Translate this page into:
Prevalence of anxiety and depressive symptoms during COVID-19 pandemic among the general population in India: A systematic review and meta-analysis
*Corresponding author: Jaison Joseph, Department of Psychiatric Nursing, College of Nursing, Pt. B.D. Sharma University of Health Sciences, Rohtak, Haryana, India.jaisonjsph@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Sharma SK, Joseph J, Varkey BP, Dhandapani M, Varghese A, Sharma S, et al. Prevalence of anxiety and depressive symptoms during COVID-19 pandemic among the general population in India: A systematic review and meta-analysis. J Neurosci Rural Pract 2022;13:608-17.
Abstract
Objective:
The novel coronavirus (n COVID-19) has affected every walk of life across the world including India. Several studies have been available on the COVID-19-related anxiety and depressive symptoms in the public health context. However, there is a dearth of evidence of a meta-analysis regarding the pooled estimates of anxiety and depressive symptoms related to this pandemic based on the existing studies conducted among the general population of India. The aim of the study was to estimate the pooled prevalence of COVID-19-related anxiety and depressive symptoms among the general population in India.
Material and Methods:
We searched the following electronic bibliographic databases: PubMed, Ovid, Science Direct, and Wiley online library for studies conducted from the onset of the COVID-19 pandemic and until September 25, 2021. We separately analyzed the outcome measures based on the risk of bias assessment. The publication bias was evaluated by funnel plots and Egger’s test.
Results:
We used a random-effect model due to the significant heterogeneity between the studies (Anxiety symptoms – I2 = 99.40% and Depressive symptoms – I2 = 95.3%). According to the index meta-analysis, the pooled estimates of anxiety and depressive symptoms among general population of India during COVID-19 pandemic are 23.5% (95% CI: 17.4–29.6%; n = 21 studies) and 20.2% (95% CI: 17.2–23.2%; n = 17 studies), respectively. In subgroup analyses, good-quality studies (Score ≥7/9) had a significant effect on the pooled prevalence.
Conclusion:
About one-fifth of the general population of India reported having anxiety and depressive symptoms during the COVID-19 pandemic. The pooled estimates varied with the methodological quality of included studies. The present study provides a comprehensive picture of the overall magnitude of anxiety and depressive symptoms due to the COVID-19 outbreak which will guide the policy makers to measure the burden of similar pandemics more judiciously in the future.
Keywords
COVID-19
Pandemic
Anxiety
Depression
General population
India
PROSPERO REGISTRATION: CRD42021282389
INTRODUCTION
A group of pneumonia cases of blurred causation connected to the South China Seafood Market alerted the health authorities in Wuhan, China at the end of 2019. Subsequently, laboratory tests found a novel coronavirus, SARS-CoV-2 as a cause for this rapid surge in pneumonia cases.[1] Coronavirus disease 2019 (COVID-19) pandemic has affected every walk of life across the world. The COVID-19, first detected in India in January 2020, started to spread in the 2nd week of March 2020.[2] One of the main approaches adopted by many countries was to impose cross-country lockdowns to prevent the spread of COVID-19 infections. Although these lockdowns were able to reduce the risk of morbidity and mortality related to COVID-19, they caused varying levels of psychological trauma and affected the mental health of the population.[3] The consequences on the mental health of the people were reported among several population groups during the COVID-19 outbreak. Underlying anxiety and depressive symptoms about this new disease can affect anyone in a society that hatches fear among people.[4] Recent pieces of evidence reported the psychological impact of COVID-19 through anxiety, depression, insomnia, post-traumatic stress disorders, attention deficit hyperactive disorders, anger, and fear of getting infected with COVID-19 among the general population.[5] Consequently, the unending psychological impacts across all the socioeconomic domains from rapidly expanding panic related to COVID-19 could have potentially caused even more damage than physical symptoms.[6] Because of numerous psychological problems related to COVID-19, there is dearth of pooled data regarding the mental health statistics among the Indian population. Recently, quite a several research reports on anxiety and depressive symptoms about COVID-19 were published. However, there is a lacuna of evidence of a meta-analysis regarding the pooled estimates of anxiety and depressive symptoms related to this pandemic based on the existing studies conducted among the general population of India. This study systematically reviewed all the published online surveys and estimated the aggregate evidence regarding the anxiety and depressive symptoms expressed by the general public during COVID-19 pandemic in this setting.
