Translate this page into:
Stroke outcome after domiciliary use of opioids in the peri-stroke period
Address for correspondence: Dr. Shivani Juneja, Department of Pharmacology, Maulana Azad Medical College, Bahadur Shah Zafar Marg, New Delhi - 110 002, India. E-mail: docshivani28@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Stroke affects large number of people worldwide resulting in disability. The people in the northern region of India follow some domiciliary practices, which include administration of opioids at the onset of stroke to retard its progression.
Aim:
To study the effect of opioids on the outcome and severity of stroke when used as domiciliary treatment in peri-stroke period.
Materials and Methods:
A prospective, observational study on stroke patients was carried out in Department of Neurology, Dayanand Medical College and Hospital, Ludhiana, Punjab, India from March 2012 to March 2013. Data were collected in a semi-structured proforma. The variables which were studied included socio-demographic characteristics such as age, gender, religion, socio-economic status, and place of inhabitation. The time of opioid administration, approximate amount administered, frequency of administration, duration of hospital stay, risk factors and co-morbid conditions were also studied. The stroke severity was analyzed by comparing National Institutes of Health Stroke Scale (NIHSS) score and outcome by comparing Modified Rankin Scale (MRS) score in both the groups at the time of admission and at the time of discharge.
Results:
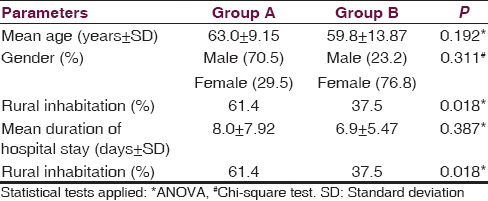
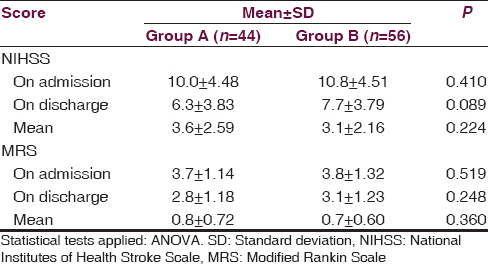
Out of n = 100 recruited patients, n = 44 (Group A) reported opioid intake in the peri-stroke period and n = 56 (Group B) did not. Proportions of patients from rural areas were 61.4% in Group A and 37.5% in Group B. Mean age in groups A and B was 63 ± 9.15 and 59.8 ± 13.87 years, respectively; in these groups male proportions were 70.5% and 60.7%, respectively. At admission, mean NIHSS scores in Groups A and B were 10.0 ± 4.48 and 10.8 ± 4.51, respectively; on discharge, these scores were 6.3 ± 3.83 and 7.7 ± 3.79, respectively. At admission, mean MRS scores in Groups A and B were 3.7 ± 1.14 and 3.8 ± 1.32, respectively; upon discharge, these scores were 2.8 ± 1.18, 3.1 ± 1.23 respectively.
Conclusion:
In this cohort, we found that the domiciliary practice of opioids administration in the peri-stroke period is more common among the elderly and in the rural areas. There was no statistically significant difference in the mean NIHSS and MRS scores at admission as well as discharge implying that the opioid administration did not improve outcome or decrease the severity of the stroke. Our findings are robust enough to propose a larger sample size and follow-up in future studies to definitively ascertain the effect of opioids as pretreatment in stroke patients.
Keywords
Domiciliary
opioids
stroke
Introduction
Stroke, a vascular disorder of the central nervous system, is the third leading cause of death worldwide.[123] The treatment is designed to reverse the tissue damage and improve the clinical outcome.[45] Even till date, it is a challenge for the clinicians to establish a therapeutic regimen that allows the patient to regain prestroke health status because of the substantial disability associated with stroke. The cost of care involved for these patients is high and have adverse social implications. Moreover, no satisfactory drugs for the primary prevention of stroke are available.[6] Therefore, a number of people in North India are following local practices in order to minimize disability.
More than one-third of the world population, particularly in Asia, is involved in the use of complementary and alternative medicine in patients with stroke and use of opioids (in the crude form) is one of them.[7] The people in some parts of India especially in the northern region, have a strong belief regarding the protective effects of opioids when given at the onset of stroke. This protection reportedly results in aborting an attack or preventing its progression. However, its use has not been scientifically evaluated. There are very few studies done with respect to the use of opioids in stroke. The current study was planned in view of the current prevalence of the use of opioids at the onset of stroke as a preadmission domiciliary practice. The study was done to assess if opioids can improve outcome or reduce the severity of stroke when administered at its onset.
