Translate this page into:
Response of Syrinx Associated with Chiari I Malformation to Posterior Fossa Decompression with or without Duraplasty and Correlation with Functional Outcome: A Prospective Study of 22 Patients
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
The aim of the study is to correlate the surgical outcome with radiological changes in patients with Chiari I malformation (CMI) with syrinx. We also compared long-term functional and radiographic outcome in CM1 patients treated with posterior fossa decompression (PFD) with or without duroplasty.
Patients and Methods:
From December 2013 to October 2015, 22 patients who underwent surgery with the diagnosis of CMI and syrinx were included in the study. Measurements were performed on preoperative and postoperative magnetic resonance (MR) scans using the same software. All patients underwent PFD with or without duroplasty. Clinical results were evaluated on the basis of the Chicago Chiari Outcome Scale (CCOS). We assessed the degree of resolution of syrinx and outcome of Chiari decompression with PFD versus PFD with duroplasty. Mean duration of follow-up was 12.4 ± 5.37 months (range: 6–24 months).
Results:
Out of 19 patients in whom syrinx diameter decreased on postoperative MR imaging, 17 (89.5%) improved based on CCOS and 2 (10.5%) were unchanged while out of three patients in whom syrinx worsened, 2 (66.7%) improved and 1 (33.3%) was unchanged (P = 0.37). The cord diameter was found to have decreased in 12 patients and of these 11 (91.7%) improved. The cord diameter increased in 10 patients, but 8 (80%) improved (P = 0.57). The mean changes in syrinx, cord, and syrinx/cord ratio were studied in both groups with and without duroplasty, were not statistically significant. In this study, radiological parameters failed to predict functional outcome.
Conclusions:
The outcome does not correlate with change in any of the syrinx-related factors. Surgical decompression with or without duroplasty does not have a statistically significant relationship in the degree of syrinx resolution. Surgical decompression without duroplasty provides the benefits of surgical decompression while avoiding the complications of intradural techniques.
Keywords
Chiari malformation
Chicago Chiari Outcome Scale
functional outcome
posterior fossa decompression
syrinx
INTRODUCTION
Chiari I malformation (CMI) is complicated by syringomyelia in about 65%–85% cases and is responsible for various manifestations of the diseases.[1] Pathophysiological mechanisms responsible for the progression of syringomyelia associated with CMI remain poorly defined and controversial.[12] Although the increase in retro cerebellar space and improvement in cerebrospinal fluid (CSF) flow has been widely accepted as the surgical goal, there is little consensus on the surgical technique used for decompression.[345] Although a subjective decrease in the syrinx size on the postoperative imaging is reassuring to the surgeon, often the size of the syrinx cavity does not correspond to clinical symptomatology.[6]
Preoperatively, presence and increase in size of cord cavities seem to go hand in hand with progressive clinical deterioration. However, interestingly, after surgical decompression, a correlation between amelioration and/or decrease in size of syrinx and clinical symptomatology is not always seen. When the cavity has not shown any decrease in size, and perhaps, the pressure inside it admittedly has not increased; however, even in these circumstances, the process of cord atrophy at best remains active, and one does not see the expected deterioration. Hence, there appears to be gaps in our understanding about worsening of the clinical condition of patients despitethe resolution of syrinx and vice-versa.
Our objective was to study the functional outcome of CMI associated with syringomyelia and to correlate the functional outcome with radiological changes in the syrinx and spinal cord. We also assessed the influence of surgical techniques on syringomyelia and cord. The possible explanations for the facts why functional outcome does not correlate with change in any of the syrinx-related factors, which at first glance seem to contradict the normal reasoning, are also discussed.
PATIENTS AND METHODS
From December 2013 to October 2015, 22 patients who underwent surgery with the diagnosis of CMI and syrinx were included in the study. Measurements were performed on preoperative and postoperative magnetic resonance (MR) scans using the same software. All patients underwent posterior fossa decompression (PFD) with or without duroplasty. Clinical results were evaluated on the basis of the Chicago Chiari Outcome Scale (CCOS).[7] The mean duration of follow-up was 12.4 ± 5.37 months (range: 6–24 months). The outcome analysis and MR imaging (MRI) study were performed during the follow-up consultation.