MATERIALS AND METHODS
This systematic review is reported following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guideline checklist[7] and is registered in the PROSPERO (CRD42021282389).
Search strategy
Multiple electronic databases such as PubMed, Wiley online library, Science Direct, APA Psych Info, and grey literature sources were searched for articles published from January 2020 to September 2021, to retrieve potential articles on anxiety and depressive symptoms due to COVID-19 among the general population in India. We used the following search terms; “prevalence,” “depression,” “anxiety,” “COVID-19,” “India” combined with the use of Boolean operators “AND” and “OR.” Both free-text words and MeSH terms were used for the search process [Supplementary Material 1]. The studies were independently reviewed by two reviewers (JJ and AV) for eligibility and eligible studies were selected after removing the duplicates manually.
Eligibility criteria
Our inclusion criteria were studies conducted in India, studies reporting anxiety or depressive symptoms, the population included the general population. Our exclusion criteria were studies conducted among health-care personnel, reviews, case reports, and qualitative studies. Further, studies with inadequate data and outcome measures other than anxiety and depressive symptoms such as psychological distress, post-traumatic stress disorders, and physical symptoms were also excluded from the study. No attempts are made to acquire grey/unpublished literature considering the inherent conflict of interest which might increase the risk of bias.
Data extraction, quality assessment, and data synthesis
The data from the studies were extracted onto a data extraction form with the following study characteristics and relevant data, namely, author (year and period of conducting the study), study design, sample size, age, and survey tools. The main outcomes assessed were the prevalence of anxiety and depressive symptoms. The methodological quality of included studies was assessed by two independent reviewers employing the “JBI Critical Appraisal Checklist for Studies Reporting Prevalence Data.”[8] This checklist contains nine criteria with a total quality score ranging from 1 to 9. We classified scores as having a high (0–3), moderate (4–6), and low (7–9) risk of bias. Two independent reviewers (MD and JJ) assessed the methodological quality of the studies using the Joanna Briggs quality assessment tool. Discrepancies were addressed by discussion and mutual consensus and involved a senior third reviewer (SS).
In all statistical analyses, the significance level was considered at P < 0.05, employing the software open Meta. Statistical heterogeneity was measured using I2 statistics. Heterogeneity was considered not important (0–40%), moderate (30–60%), substantial (50–90%), and considerable (75–100%).[9] Freeman-Tukey Double Arcsine Proportion metric was applied to calculate the pooled prevalence as it is one of the best methods to fix the variance between studies. The pooled estimate of prevalence was calculated using the DerSimonian and Laird method of random effects models and reported as a proportion with a 95% confidence interval.[10] The funnel plot and Egger’s regression tests were used to assess potential publication.
RESULTS
The search across different electronic databases yielded 2984 citations. Duplicate studies were removed and 1384 studies were further screened. A total of 22 full-text studies (Studies evaluated anxiety symptoms – 21; and Studies evaluated depressive symptoms – 17) meeting inclusion and exclusion criteria were included in the final analysis [Figure 1]. The basic characteristics of the included studies are shown in [Table 1].[11-32] The studies were conducted from March 2020 to February 2021 across various regions of India. All the studies were cross-sectional and conducted among the general population through online web-based surveys.