Materials and Methods
Context
In Northern parts of India, it is a common practice to administer crude form of opioids at the onset of stroke with the belief that it will have protective effects. This study was undertaken to study the impact of this practice on the stroke severity and outcome.
Ethics clearance
The study was conducted after taking clearance from Institutional Ethics Committee.
Investigators
Dr. Shivani Juneja, Resident, Department of Pharmacology; Dr. Kanchan Gupta, Associate Professor, Department of Pharmacology; Dr. Monika Singla, Assistant Professor, Department of Neurology; Dr. Gagandeep Singh, Professor and Head, Department of Neurology; Dr. Sandeep Kaushal, Professor and Head, Department of Pharmacology, Dayanand Medical College and Hospital, Ludhiana.
Study design and participants
A prospective, observational study was conducted in patients with diagnosis of stroke admitted in the Department of Neurology (equipped with a stroke unit) for 1-year (March 1, 2012–March 31, 2013) after taking written informed consent.
Inclusion criteria
Patients of both gender and age >18 years presenting with stroke for the first time were recruited and followed-up in the study.
Exclusion criteria
Patients with transient ischemic attack, re-stroke and re-stroke with other co-morbidities were excluded from the study.
Patient groups
The patient recruitment flow chart is shown in Figure 1. Based upon the history of the preadmission domiciliary administration of opioids at the onset of stroke, the patients were divided into two groups. The patients with a history of opioid intake were allotted to Group A and patients with no history of opioid intake were allotted to Group B.
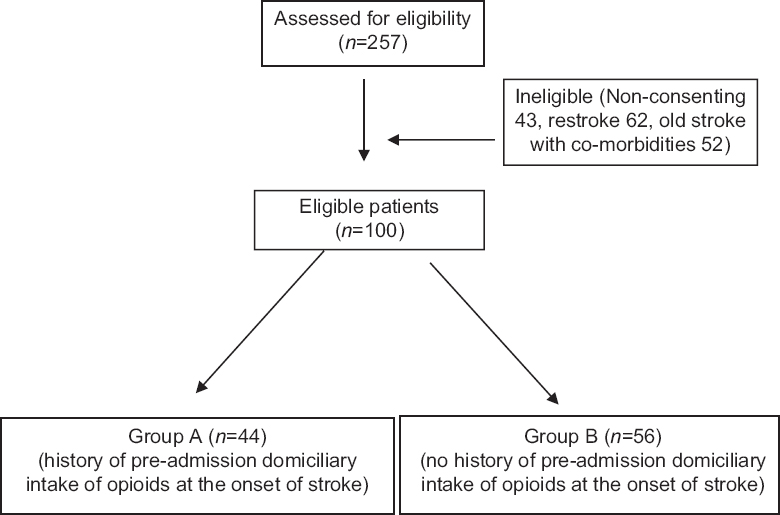
- Flow chart: Patient recruitment
Variables
The data were entered in a semi-structured proforma. The variables which were studied included socio-demographic characteristics like age, gender, religion, socio-economic status (using Kuppuswami scale based on the level of education, profession and family income) and place of inhabitation (rural or urban). The time of opioid administration, approximate amount administered, frequency of administration, duration of hospital stay, risk factors, and co-morbid conditions were also studied. The stroke severity was analyzed by comparing National Institutes of Health Stroke Scale (NIHSS) score in both the groups at the time of admission as well as at the time of discharge. The stroke outcome was analyzed by comparing Modified Rankin Scale (MRS) score in both the groups at the time of admission and at the time of discharge.[8] A decrease in NIHSS would indicate a decrease in the severity of the stroke and a decrease in MRS would indicate better outcome with the opioid administration in patients.
Statistical analysis
The continuous data like age, duration of hospital stay, NIHSS and MRS score were presented as mean ± standard deviation. The discreet data like gender, etc., was expressed as percentages and proportions. The data were analyzed using appropriate statistical tests namely unpaired t-test, Chi-square test and ANOVA. The exact P value was calculated and recorded.
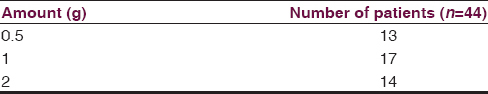
By the way of serial interviews and personal interactions with the patients and their attendants, it was found that they used the crude forms of opium which were available freely although not legal. It was mixed with various household substances such as bread crumbs, biscuits, etc., and consumed. When asked about the amount administered, the patients would tell about it in the sizes of grains rice grain, wheat grain, maize grain. Since no quantification method was available, so we weighed the same. The mixture was thus, quantified as follows: Rice grain size ~0.5 g; Wheat grain size ~1 g; Maize grain size ~2 g. However, this is an approximate method as the weight includes both that of opioid and the household substance with which it is mixed.