Assessment of syrinx and cord dimensions
Sagittal and axial images of the spine were used to calculate the diameter of the syrinx and cord. The quantitative evaluation of the syrinx diameter was done on an axial image at the level of the maximum diameter of the syrinx. A ratio of the syrinx to the cord diameter was calculated by dividing the maximum diameter of the syrinx by the diameter of the spinal cord at the same level to indirectly quantify the syrinx size in relation to cord diameter as described earlier.[8] Measurements at follow-up were obtained at the same vertebral level [Figures 1 and 2]. The change in the size of the syringomyelia in the postoperative MRI scans was classified as improved, (decreased maximum diameter), unchanged, or increased.
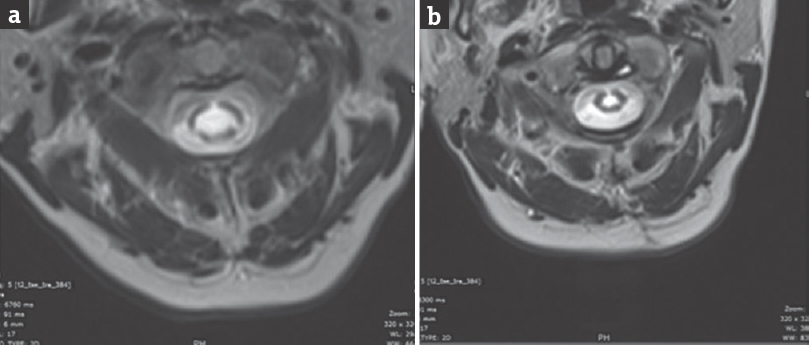
- Preoperative (a) and postoperative (b) axial images of the spine showing the diameter of the syrinx and cord
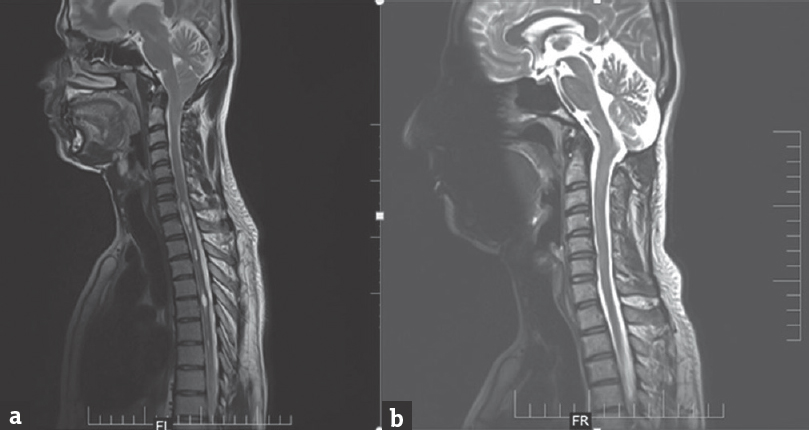
- Sagittal magnetic resonance images demonstrating a near complete reduction in the size of a holocord syrinx at 12 months postsurgical follow-up
Surgical procedure
The indications for surgical treatment were as follows: MRI confirmed CMI with syrinx and patients presented with related symptoms. All patients underwent standard 3 cm × 3 cm suboccipital craniectomy with or without duroplasty. All patients underwent uniform bony decompression. The specific surgical procedure (PFD or PFD with duroplasty [PFDD]) was chosen by each surgeon on the basis of personal preference. Of the 22 patients, 15 (68%) underwent foramen magnum decompression with duroplasty, and 7 (32%) underwent foramen magnum decompression alone.
Assessment of functional outcome
We used the CCOS[7] which is a standardized, recently, validated tool for evaluating functional outcome in CM1 patients.[9] This is a total 16-point scale consists of four categories of postoperative outcome (pain, nonpain symptoms, functionality, and complications) that are graded 1–4 which is further categorized as in improved (score: 13–16), not improved (score: 9–12), and worsened group (score: <9). To avoid the interobserver variability, all patients were graded by the same investigator.