- Process of search and selection of studies.
| Author/ Period of study |
Study setting and design | Male/Female | Age in years (Mean±SD)/Range |
Sample size/ Sampling method |
Survey tools | Depression % (n/N) |
Anxiety % (n/N) |
|---|---|---|---|---|---|---|---|
| Pandey et al.[11] March 24–April 11, 2020 |
Across India/ Online survey |
582/805 | 25.0±10.2 | 1387/ Snow ball |
DASS-21 | 16.6% (232/1387) |
14.3% (199/1387) |
| Bhowmick et al.[12] April 18–May 3, 2020 |
West Bengal/ Online survey |
182/171/2 others | 18-80 | 355/ Snow ball |
GAD-7 | NM | 15.49% (55/355) |
| Gopal et al.[13] March 29–May 24, 2020 |
Across India/ Online survey |
103/56 | 27.44±9.17 | 159/ Snow ball |
GAD-7 PHQ-4 |
14.8% (23/159) |
29.2% (62/159) |
| Joseph et al.[14] 17th April–1th May 2020 |
Haryana/ Online survey |
366/374 | 58.68±8.05 | 740/ Snow ball |
PHQ-9 GAD-7 |
8.8% (65/740) |
6.1% (45/740) |
| Verma et al.[15] April 4–14, 2020 |
Across India/ Online survey |
183/173 | 18–41 | 345/ Snow ball |
DASS-21 | 25% (86/345) |
28% (97/345) |
| Kaurani et al.[16] April 19–May 5, 2020 |
Across India/ Online survey |
310/317 | 20–70 | 627/ Snow ball |
BAI-21 | NM | 23/627 36.68% |
| Chaudhary et al.[17] November 15, 2020–February 15, 2021 |
Karnataka/ Online Survey |
180/144 | 18–30 | 324/ Snow ball |
GAD-7 PHQ-9 |
28.7% (93/324) |
23.76% 77/324 |
| Kaur et al.[18] May 24–June 5, 2021 |
Across India/ Online survey |
525/584 | 32.98±14.72 | 1109/ Snow ball |
DASS-21 | 25.87% 287/1109 |
45.26% 506/1109 |
| Singh and Khokhar[19] Last week of April 2020 |
West Bengal/ Online survey |
95/139 | 28.59±10.47 | 234/ Snow ball |
PHQ-9 | 14.1% 33/234 |
NM |
| Srivastava et al.[20] June 20–July 4, 2020 |
Across India/ Online survey |
1146/858 | 37 (18–60) | 2004/ Snow ball |
CAS | NM | 3.29% 66/2004 |
| Wakode et al.[21] May 18–25, 2020 |
Across India/ Online survey |
149/108 | 25 | 257/ Snow ball |
GAD-7 | NM | 88% 228/257 |
| Nathiya et al.[22] May 23–29, 2020 |
Across India/ Online survey |
278/201 | 15–30 | 479/ Snow ball |
DASS-21 | 24.63% 118/479 |
30.89% 148/479 |
| Hazarika et al.[23] April 6–22, 2020 |
Across India/ Online survey |
167/255 | 30.5±10.9 | 422/ Snow ball |
DASS-21 | 34.7% (146/422) |
32% (135/422) |
| Gaur et al.[24] April 24–May 7, 2020 |
Across India/ Online survey |
653/362 | 18–60 | 1015/ Snow ball |
GAD-7 PHQ-9 |
12.8% 129/1015 |
9% 92/1015 |
| Chauhan et al.[25] April 1–30, 2020 |
Across India/ Online survey |
614/373 | 34.28±12.27 | 987/ Snow ball |
SAS | NM | 32.2% (318/987) |
| Balhara YPS. et al.[26] April 2020-Journal Submission |
New Delhi/ Online survey |
NM | 19.6±1.9 | 128/ Snow ball |
PHQ-9 GAD-7 |
26.9% 105/393 |
16.92% 66/393 |
| Sebastian et al.[27] Not Available |
29 States of India/ Online survey |
NM | 29.3±9.7 | 1257/ Snow ball |
PHO-4 | 13.9% (174/1257) |
13.9% (174/1257) |
| Grover et al.[28] April 6–24, 2020 |
Across India/ Online survey |
NM | 41.2±13.6 | 894/ Snow-ball |
GAD-7 PHQ-9 |
105/894 11.74 |
140/894 15.65% |
| Tomar et al.[29] April 28–May 8,2020 |
