| 4 | Barranco et al.2018[2] |
45 | Female | No significant medical history | Sudden death during sexual activity | Probably due to the expansion of the pineal cyst | Chronic headache | Not mentioned | 1.5 × 2.0 cm | Direct after sexual activity | Glial tissue, proliferation of pinealocytes, microcalcifications, Synaptophysin, Glial fibrillary acidic protein-positive fibers | No abnormalities in the brain except the pineal cyst, no external injury, no abnormalities in the internal organs |
GFAP: Glial fibrillary acidic protein
First, a female individual aged 20 presenting with a pineal cyst and vascular abnormality who passed away unexpectedly in bed was described by Richardson and Hirsch in 1986. An autopsy revealed that midbrain compression may have been the cause of death. Despite having a history of headaches and fainting, the patient denied having any recent complaints. The pineal cyst was 1.4 cm in diameter. A vascular malformation in the cyst wall with evidence of a recent hemorrhage was discovered through microscopic analysis.[12] These alterations were consistent, on a macroscopic level, with a pineal cyst containing a vascular malformation.[10]
Milroy and Smith (1996) present a case involving a 22-year-old male. He had been in the middle of a boxing match when he collapsed. He showed no signs of illness and had no predisposing conditions. The pineal cyst was 1.2 cm in size. Rosenthal fibers and gliosis were found on microscopic examination. There were no obvious signs of trauma on a macroscopic level, including any abnormalities in the brain or internal organs.[8]
In the third case, which Na et al.[9] reported in 2014, a 30-year-old woman was discovered dead at a public restroom without any signs of trauma. Only chronic headaches were present in the patient’s medical history. The pineal cyst measured 1.3 cm in size. A unilocular cystic pineal lesion with glial tissue, Rosenthal fibers, and calcified nodules was discovered under a microscope. To further define the lesion, immunostaining for synaptophysin and glial fibrillary acidic protein was done. There were no abnormalities in the brain or the internal organs on a macroscopic level.[9]
In 2018, Barranco et al.[2] reported the case of a 45-year-old woman who died unexpectedly after reaching orgasm during sexual intercourse. In this case, there was no evidence of predisposing factors or disease in the patient’s past. Only a prior history of headache was present as a preexisting symptom. The cyst was 1.5 cm in size. Microscopical examination revealed glial tissue, pineocyte proliferation, and microcalcifications. There were no abnormalities in the brain or internal organs at the macroscopic level.[2]
DISCUSSION
The findings of the selected studies have generated interest and increased awareness regarding this particular topic. A complete forensic analysis revealed that cardiorespiratory failure resulting from compression of the midbrain as a result of a non-neoplastic pineal gland cyst during strenuous activities can cause sudden death.[2] These studies will examine the correlation between pineal cysts and other possible causes of sudden death. Pineal cyst-related sudden deaths are uncommon, so it is imperative that experts in forensic medicine, neuroradiology, neurosurgery, and neurology work together to determine the causes of these deaths and any associated risks.
Pineal cysts can be fatal due to the pressure that they exert on sensitive neurological structures, especially the midbrain if they grow rapidly. These cysts, especially if they are present alongside vascular malformations, can bleed and grow rapidly.[10] The reticular formation is a crucial neuronal network that controls consciousness and several cardiovascular and respiratory reflexes, and its disruption can have serious consequences such as sudden death.[13,14]
Occasionally, death can occur suddenly after engaging in certain physically demanding activities that raise intracranial pressure and exacerbate brainstem compression.[2] Some cysts, especially if they are large, cause symptoms, or are associated with vascular malformations, can be dangerous causing sudden death. Due to the rarity of reported cases and the fact that pineal cysts are often asymptomatic, their true incidence rate is unknown.
Pathological analyses elucidate the role of vascular malformations in rapid cyst expansion and the ensuing compression of vital brain structures, adding complexity to the understanding of sudden death mechanisms in these patients.[10] It is interesting that patients were frequently young and seemingly healthy, which emphasizes how sudden death associated with pineal cysts can happen without warning. Sometimes, the only symptoms were fainting or excruciating headaches, highlighting the importance of early identification and monitoring.[2,9,10] Some research has suggested a genetic or familial predisposition to the development of pineal cysts, but this is primarily based on case studies and small sample sizes. Epigenetic changes have been linked to several neurological conditions because they can change gene expression without changing the DNA sequence. They might have an impact on the differentiation and proliferation of pineal gland cells, which would help cause cysts to form. Although large-scale genome-wide association studies have not yet been carried out, they may be able to pinpoint genetic variations linked to an elevated risk of these cysts.[15] Because the pineal gland secretes melatonin, cyst formation may be related to disruption of the gland’s endocrine function. Disruptions in circadian rhythms, which melatonin plays an important role in maintaining, have been linked to several health problems. In addition, melatonin itself can regulate immune responses and has antioxidant properties.[16] Therefore, changes in melatonin production may affect the ratio of cell proliferation to cell death in the pineal gland, which may contribute to cyst development. Pineal cysts can be caused by several different variables, including genetics, epigenetics, the endocrine system, and the environment; thus, it is likely that a combination of these factors is responsible for their growth, creation, and enlargement, which can lead to brainstem compression.
Young adults appear to have a higher prevalence, suggesting that this group may be more prone to sudden, serious complications. The cysts’ physical characteristics, particularly their size, are also important. Cysts that are less severe and frequently asymptomatic are typically found by accident. Due to their mass effect and compression of the surrounding structures, larger cysts (typically >15 mm) can cause clinical syndromes, which can cause unexpected and sudden complications.[17] Another risk is the growth rate of pineal cysts, which is not fully understood. Some cases relate sudden death to rapid cyst expansion, primarily brought on by hemorrhage. Chronic headaches or visual disturbances may indicate a higher risk of unexpected complications. Comorbidities, or underlying medical conditions, are also important. Due to the physiological stress induced by sexual activity, exercise, or other triggers, patients with cardiovascular diseases, arrhythmias, or undiagnosed conditions may be more susceptible to sudden death.