Results
The socio-demographic profile of patients with stroke is depicted in Table 1. In Group A, 68.2% patients were Sikhs, 29.5% were Hindus and 2.3% were Muslims whereas in Group B, 33.9% were Sikhs, 64.3% were Hindus and 1.8% were Muslims (P = 0.002). Majority of patients in both the groups belonged to lower middle socio-economic strata (52% in Group A and 53.5% in Group B) when assessed on the basis of Kuppuswami scale.
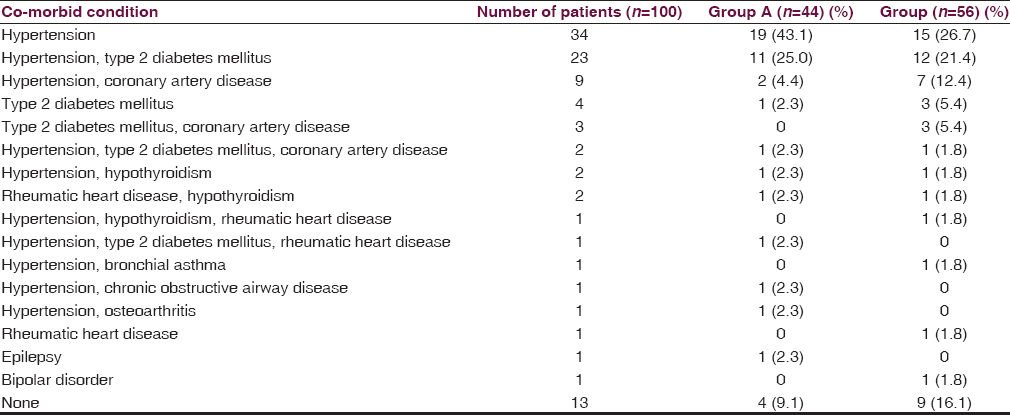
The risk factors and the co-morbid conditions in both the patient groups were also determined [Table 2]. Multiple co-morbidities were noticed in most of the patients in both the groups. Thirty-four patients had a history of alcohol intake and out of which 45.5% belonged to Group A and 25% belonged to Group B. In Group A, 4.5% patients were smokers and 7.1% patients in Group B. Six patients had a history of substance abuse in our study out of whom three belonged to Group A.
In our study, 61% patients were diagnosed as having an anterior circulation stroke, 29% as hemorrhagic stroke, 9% as posterior circulation stroke, and 1% as lacunar stroke. The amount of opioids given to the patients of stroke is shown in Table 3. The opioids were administered once in 82% patients, twice in 14% and thrice in 4% patients of Group A. In majority of patients (66%), opioids were administered within 1-h of the onset of stroke. However, the frequency and amount of opioids administered did not have any effect on the outcome. The stroke severity as evaluated on the basis of NIHSS score and the outcome by using MRS score are shown in Table 4.
Discussion
There is scarce evidence present in the scientific literature regarding the protective effect of opioids in stroke although some animal studies have implicated the opioid system in the study of brain injury and neuroprotection.[91011] A study by Kao et al. on focal cerebral ischemia/reperfusion rat model demonstrated that the opioidergic agents have a role in postischemic progression through both opioid dependent and independent mechanism.[12] Some other studies have suggested that the opioid receptor activation with opioid agonists protects the brain from ischemia or extends animal survival time during severe hypoxia.[13] Feng et al. in a study had also demonstrated that δ-opioid receptor mediated neuroprotection may have clinical importance in hypoxic-ischemic insult like in stroke.[1314]
There is only one human study by Rezvani and Ghandehari, which was done in Eastern Iran to assess if opium addiction is a probable influencing factor for ischemic heart disease (IHD) and ischemic stroke (IS). This study showed that oral opium addiction was a significant protective factor of IS (P = 0.002), but not IHD. However, the limitation of this study was that the assessment of opium dose, mean duration of opium consumption and purity of opium was not done.[15]
In our study, we found the prevalence of the use of opioids to be fairly high (44%) in the patients with stroke. The findings in our study correlate with scientific literature available, according to which stroke occurs more often in men and the risk of stroke doubles with each decade over the age of 55 years.[116] In addition to this, ours is a male dominant society and it has been seen that male gender have a better access to medical care as compared to female gender, and this may also be the reason for higher number of males presenting to our hospital. However, another study with a larger sample size would be able to provide a better indicator of true gender distribution in patients with stroke in this part of the country.