Across India/ Online survey |
1160/1085 | 32.4±11.4 | 2245/ Snow ball |
DASS-21 | 20.66% (464/2245) |
23.47% (534/2245) |
| Wani et al.[30] May 2020 |
Kashmir/Online study | 138/149 | 27.35±7.81 | 287/ Snow ball |
DASS-21 | 29.61% (85/287) |
25.08% (72/287) |
| Reddy et al.[31] April 1–May 12, 2020 |
11 States of India/ Online survey |
477/416 | 16-60 | 891/ Respondent -driven |
DASS 21 | 22% 200/891 |
15% 138/891 |
| Desai et al.[32] April 8–14, 2020 |
Karnataka/ Online survey |
764/768/5 others | 10-70 | 1537/ Snow ball |
GAD-7 PHQ-9 |
16.7% (257/1537) |
12.4% (192/1537) |
NM: Not mentioned, Depression, Anxiety, and Stress Scale-21 (Cutoff: -Depression ≥ 13, Anxiety ≥ 09, Stress ≥ 19), GAD-7-generalized anxiety disorder (Cutoff ≥ 10), PHQ-4-Patient health questionnaire (Cutoff ≥ 3), PHQ-9: Patient health questionnaire (Cutoff ≥ 10), BAI: Beck Anxiety Inventory (Cutoff ≥ 22), CAS: Coronavirus anxiety scale (Cutoff ≥ 9), SAS: Zung Self-Rating Anxiety Scale (Cutoff ≥ 45)
The total sample size was 17,683 ranging from 128 to 2245. The majority of the participants (52.4%) were males and details of the gender distribution of the study participants were not available in the three studies.[26-28] Twelve studies[11,13,14,18,19,23,25-30] specifically mentioned the details of the age of the study participants in which the mean age was 32.27 (SD-10.01).
The age range of the subjects varied from 10 to 80 years in which four studies enrolled participants <18 years of age,[11,22,31,32] and one study exclusively targeted the anxiety and depressive symptoms among the middle-aged and elderly population.[14] Out of the –22 studies, 15 studies[11,13,15,16,18,20-25,27-29,31] recruited study subjects from various states of India. The remaining seven studies had participants from Karnataka (n = 2),[17,32] West Bengal (n = 2),[12,19] Haryana (n = 1)14, New Delhi (n = 1),[26] and Jammu and Kashmir (n = 1).[30] Various validated scales with specific cutoffs used in our study were: Depression, Anxiety, and Stress Scale-21 (DASS-21), Generalized Anxiety Disorder (GAD7), Patient health questionnaire (PHQ) (PHQ-4 and PHQ-9), Beck Anxiety Inventory, Coronavirus Anxiety Scale, and Zung Self-Rating Anxiety Scale.
The prevalence estimates
The pooled estimates of anxiety and depressive symptoms among general population of India during COVID-19 pandemic were 23.5% (95% CI: 17.4–29.6%; n = 21 studies) and 20.2% (95% CI: 17.2–23.2%; n = 17 studies), respectively [Figures 2 and 3]. We used the DerSimonian and Laird method of random-effects models to calculate the pooled estimates as there was a significant heterogeneity on the outcome measures (Anxiety symptoms – I2 = 99.40%, Q = 3365.79, P < 0.001, Tau Squared = 0.02 and Depressive symptoms – I2 = 95.3%, Q = 340.30, P < 0.001, Tau Squared = 0.04).

- Prevalence of anxiety symptoms among general population of India during COVID-19 pandemic.

- Prevalence of depressive symptoms among general population of India during COVID-19 pandemic.