Statistical analysis
All statistical tests were performed using IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp. (Statistical Package for the Social Sciences, Chicago). Qualitative variables were analyzed between the groups with the Chi-square test or Fisher's exact test as appropriate. Normally distributed quantitative variables were analyzed using independent samples Student t-test between the groups and paired samples t-test for within-group analysis across time points. Nonnormally distributed quantitative data and ordinal data were analyzed using the Mann–Whitney U-test for between-group comparison and Wilcoxon signed-rank test for within group comparison across time points. P < 0.05 was taken as the level of statistical significance.
RESULTS
Clinicoradiological correlations
All patients were >18-year-old, and the mean age at presentation was 31 years (31.88 ± 12.22). Gender distribution showed 1.34:1 proportion of male-to-female ratio. The mean duration of symptoms was 21 months (21.57 ± 20.47, range: 3–96 months).
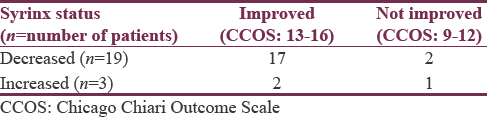
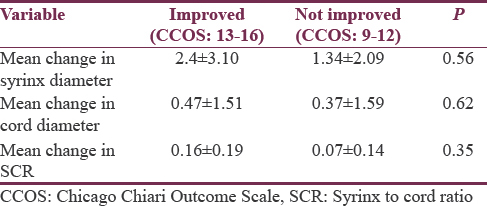
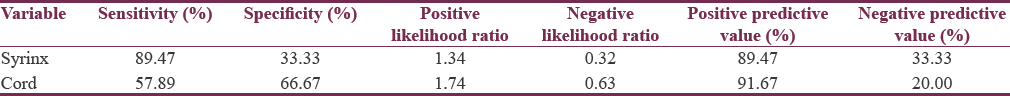
Out of 19 patients in whom syrinx diameter decreased on postoperative MRI, 17 (89.5%) improved based on CCOS and 2 (10.5%) were unchanged while out of 3 patients in whom syrinx worsened, 2 (66.7%) improved and 1 (33.3%) was unchanged (P = 0.37) [Table 1]. The cord diameter was found to be decreased in 12 patients and out of which 11 (91.7%) improved while cord diameter increased in 10 patients, but 8 patients (80%) improved (P = 0.57). We analyzed mean changes in syrinx and cord diameter, mean changes in syrinx to the cord ratio between improved and not improved patients, which were not significant statistically as shown in Table 2. We also evaluated sensitivity, specificity, and predictive value of change in syrinx and cord diameter to predict the functional outcome as shown in Table 3. In this study, radiological parameters failed to predict clinical outcome. This suggests, as seen in our series, that clinical improvement does not necessitate concurrent radiographic improvement or vice versa.
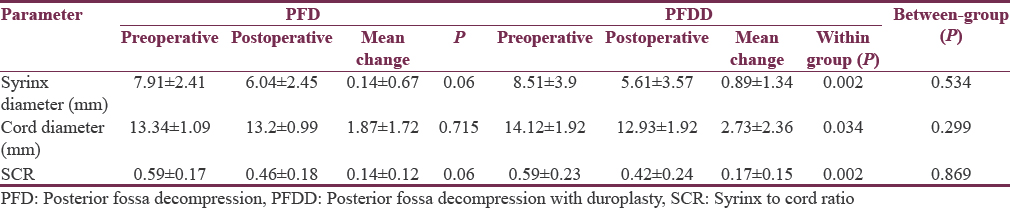
Influence of surgical technique on syrinx and cord
We found a statistically significant difference in preoperative and postoperative mean change in syrinx, cord, and syrinx/cord ratio in patients who underwent foramen magnum decompression with duroplasty (n = 15), and these changes were not significant statistically when studied in patients who underwent bony decompression alone (n = 7). However, when these parameters were studied in both groups with and without duroplasty, were not significant statistically. Our analysis suggests that performing duraplasty may lead to a greater decrease in concurrent syrinx; however, this could not be correlated to functional outcome [Table 4].
