Translate this page into:
Report of ventriculoperitoneal shunt for lately detected open-lip schizencephaly
*Corresponding author: Ajaya Kumar Ayyappan Unnithan, Department of Neurosurgery, Muthoot Hospital, Kozhencherry, Kerala, India. drajayakumara@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Unnithan AKA. Report of ventriculoperitoneal shunt for lately detected open-lip schizencephaly. J Neurosci Rural Pract. 2024;15:512-4. doi: 10.25259/JNRP_622_2023
Dear Editor,
Schizencephaly (“split brain”) is a neuronal migration disorder and causes seizures and developmental deficits.[1] The prevalence is reported as 1.54/100,000 births and 1/1650 patients with epileptic seizures or psychomotor retardation. There is a cleft through the cerebral hemisphere from the pia to the ependymal lining of the lateral ventricles. Type I or “closed-lip” schizencephaly has a strip of connecting gray matter tissue. In type II or “open-lip” schizencephaly, there is no connecting band. Children present with hemiparesis, seizures, intellectual disabilities, and language deficits.[2] Ventriculomegaly is common. Rarely, adults also present with symptoms due to schizencephaly.[3] Indications for surgery are features of raised intracranial tension (ICT) and intractable epilepsy.[1,4] Ventriculoperitoneal (VP) shunt is done to reduce intracranial pressure, although it is not a treatment for schizencephaly[5,6]
A 41-year-old male presented with headache, neck pain, left-side weakness, and recurrent seizures. Headache and neck pain were present for about one month. He had seizures since childhood and was on clobazam and oxcarbazepine. He had seizures from the age of six and was not on regular medicines. Later, he was given clobazam from the age of 20 years, and oxcarbazepine was added for control. He consulted a neurologist one month ago. Levetiracetam also was added. He has left hemiparesis and decreased cognition since childhood. He is oriented and has good attention. He has dyscalculia, impaired abstract thinking, and constructional apraxia. Left forearm and hand had atrophy and deformity. The whole muscles of the forearm and hand were atrophic and had flexion deformity at the elbow. He had a paretic gait. There was no neck stiffness. There was prominence on the right side of the head. He did not have any psychiatric manifestations.