Methodological quality
Out of the 22 studies (21 studies evaluated anxiety symptoms and 17 studies evaluated depressive symptoms), the median quality score was 6 (Mean – 5.45; SD – 1.5) and the quality score ranged from 3 to 7. Among studies on anxiety symptoms, there were eight high-quality studies (Score ≥ 7/9), and the remaining 13 studies were found to have a moderate-to-high risk of bias. Among the 17 studies on depressive symptoms, there were eight high-quality studies (Score ≥ 7/9) and nine were of moderate-to-low quality. Altogether, the reporting structure was poorly followed in the majority of the studies making the comparisons an arduous task. The sample size calculation and the characteristics pertinent to standards of data collection were not addressed in many studies. [Table 2] summarizes the quality score of each study included in the meta-analysis.
| Author | Q1 | Q2 | Q3 | Q4 | Q5 | Q6 | Q7 | Q8 | Q9 | Score | Remarks |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pandey et al. | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 5 | Moderate risk of bias |
| Bhowmick et al. | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 4 | Moderate risk of bias |
| Gopal et al. | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 5 | Moderate risk of bias |
| Joseph et al. | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 1 | 1 | 7 | Low risk of bias |
| Verma et al. | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 7 | Low risk of bias |
| Kaurani et al. | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 4 | Moderate risk of bias |
| Chaudhary et al. | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 7 | Low risk of bias |
| Kaur et al. | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 1 | 7 | Low risk of bias |
| Singh et al. | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 0 | 3 | High risk of bias |
| Srivastava et al. | 1 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 5 | Moderate risk of bias |
| Wakode et al. | 0 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 4 | Moderate risk of bias |
| Nathiya et al. | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low risk of bias |
| Hazarika et al. | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low risk of bias |
| Gaur et al. | 1 | 1 | 0 | 1 | 1 | 1 | 0 | 1 | 0 | 6 | Moderate risk of bias |
| Chauhan et al. | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 3 | High risk of bias |