Multiple mechanisms involving vital brain or cardiovascular structures may contribute to the unexpected demise of pineal cyst patients. Possible causes include ventricular arrhythmias, aortic dissection, drug interactions leading to respiratory depression, midbrain compression from a pineal gland cyst, and vascular malformations resulting in an enlarged pineal gland. To effectively prevent and intervene, awareness and knowledge of these mechanisms are required. The existing studies on sudden death in patients with pineal cysts provide valuable insights and reveal several study gaps. The potential roles of other imaging modalities and long-term follow-up studies have yet to be thoroughly explored. Addressing these gaps through more extensive, comparative studies with longitudinal follow-ups and exploring genetic factors could enhance our understanding of these patients’ risk factors, mechanisms, and optimal management strategies.
Clinical implications and limitations
The results regarding sudden death in pineal cyst patients highlight the clinical significance of early detection, monitoring, and intervention. Since most pineal cysts are asymptomatic, routine brain imaging and comprehensive neurological examinations become crucial for prompt diagnosis. Age and cyst size are two examples of potential risk factors that can help with risk stratification and guide treatment choices. For patients with symptomatic cysts, routine follow-ups can help identify changes and launch prompt interventions, minimizing negative effects, and improving patient outcomes. Establishing evidence-based guidelines for treating patients with pineal cysts and lowering the risk of unexpected death requires more research. The study’s limitations include the small number of cases included in the sample. It is not possible to extrapolate these results to the entire population of people who have pineal cysts. It may be important to examine the pineal gland during autopsy procedure in cases of sudden death. Morphological changes in the neuroendocrine system of the pineal gland may be associated with various systemic conditions including diabetes, obesity, and hypertension pancreatitis.[9,18]
CONCLUSION
Our research on sudden deaths due to pineal cysts highlights the significance of thorough investigation and monitoring, especially for younger patients exhibiting symptoms due to pineal cyst. Considering the rarity of sudden deaths caused by pineal cysts and the study’s limitations, additional large-scale, and longitudinal research is required. Understanding this uncommon condition, better-stratifying patients at risk, and enhancing patient outcomes will depend critically on the ongoing investigation.
Declaration of patient consent
Patient‘s consent not required as patients identity is not disclosed or compromised.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Neuroimaging in emergency: A review of possible role of pineal gland disease. Gland Surg. 2019;8:133-40.
- [CrossRef] [PubMed] [Google Scholar]
- Sudden and unexpected death during sexual activity, due to a glial cyst of the pineal gland. Am J Forensic Med Pathol. 2018;39:157-60.
- [CrossRef] [PubMed] [Google Scholar]
- Pineal region tumors In: Primary central nervous system tumors. United States: Humana Press; 2011.
- [CrossRef] [Google Scholar]
- The pineal gland: anatomy, physiology, and clinical significance. J Neurosurg. 1985;63:321-41.
- [CrossRef] [PubMed] [Google Scholar]
- Pineal cyst: A review of clinical and radiological features. Neurosurg Clin N Am. 2011;22:341-51, vii
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic pineal cysts: Clinical manifestations and management. Acta Neurochir (Wien). 2002;144:233-42. discussion 242
- [CrossRef] [PubMed] [Google Scholar]
- Pineal cyst presenting with intracystic and subarachnoid haemorrhage: Report of a case and review of the literature. Br J Neurosurg. 1999;13:189-92.
- [CrossRef] [PubMed] [Google Scholar]
- Sudden death due to a glial cyst of the pineal gland. J Clin Pathol. 1996;49:267-9.
- [CrossRef] [PubMed] [Google Scholar]
- An autopsy case of sudden unexpected death due to a glial cyst of the pineal gland. Am J Forensic Med Pathol. 2014;35:186-8.
- [CrossRef] [PubMed] [Google Scholar]
- Sudden, unexpected death due to “pineal apoplexy”. Am J Forensic Med Pathol. 1986;7:64-8.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of pineal cysts in children and young adults. Clinical article. J Neurosurg Pediatr. 2009;4:230-6.
- [CrossRef] [Google Scholar]
- Nonneoplastic pineal cysts: A clinicopathologic study of twenty-one cases. Ann Diagn Pathol. 1997;1:11-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pineal cavernous malformations: Report of two cases. Yonsei Med J. 2005;46:851-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pineal cyst apoplexy: A rare complication of common entity. Brain Tumor Res Treat. 2020;8:66-70.
- [CrossRef] [PubMed] [Google Scholar]
- Germline and somatic mutations in the pathology of pineal cyst: A whole-exome sequencing study of 93 individuals. Mol Genet Genomic Med. 2021;9:e1691.
- [CrossRef] [PubMed] [Google Scholar]
- Melatonin for delirium prevention in hospitalized patients: A systematic review and meta-analysis. J Psychiatr Res. 2021;133:181-90.
- [CrossRef] [PubMed] [Google Scholar]
- Pineal cyst: Results of long-term MRI surveillance and analysis of growth and shrinkage rates. J Neurosurg. 2023;138:113-9.
- [CrossRef] [PubMed] [Google Scholar]
- Digital histological morphometry of the human pineal gland in a postmortem study, with endocrine and neurological clinical implications. Anat Histol Embryol. 2023;52:12-20.
- [CrossRef] [PubMed] [Google Scholar]