Complications
Surgical complications were assessed throughout the patient's postoperative course from the time of surgical decompression to the last clinic visit. Complications were experienced by three patients after the initial procedure. Two patients experienced CSF-related complications after surgery. One patient had a CSF leak from the operative site wound, and one developed supratentorial subdural hygromas following decompressive surgery, which was managed without any intervention. One patient had discharge from wound site which was managed conservatively. None of them had an irreversible injury after surgery. In this series, 100% of the CSF-related complications occurred after opening the dura.
DISCUSSION
The presence of syrinx is very common in CMI patients and can alter presentation and outcome. Patients with syrinx often present with more severe neurological and myelopathic symptoms.[1011] It is well established that CMI is the leading cause of syringomyelia and that the worsening of syringomyelia is one of the main causes of neurological symptoms in these patients, and the improvement or resolution of syringomyelia is one of the main aims of the surgical treatment of patients with CMI.[1213] Bogdanov and Mendelevich and Gil et al. have reported that the clinical improvement in CMI patients does not necessarily correlate with radiological improvement.[1415] Depreitere et al. in a series of 22 patients noticed a radiographic improvement in 80% of patients while 76% of patients experienced an improvement within the first 3 months after operation on the global outcome scale.[16] As per literature, inpatients with Chiari-associated syrinx incidences of radiographic improvement ranges from 44% to 100%[51718192021] while resolution or improvement of clinical symptoms ranges from to 35% to 100%.[1617192122] Furtado et al. in their study of 20 pediatric patients reported that the functional outcome does not correlate with any of the syrinx-related factors.[23] Durham and Fjeld-Olenec reported in a meta-analysis that there was no significant difference in either clinical improvement (78.6 vs. 64.6%, relative risk [RR] 1.23, 95% confidence interval [CI] 0.95–1.59) or syringomyelia decrease (87.0 vs. 56.3%, RR 1.43, 95% CI 0.91–2.25) between PFDD and PFD.[24] Although not statistically significant in the meta-analysis, some studies also show higher rates of postoperative syrinx resolution or improvement in patients undergoing PFDD.[242526] Munshi et al. in their retrospective series reported that out of seven patients who underwent only bony decompression for Chiari malformation associated with syrinx, six patients underwent follow-up MRI, 3 (50%) had a decrease in the size of the syrinx, and all three had clinical improvement. In their duroplasty group, out of 12 patients, nine underwent follow-up MRI, and all these patients (100%) had a decrease in the cavity size including eight with clinical improvement.[21] However, these previous studies had definite limitations being retrospective in nature and the methods used to report clinical outcomes were poorly defined and not based on any validated Chiari-specific outcome measure. Apart from this, most studies in this area have been conducted in pediatric patients. In a retrospective study of pediatric patients, Lee et al. found postoperative syrinx improved or resolved 10/13 in the decompression with duraplasty group compared to 8/8 in the only bony decompression group (P = 0.26) while clinical improvement defined by the mean CCOS score was comparable in patients receiving PFDD (14.7) and PFD (14.6) (P = 0.70). There was no difference in long-term clinical outcome and syrinx resolution or improvement between both groups in this study.[6]
In our cohort, we saw radiographic improvement in syrinx diameter in 86% of patients (n = 19/22). Out of 19 patients in whom syrinx diameter decreased on postoperative MRI, 17 (89.5%) improved and 2 (10.5%) were unchanged while out of three patients in whom syrinx worsened, 2 (66.7%) improved, and 1 (33.3%) was unchanged (P = 0.37). The cord diameter was found to be decreased in 12 patients, and out of which, 11 (91.7%) improved on CCOS while cord diameter increased in 10 patients, but 8 (80%) improved (P = 0.57). The mean changes in syrinx diameter, cord diameter, and syrinx to cord ratio were not significant statistically when compared between improved and not improved group. Further, in this study, when these parameters were studied in both groups with and without duroplasty, were not significant statistically.