| Balhara et al. | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 1 | 0 | 4 | Moderate risk of bias |
| Sebastian et al. | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 | Moderate risk of bias |
| Grover et al. | 1 | 1 | 0 | 0 | 1 | 1 | 1 | 0 | 1 | 6 | Moderate risk of bias |
| Tomar et al. | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 | Moderate risk of bias |
| Wani et al. | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 1 | 0 | 3 | High risk of bias |
| Reddy et al. | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low risk of bias |
| Desai et al. | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 1 | 0 | 7 | Low risk of bias |
Q1 -Was the sample frame appropriate to address the target population?; Q2 -Was study participants sampled in an appropriate way?; Q3 -Was the sample size adequate?; Q4 -Was the study subjects and the setting described in detail?; Q5 -Was the data analysis conducted with sufficient coverage of the identified sample?; Q6 -Was valid methods used for the identification of the condition?; Q7 -Was the condition measured in a standard, reliable way for all participants?; Q8 -Was there appropriate statistical analysis?; Q9 -Was the response rate adequate, and if not, was the low response rate managed appropriately? (1 – Yes; 0 – No)
Subgroup and sensitivity analysis
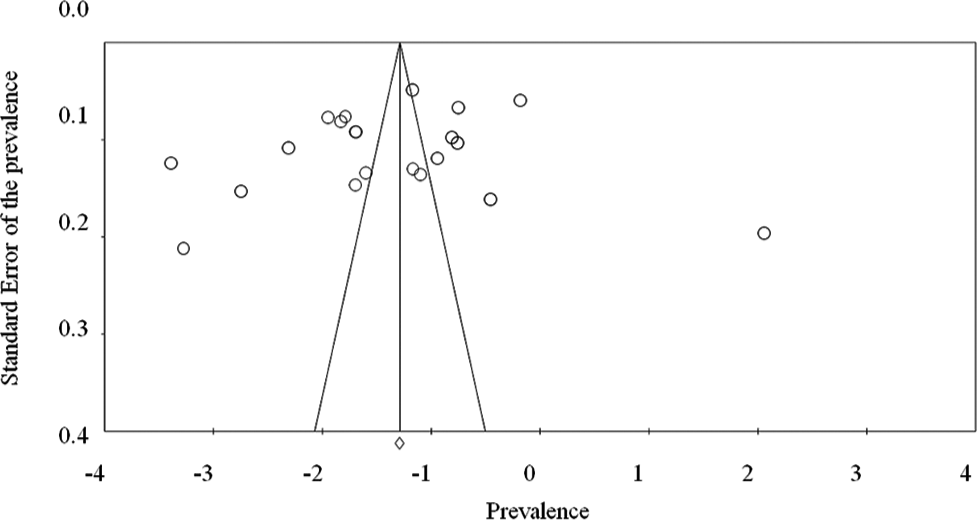
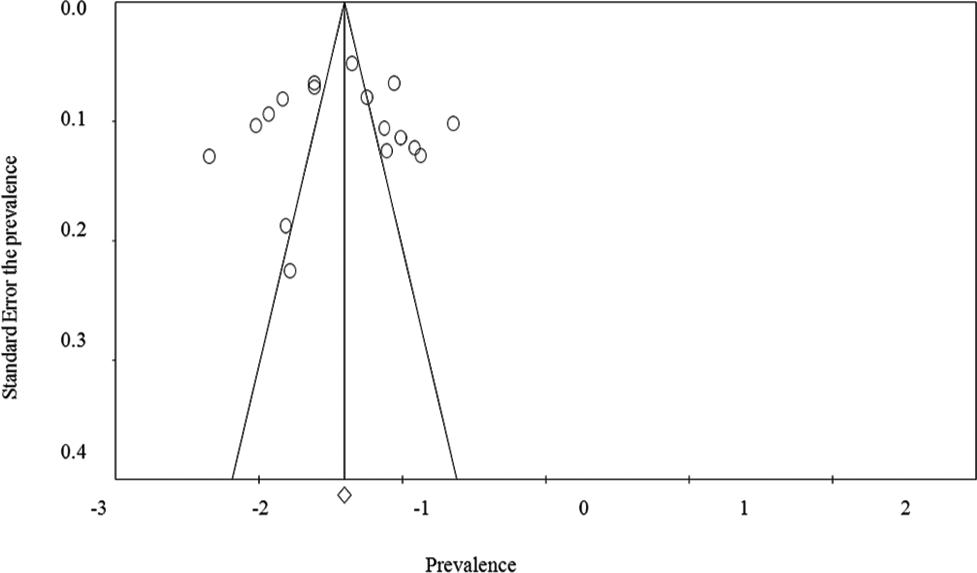
We did subgroup analyses based on the methodological quality of included studies [Table 3]. The pooled estimates of anxiety symptoms were slightly higher for good-quality studies (Score ≥ 7/9) than those with moderate and low quality (24.2%; 95% CI: 14.8–33.7% vs. 23.0%; 95% CI: 14.9– 31.1%). The pooled prevalence of depressive symptoms was higher for those with good-quality studies (Score ≥ 7/9) as compared to those studies with moderate and low quality (23.2%; 95% CI: 17.5–28.9% vs. 17.5%; 95% CI: 14.3–20.7%). We did a leave-one-out sensitivity analysis using the random effect model to identify the effect of individual studies in which the prevalence of anxiety and depressive symptoms ranged between 20.1–24.5% and 19.3–20.9%, respectively. A reasonable asymmetry of the funnel plot [Supplementary Materials 2 and 3] revealed the existence of publication bias and Egger’s test of the outcome measures revealed no publication bias (Anxiety symptoms: P = 0.349 and Depressive symptoms: P = 0.897).
