Translate this page into:
Reposing the herniated spinal nerves following accidental iatrogenic dural tear in spine surgery-The “no touch hip flexion technique”
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
During lumbosacral operations dura may get breached and the cerebrospinal fluid (CSF) with underlying nerve roots immediately come out from the dura vent like a flower vase. These nerves don’t go back easily and also if attempted to push it in, cause physical damage. The treatment of dural tear has evolved through time. There are several methods for the repair of dural tear including primary repair, tissue sealant, blood patch, tissue grafting, gelfoam and glue applications.[1] We report five cases of accidental dural tear after lumbar disc Figure 1: Surgery, its intradural reposition with no-touch hip flexion technique [Table 1].

- L5/S1 PIVD
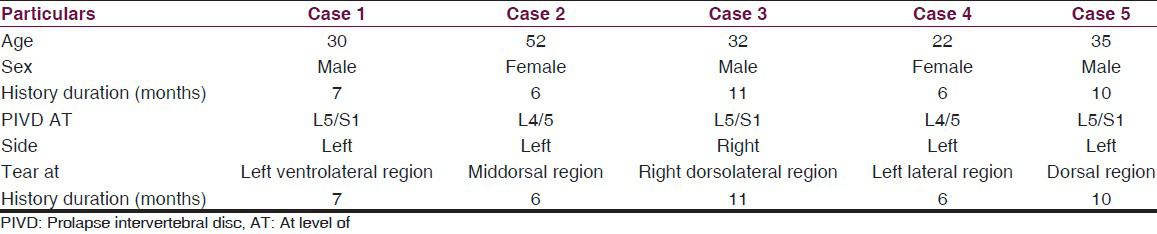
In all the cases during the operation, we noted that the ventral dura was severely adhered to the surrounding tissue. During dissection, the thinned dura was torn. There was CSF leakage and immediate rootlet herniation. We did not touch the herniated nerve roots, instead we put a cotton patty on the vent. Then semiprone position was made and back towards the operator. Then flexed the hip joint so that the intrathecal stretching of nerves transmitted through the lumbosacral nerves via sciatic nerve caused the herniated nerve roots to go inside spontaneously and immediately. Then water tight duraplasty was done without physical handling of herniated nerve roots. For confirmation of CSF leakage Valsalva maneuver was done before wound closure.
Incidental dural tear is a common complication of spinal surgery (incidence from 3.1% to 14%).[234] The risk of dural tears is increased by conditions such as fibrotic adhesion in chronic cases, scar tissue from prior surgery, eroded dura, redundant dura in patients with large disc herniations,[4] advanced patient age and the surgeon's training level.[5] Good long-term outcomes have been reported when incidental dural tears were recognized intraoperatively and repaired primarily.[3] There are several methods for the repair of dural tear including primary repair, tissue sealant, blood patch, and tissue grafting.[1] Poor clinical outcome[4] have been reported like posttraumatic spinal cord or nerve root herniation through a dural defect site which may cause recurrence of radiating pain also headaches and wound infection in the short term and presence of a pseudomeningocele, persistent CSF leak, neurologic deficits, fistula formation, meningitis, arachnoiditis, or an epidural abscess in the long term. In addition, a pseudomeningocele may entrap nerve roots or the spinal cord and cause radicular symptoms. Nerve root herniation is an infrequent complication of incidental dural tear. Unrecognized or incidental dural tear was repaired using Gelfoam and fibrin glue. Treatment with gelfoam and fibrin glue alone may not prevent persistent CSF leakage.[6] Surgically the dorsal dural vent is primarily repaired by increasing the vent and then manually reposing the herniated nerves with non-toothed fine forceps. Although conservative treatments such as bed rest and closed subarachnoid drainage have been attempted, midline durotomy and meticulous surgical dural repair remain the definitive treatment for ventral dural vents. One study reported that bed rest is not a definitive treatment; in this study, the patients who did not undergo dural repair developed complications.[7] These patients eventually underwent dural repair. Another study reported that the Valsalva maneuver may help identify the dural tear in suspected cases.[8] In dural dorsal or ventrolateral vents the physical handling of the herniated nerve roots thus iatrogenic damage may be avoided by a very simple maneuver. We operate these patients usually in prone position. Immediately after incidental dural tear we put a cotton patty on the herniated nerves. Do not touch the nerves with any instrument, make semi-prone position and flex the hip joint so that the various lumbosacral plexus’ nerves stretch which in turn stretches the intrathecal nerve root causes them to go inside without increasing the vent and physical handling of the nerves.
Iatrogenic dural vent causes rootlet herniation and a simple “no touch hip flexion technique” reposes the nerve roots effectively without physical handling to prevent nerve rootlet entrapment and other complications. Valsalva maneuver should be performed before and after the wound closure.
References
- Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: A review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976). 2006;31:2609-13.
- [Google Scholar]
- Spinal pseudomeningoceles and cerebrospinal fluid fistulas. Neurosurg Focus. 2003;15:E6.
- [Google Scholar]
- Evaluation and treatment of dural tears in lumbar spine surgery: A review. Clin Orthop Relat Res 200:238-47.
- [Google Scholar]
- Long-term results of lumbar spine surgery complicated by unintended incidental durotomy. Spine (Phila Pa 1976). 1989;14:443-6.
- [Google Scholar]
- Intervertebral space nerve root entrapment after lumbar disc surgery. Two cases. Spine (Phila Pa 1976) 1994:249-50.
- [Google Scholar]
- Treatment of dural tears associated with spinal surgery. J Bone Joint Surg Am. 1981;63:1132-6.
- [Google Scholar]
- Postlaminectomy lumbar pseudomeningocele: Report of four cases. Neurosurgery. 1992;30:111-4.
- [Google Scholar]