In addition, there was a higher prevalence of domiciliary use of opioids in rural areas. On evaluation of socio-economic status by using Kuppuswami scale,[17] it was seen that most of the patients with a history of opioid administration at the onset of stroke belonged to lower middle socio-economic status. The probable reason for the high prevalence of opioid use in this class in the rural areas may be attributed to low literacy levels and poor access to good medical facilities, which prompts them to use home remedies based on the local beliefs. We also observed during our study that the registered medical practitioners with inadequate medical qualification practicing in the rural areas of Indian also promote this domiciliary practice without any proven evidence of improvement in the patients with stroke.
Though the use of opioids is not legal, it is freely available and abused commonly. In a household survey of opium use by Darshan et al. in Punjab, the prevalence rate of opium use was found to be 5.76%, which was much higher among men than in women. According to the survey, the abuse of intoxicating drugs is mainly confined to alcohol, tobacco, opium, and cannabis. Among psychosocial correlates, religion was of obvious predominance. Sikh population are nonsmokers, have less incidence of tobacco abuse; but incidence of alcohol and opium abuse is higher.[18] In our study also, we found a higher prevalence of opioid use among the Sikh community (68.2%) residing in the rural areas of Punjab as compared to the Hindu and Muslim community.
The outcome (MRS) showed no statistically significant difference between both the groups on admission and on discharge. At admission, there was no statistically significant difference in NIHSS score of both groups indicating the uniform distribution of patients in both the group. At discharge also, no statistically significant difference was seen in NIHSS score of both the groups However, more studies on a larger sample size in the same direction may provide definitive evidence regarding the neuro-protective effects of opioids in patients with stroke.
The limitation of our study are the relatively small sample size, inability to follow-up to assess any difference in improvement by virtue of it being a time bound study, quantification of opioid type and dose, both of which are not based on any established criteria due to unavailability of information regarding the forms of opioids traditionally used.
After a thorough review of scientific literature and to the best of our knowledge, this is the first known study planned to substantiate and document the use of opioids in patients with stroke with a view to investigate their neuro-protective effects. However, the need for a thorough follow-up is warranted to find out long-term sequel in these patients. This was a first initiative towards this practice with an expectation that that more studies could be carried out in future on an elaborate scale and with suitable modifications.
In this report, we found a high prevalence of use of opioids in the peri-stroke period as a domiciliary practice more so in elderly and in rural areas. However, this pretreatment did not improve outcome or reduce the severity of the stroke.
Financial support and sponsorship
Nil
Conflicts of interest
There are no conflicts of interest.
References
- Cerebrovascular diseases. In: Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, eds. Harrison's Principles of Internal Medicine. New York: McGraw Hill; 2009. p. :2513-34.
- [Google Scholar]
- Stop hypertension-group. Predictors for high costs of hospital care in elderly hypertensive patients. Blood Press. 2006;15:245-50.
- [Google Scholar]
- Complementary and alternative medicine treatments among stroke patients in India. Top Stroke Rehabil. 2012;19:384-94.
- [Google Scholar]
- Clinical stroke scales. In: Herndon RM, ed. Handbook of Neurologic Rating Scales. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2006. p. :261-84.
- [Google Scholar]
- Hibernation-like state induced by an opioid peptide protects against experimental stroke. BMC Biol. 2009;7:31.
- [Google Scholar]
- The distribution and morphology of opioid peptide immunoreactive neurons in the cerebral cortex of rats. J Neurosci. 1984;4:1104-17.
- [Google Scholar]
- Opioid peptide levels in gerbil brain after transient ischemia: Lasting depletion of hippocampal dynorphin. Stroke. 1987;18:765-70.
- [Google Scholar]
- Opioids modulate post-ischemic progression in a rat model of stroke. Neurochem Int. 2008;52:1256-65.
- [Google Scholar]
- A novel insight into neuroprotection against hypoxic/ischemic stress. Sheng Li Xue Bao. 2009;61:585-92.
- [Google Scholar]
- Delta Opioid Peptide Enhances Neurogenesiis After Stroke. University of South Florida. Available from: http://www. 3.research.usf.edu/dpl/content/data/PDF/09A064.pdf
- [Google Scholar]
- Is opium addiction a risk factor for ischemic heart disease and ischemic stroke? J Res Med Sci. 2012;17:958-61.
- [Google Scholar]
- 2012 ACCF/AHA Focussed Update of the Guideline for the Management of Patients With Unstable Angina/Non-ST Elevation Myocardial Infarction: A Report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2012;126:875-910.
- [Google Scholar]
- Kuppuswamy's socio-economic status scale – A revision of economic parameter for 2012. Int J Res Dev Health. 2013;1:2-4.
- [Google Scholar]
- Drug abuse in a farm community; a brief appraisal of a research work. Drug Alcohol Depend. 1981;7:347-66.
- [Google Scholar]