| Subgroup | Category | No. of studies | Events/N | Pooled prevalence (95% CI) |
Heterogeneity | χ2 (P-value) | |
|---|---|---|---|---|---|---|---|
| I2 | T | ||||||
| Methodological Quality (Score ≥ 7/9) | |||||||
| Depression | Moderate and High Risk Low Risk |
09 08 |
1350/7871 1252/5847 |
17.5% (14.3–20.7%) 23.2% (17.5–28.9%) |
92.72 96.67 |
0.022 0.066 |
26.64<0.0001 |
| Anxiety | Moderate and High Risk Low Risk |
13 08 |
2029/11867 1338/5847 |
23.0% (14.9–31.1%) 24.2% (14.8–33.7%) |
99.53 98.95 |
0.022 0.018 |
56.75<0.0001 |
DISCUSSION
The present study provides a statistical summary of online surveys related to COVID-19 associated anxiety and depressive symptoms in the Indian general public. This meta-analysis reports that in India, the aggregate prevalence of depression and anxiety symptoms among the general population ranged from 20.2% to 23.5%, though estimates varied based on screening tools and methodological approaches. Psychological reactions may vary according to the impact of the pandemic and the time of data collection, hence, should be interpreted accordingly. There is a wide variation in the magnitude of psychological impact due to COVID-19 across the globe.[33] Two recently published meta-analyses estimated the pooled prevalence of COVID-19-related anxiety symptoms (31.9–38.12%) and depressive symptoms (33.7–34.1%) in the general population across the global community, which was notably higher than our findings.[34,35] Furthermore, a web-based survey from China reported an overall prevalence of anxiety and depressive symptoms of 35.1% and 25.1%, respectively, during the peak period of the COVID-19 epidemic.[36] These discrepancies in the results may be explained by significant heterogeneity based on the country-wide differences in onset and severity of the pandemic, availability, and utilization of healthcare, awareness of COVID-19, and guidelines for the general public. Our findings are based on the online surveys conducted from the inception of COVID-19 to September 2021. The first and second waves of COVID-19 in India started in the middle of March 2020 and 2021, respectively.[37]
As expected, there was significant heterogeneity between the studies (Anxiety symptoms – I2 = 99.40% and Depressive symptoms – I2 = 95.3%) included in our meta-analyses. This might be attributed to the differences in the screening tools and methodological approaches employed in each study. However, it is worth noting that our pooled estimates are based on the existing studies with uniform cutoff scores as per the standard screening tools. Taken together, we also noted that the exclusion of a single study did not affect the overall pooled prevalence in which the prevalence of anxiety and depressive symptoms ranged between 20.1–24.5% and 19.3–20.9%, respectively. The National Mental Health Survey of India 2015–16 (NMHS-2015-2016) found that the mental morbidity of individuals above the age of 18 years was 10.6% in the lifetime prevalence of depression and was reported to be 5.2%.[38] As expected, the findings of the present study reported a high rate of pandemic-related depression in the general public as compared to the NMHS-2015-2016 data. However, our findings need to be interpreted based on several grounds of uncertainties that might confound the general public views related to the COVID-19 worldwide epidemic. The inherent design of the included studies like sampling techniques and the online surveys circulated through a few social media platforms such as WhatsApp which limit the generalizability of the study to people with internet access. The sample might be contaminated by selection and respondent bias and the likelihood of under or over-reporting is also need to be considered.
Implications
Certainly, the findings of this study might be the stepping-stones to devising appropriate planning to protect the general public during the current or emerging pandemic situation. An aggregate of estimates of anxiety and depressive symptoms across the country has implications for planning specialized mental health initiatives such as toll-free helplines, e sanjeevani helplines, and telepsychological consultation.[39] As the COVID-19 pandemic made greater demand on the mental health-care resources, the government policy should address the specialized services in times of pandemics. The present study further advocates the importance of sensitizing the public to stay away from overloaded information during every pandemic. Uncertainty and insecurity about the future result in depressive and anxiety symptoms. Therefore, the public mass campaigns should focus more on general coping strategies and positive well-being to address the psychological morbidities. Having said that, the effective utilization and reach of these services might not be possible without sound epidemiological data. With the history of worldwide epidemics repeating, the wide dissemination of psychological first aid services needs strategic plans in the form of virtual clinics and ongoing online surveillance systems.[40] All these efforts are vital for the successful monitoring and management of the future pandemic. Taken together, the current estimates will guide the researchers and policymakers to minimize the psychological impact caused by a similar pandemic in the future by focusing more on the public campaigns to build protective factors against anxiety and depressive symptoms.