Computed tomography (CT) brain showed a large subdural collection along the right frontotemporoparietal region, communicating with the right lateral ventricle, suggestive of open-lip schizencephaly. Associated corpus callosal dysgenesis and enlargement of right hemicranium are seen [Figure 1a]. Although magnetic resonance imaging is needed to evaluate congenital malformations, 128-slice CT with reformations showed the details.
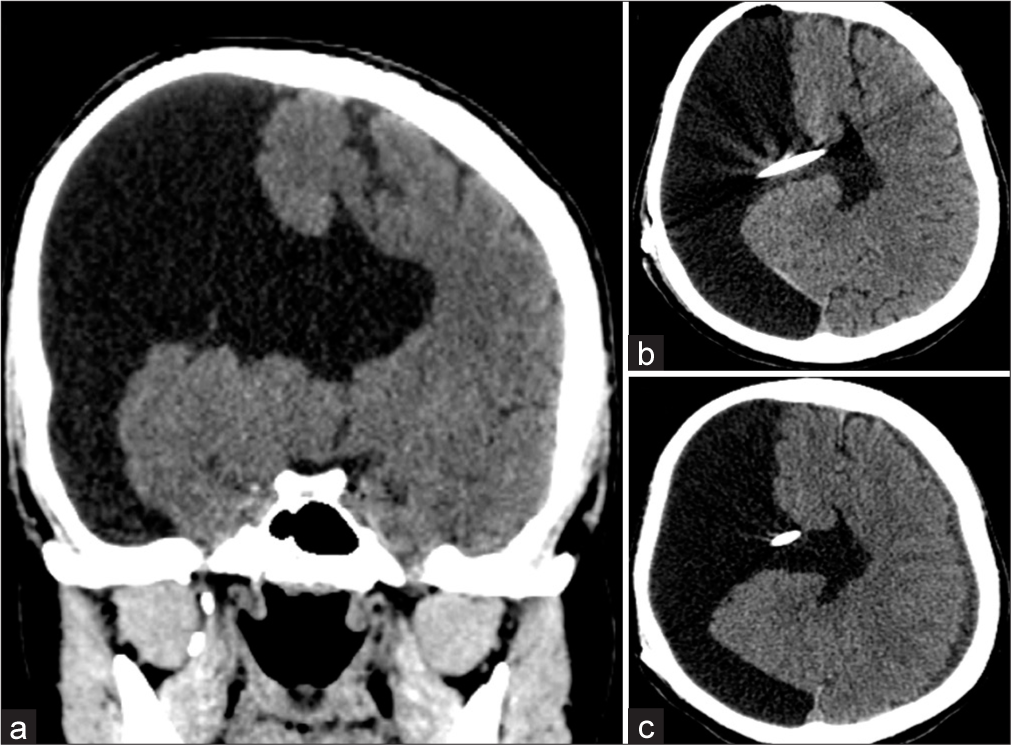
- (a) Computed tomography (CT) scan showing large subdural collection on the right side with open-lip schizencephaly; (b) post-operative CT scan showing the tip of shunt in ventricle; and (c) follow-up CT scan showing a reduction in right subdural collection and appearance of thin subdural hygroma on the left side.
The right VP shunt was done. The indications were symptoms of raised intracranial tension and large subdural collection in CT. Burr hole was made over parietal eminence. Chhabra low-pressure shunt was used. The ventricular catheter was inserted into the cavity and clear fluid came under pressure. Post-operative CT scan showed a reduction in the subdural collection [Figure 1b].
Headache and neck pain reduced. He had a subjective reduction in the enlargement of the right hemicranium. The CT brain after one month showed a thin subdural hygroma on the left side, suggestive of a reduction in the intracranial pressure [Figure 1c]. Paretic gait improved. No seizure occurred in three years. The electroencephalogram was normal. Levetiracetam was stopped and the dose of clobazam was reduced.
The VP shunt or cysto-VP shunt is recommended for large fluid-filled cavities associated with open-lip schizencephaly.[1] Literature shows a good prognosis after surgery in children. The VP shunt was successful for a tonsillar herniation in a preterm infant with open-lip schizencephaly and progressive hydrocephalus.[6] Clinical improvement has been noted in the case of bilateral fluid-filled cavities following the VP shunt.[7] Malignant hyperthermia and cerebral venous thrombosis occurred after VP shunt in a 9-month-old boy with schizencephaly and progressive hydrocephalus.[8] He was treated with dantrolene and hydration. A female neonate had hydrocephalus, large open-lip left schizencephaly, patent foramen ovale, spondylocostal dysplasia, and hypoparathyroidism. The VP shunt was done. However, she died due to bronchopneumonia and respiratory failure.[9]
Refractory epilepsy following VP shunt for hydrocephalus in a child with schizencephaly necessitated anatomic hemispherectomy.[10] At present, there is no report of VP shunt for an adult with schizencephaly. The published cases of schizencephaly who underwent shunt surgery are shown in Table 1.