The consequence of the expansion of the cord from the inside out can lead to increase pressure in these cavities which in turn resulting in cord atrophy and clinical worsening. The poor outcome of patients despite resolution of syrinx can be explained by the fact that irreversible neurological damage secondary to progressive gliosis may persist after surgery.[27] We hypothesize that postoperative normalization of the craniospinal pressure dissociation creates a new equilibrium of CSF flow pattern enabling the hydrostatic pressure in syrinx to decrease. This leads to decrease devastating effects on surrounding cord tissue though the syrinx does not necessarily collapse.[16] This could explain why functional outcome does not correlate with change in any of the syrinx-related factors.
In Chiari patients, we hypothesize that perhaps the presence of syrinx rather than the size of syrinx makes a patient symptomatic. Syrinx is usually eccentric, and when it has affected crossing fibers, then clinical symptoms appear. Size of syrinx does not matter as it may decrease, remain status quo or increase in some patients. The surgery helps to reduce the pressure inside syrinx cavity, thereby on the cord.[28] Syrinx progression persists after craniocervical decompression because continued obstruction of the CSF pathways at the foramen magnum blocks the rapid efflux and influx of CSF between the cranial and spinal which normally compensates for brain expansion and contraction during the cardiac cycle. Other possibilities are inadequate decompression; progressive cord atrophy may be responsible for the increase in size of syrinx in some patients despite a reduction in syrinx pressure.
In this series, when the dura was opened, the surgical complications included one case of CSF leak; one case of subdural hygroma that subsequently resolved with conservative treatment only; and one case of superficial wound infection. When the dura was not opened, none of our patients had a complication. Hayhurst et al. reported overall 30% complication rate in the dural opening group compared with 12.5% in the bony decompression group.[29] In a retrospective study, Lee et al. noted CSF-related complications were more common in patients receiving PFDD (7/36) than posterior fossa decompression only (0/29) (P = 0.014).[6] The overall complication rate in our surgical cohort was 13.6%. We conclude that PFD without duraplasty might be associated with lesser complication rates with a similar outcome.
The current study focuses on long-term functional outcome, radiographic syrinx improvement, and influence of surgical techniques on syrinx and cord. We recommend neurosurgeons should focus on the functional outcome rather than radiological findings after surgical decompression and a residual syrinx can be followed over time if it does not increase and there are no changes in the clinical status. Our analysis suggests that performing duraplasty to treat CMI may lead to a greater decrease in concurrent syrinx; however, this could not be correlated with functional outcome. In other words, clinical results are comparable in both groups, whereas radiographic results are better for duraplasty group, although it is difficult to make this comment with patients that have severe obstruction secondary to CMI. These findings may help in surgical decision making and aid in patient education. The strengths of our study are prospective in nature; the CCOS provides a more robust comparison of functional outcome than earlier gestalt method and the sample size in this study is comparable to or larger than most earlier series. Although we have drawn several noteworthy correlations in this series, no definitive conclusions can be made as our conclusions are nevertheless limited by selection bias of treatment groups, data analysis is subject to treatment bias, and all potential confounding factors cannot be accounted for.
CONCLUSIONS
The functional outcome does not correlate with change in any of the syrinx-related factors. We found that surgical decompression with or without duroplasty has no statistically significant relationship with the degree of syrinx resolution. Surgical decompression without duroplasty provides the benefits of surgical decompression while avoiding the complications of intradural techniques. However, further studies with larger cohorts and longer follow-up would probably provide a better picture of the effect of these factors on outcome.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Chiari I malformation redefined: Clinical and radiographic findings for 364 symptomatic patients. Neurosurgery. 1999;44:1005-17.
- [Google Scholar]
- The case for duraplasty in adults undergoing posterior fossa decompression for chiari I malformation: A systematic review and meta-analysis of observational studies. Clin Neurol Neurosurg. 2014;125:58-64.
- [Google Scholar]
- Long-term follow-up of chiari-related syringomyelia in adults: Analysis of 157 surgically treated cases. Neurosurgery. 2009;64:308-15.
- [Google Scholar]
- Surgical treatment of chiari I malformation: Indications and approaches. Neurosurg Focus. 2001;11:E2.
- [Google Scholar]
- Surgery for syringomyelia: An analysis based on 163 surgical cases. Acta Neurochir (Wien). 2000;142:293-301.