| Author | Number of cases | Age/sex | Clinical features | Imaging | Surgery | Follow-up |
|---|---|---|---|---|---|---|
| Chiang et al. | 1 | 7-months/F | Right hemiparesis, head nodding | Left schizencephaly with mass effect. | VP shunt | Improvement in head nodding and hemiparesis |
| Halabuda et al. | 3 | 1) 33-year/M 2) 1-month /F 3) 1-month /F |
1) Seizure, headache, vomiting. 2) Epilepsy, intracranial hypertension. 3) Epilepsy, intracranial hypertension |
1) Bilateral fluid-filled spaces in middle cranial fossae. 2) Bilateral temporal and occipital fluid-filled spaces. 3) Bilateral open schizencephaly. |
1) Cysto-peritoneal shunt 2) VP shunt 3) Cysto-VP shunt |
1) Small intracerebral and subdural hematomas. Fluid-filled spaces reduced. 2) Marked reduction of fluid-filled spaces. 3) Clinical improvement, but has epilepsy. |
| Gonzalez et al. | 1 | 4-day/M | Rapid head growth, tense anterior fontanelle, sutural diastasis. | Right occipitoparietal open-lip schizencephaly. | VP shunt | Recovered |
| Rege and Patil | 1 | 15-day/F | Poor feeding, seizure, large head, tense fontanelle. | Bilateral frontoparietal fluid-filled spaces. | VP shunt | Clinical improvement. |
| Watanabe et al. | 1 | 9-month/M | Congenital cataract, progressive hydrocephalus. | Schizencephaly. | VP shunt | Malignant hyperthermia and cerebral venous thrombosis, improved. |
| Ognean et al. | 1 | Neonate | Hypotonia, weak sucking, patent foramen ovale, spondylocostal dysplasia, and hypoparathyroidism. | Hydrocephalus, large open-lip left schizencephaly. | VP shunt | Pneumonia, respiratory failure, died in 5th month. |
| Heuer et al. |
1 | 1-year/M | Large head. | Hydrocephalus with large cleft. | VP shunt | Refractory epilepsy. Anatomic hemispherectomy was done at 8-year. |
VP: Ventriculo-peritoneal
The treatment for schizencephaly focuses mainly on rehabilitation for deficits.[3,7] Surgical resection of the epileptogenic zone, topectomy, and temporal lobectomy are the surgical procedures that may be needed in case of intractable epilepsy.[4] Large fluid-filled spaces, hydrocephalus, and intracranial hypertension necessitate shunt surgery.[1]
This is a report of an adult with lately detected open-lip schizencephaly producing a large fluid collection and mass effect. This is the first report of VP shunt for an adult with schizencephaly. Although the patient already had symptoms during childhood, the diagnosis was delayed. This may be an alerting case report, especially with regard to the diagnostic services in rural areas. The high index of suspicion in a child with seizure and focal deficit should lead to prompt imaging to diagnose congenital malformations.
Ethical approval
The Institutional Review Board has waived the ethical approval for this study.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Schizencephaly-diagnostics and clinical dilemmas. Childs Nerv Syst. 2015;31:551-6.
- [CrossRef] [PubMed] [Google Scholar]
- Schizencephaly in children: A single medical center retrospective study. Pediatr Neonatol. 2018;59:573-80.
- [CrossRef] [PubMed] [Google Scholar]
- A rare case of schizencephaly in an adult with late presentation. J Family Med Prim Care. 2017;6:450-2.
- [CrossRef] [PubMed] [Google Scholar]
- Long-term outcome of surgical treatment of patients with intractable epilepsy associated with schizencephaly. Acta Neurochir (Wien). 2013;155:1717-24.
- [CrossRef] [PubMed] [Google Scholar]
- Ventriculo-peritoneal shunt in the treatment of schizencephaly with infantile spasm: Report of one case. Zhonghua Min Guo Xiao Er Ke Yi Xue Hui Za Zhi. 1991;32:257-61.
- [Google Scholar]
- Unilateral open-lip schizencephaly with tonsillar herniation in a preterm infant. J Pediatr Neurosci. 2019;14:225-7.
- [CrossRef] [PubMed] [Google Scholar]
- Bilateral giant open-lip schizencephaly: A rare case report. J Pediatr Neurosci. 2016;11:128-30.
- [CrossRef] [PubMed] [Google Scholar]
- Malignant hyperthermia and cerebral venous sinus thrombosis after ventriculoperitoneal shunt in infant with schizencephaly and COL4A1 mutation. World Neurosurg. 2019;127:446-50.
- [CrossRef] [PubMed] [Google Scholar]
- Hydrocephaly, schizencephaly, spondylocostal dysplasia, and hypoparathyroidism in an infant of a diabetic mother. Acta Endocrinol (Buchar). 2017;13:494-501.
- [CrossRef] [PubMed] [Google Scholar]
- Anatomic hemispherectomy for intractable epilepsy in a patient with unilateral schizencephaly. J Neurosurg Pediatr. 2008;2:146-9.
- [CrossRef] [PubMed] [Google Scholar]