- [Google Scholar]
- Comparison of posterior fossa decompression with or without duraplasty in children with type I chiari malformation. Childs Nerv Syst. 2014;30:1419-24.
- [Google Scholar]
- A novel scoring system for assessing chiari malformation type I treatment outcomes. Neurosurgery. 2012;70:656-64.
- [Google Scholar]
- Factors contributing improvement of syringomyelia and surgical outcome in type I chiari malformation. Childs Nerv Syst. 2009;25:453-9.
- [Google Scholar]
- External validation of the Chicago Chiari Outcome Scale. J Neurosurg Pediatr. 2014;13:679-84.
- [Google Scholar]
- Treatment of chiari I malformation in patients with and without syringomyelia: A consecutive series of 66 cases. Neurosurg Focus. 2001;11:E3.
- [Google Scholar]
- Clinical and radiological outcome of craniocervical osteo-dural decompression for chiari I-associated syringomyelia. Neurosurg Rev. 2010;33:297-303.
- [Google Scholar]
- Chiari I malformation with syringomyelia. Evaluation of surgical therapy by magnetic resonance imaging. J Neurosurg. 1988;68:726-30.
- [Google Scholar]
- International survey on the management of chiari I malformation and syringomyelia. Childs Nerv Syst. 2004;20:341-8.
- [Google Scholar]
- Syrinx size and duration of symptoms predict the pace of progressive myelopathy: Retrospective analysis of 103 unoperated cases with craniocervical junction malformations and syringomyelia. Clin Neurol Neurosurg. 2002;104:90-7.
- [Google Scholar]
- Expansion of chiari I-associated syringomyelia after posterior-fossa decompression. Childs Nerv Syst. 2000;16:555-8.
- [Google Scholar]
- Posterior fossa decompression in syringomyelia associated with a chiari malformation: A retrospective analysis of 22 patients. Clin Neurol Neurosurg. 2000;102:91-6.
- [Google Scholar]
- Outcome of chiari-associated syringomyelia after hindbrain decompression in children: Analysis of 49 consecutive cases. Neurosurgery. 2008;62:1307-13.
- [Google Scholar]
- “Conservative” cranio-cervical decompression in the treatment of syringomyelia-chiari I complex. A prospective study of 20 adult cases. Spine (Phila Pa 1976). 1995;20:2479-83.
- [Google Scholar]
- Pediatric syringomyelia with chiari malformation: Its clinical characteristics and surgical outcomes. Surg Neurol. 1999;51:383-90.
- [Google Scholar]
- The resolution of syringohydromyelia without hindbrain herniation after posterior fossa decompression. J Neurosurg. 1998;89:212-6.
- [Google Scholar]
- Effects of posterior fossa decompression with and without duraplasty on chiari malformation-associated hydromyelia. Neurosurgery. 2000;46:1384-9.
- [Google Scholar]
- Surgical experience in 130 pediatric patients with chiari I malformations. J Neurosurg. 2003;99:291-6.
- [Google Scholar]
- Correlation of functional outcome and natural history with clinicoradiological factors in surgically managed pediatric chiari I malformation. Neurosurgery. 2011;68:319-27.
- [Google Scholar]
- Comparison of posterior fossa decompression with and without duraplasty for the surgical treatment of chiari malformation type I in pediatric patients: A meta-analysis. J Neurosurg Pediatr. 2008;2:42-9.
- [Google Scholar]
- The role of cine flow MRI in children with chiari I malformation. Childs Nerv Syst. 2003;19:109-13.
- [Google Scholar]
- Intraoperative ultrasonography used to determine the extent of surgery necessary during posterior fossa decompression in children with chiari malformation type I. J Neurosurg. 2006;105:26-32.
- [Google Scholar]
- Quantitative cine-mode magnetic resonance imaging of chiari I malformations: An analysis of cerebrospinal fluid dynamics. Neurosurgery. 1994;35:214-23.
- [Google Scholar]
- Hindbrain decompression for chiari-syringomyelia complex: An outcome analysis comparing surgical techniques. Br J Neurosurg. 2008;22:86-91.
- [Google Scholar]