Strength and limitations
The major strength of the present meta-analysis is its novelty of unique comprehensive data regarding the overall psychological burden of COVID-19 among the general population of India. Besides, to the best of our knowledge, this is the first meta-analysis that provides an epidemiological evidence base regarding the magnitude of anxiety and depressive symptoms linked to COVID-19 in the general population of India. The separate analysis based on methodological quality is a further strength in terms of the credibility of the findings. However, there are certain drawbacks to this paper. The results are purely based on online surveys recruited through snowball sampling using different web-based platforms posing a threat to the external validity of findings due to selection and respondent bias. In addition, confounding risk factors that may influence the findings of the study such as the presence of a history of mental illness and substance use were not reported in many of the studies. Several studies included in the meta-analysis were found to have moderate-to-high risk of bias leading to limitations in the quality of strength of evidence. Although the included studies used valid scales for measuring anxiety and depressive symptoms, high heterogeneity was observed due to differences in sensitivity and specificity of screening tools. Therefore, the data on the severity and type of anxiety disorder and depression have not been considered.
CONCLUSION
About one-fifth of the general population of India reported having anxiety and depressive symptoms during the COVID-19 pandemic. The pooled estimates varied with methodological quality of included studies. The present study provides a comprehensive picture of the overall mental health of the COVID-19 outbreak which will guide the policymakers to measure the burden of similar pandemics more judiciously in the future.
Acknowledgments
Elezebeth Mathews would like to thank DBT, India for the Clinical and Public Health Early Career Fellowship (grant number IA/CPHE/17/1/503345).
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
SUPPLEMENTARY FILES
Supplementary Material 1
1. Example of search terms used in PubMed
| Search concept | MeSH terms and keywords |
|---|---|
| Prevalence | “Prevalence” [MeSH] OR “Epidemiology” [MeSH] |
| Anxiety | “Anxiety”[MeSH] OR “Anxiety Disorder” [MeSH] OR “Anxiety Disorders”[Text Word] “Social Anxieties” [Text Word] OR “Nervousness” [Text Word] OR Anxiousness [Text Word] |
| Depression | “Depression” [MeSH] OR “Depressive disorder”[MeSH] OR depression[Text Word] OR Depressive Symptoms [Text Word] Emotional Depression [Text Word] |
| COVID-19 | “COVID-19” [MeSH] OR “SARS Coronavirus 2” [MeSH] OR “COVID-19” [Text Word] OR “SARS-CoV-2 Infection” [Text Word] OR “2019 Novel Coronavirus Disease” [Text Word] OR “COVID-19 Virus Infection” [Text Word] OR Severe Acute Respiratory Syndrome Coronavirus 2 Infection [Text Word] OR COVID-19 Pandemic OR Wuhan Coronavirus [Text Word] OR 2019-nCoV OR SARS Coronavirus 2 [Text Word] |
| India | “India”[MeSH] OR “India” [Text Word] OR “South-east Asia” [Text Word] OR “low- and middle-income countries” [Text Word] |
2. Wiley online library (Search hits=784)
Topic: humans AND (depression OR anxiety) AND (COVID-19 OR pandemic) AND (India)
3. Science direct (Search hits=568)
Topic: humans AND (depression OR anxiety) AND (COVID-19 OR pandemic) AND (India)
Refined by: Journal Article, from January 1, 2020 to October 30, 2021
4. Google Scholar (first 30 pages: search hits=300)
Topic: humans AND (depression OR anxiety) AND (COVID-19 OR pandemic) AND (India)
Refined by: Journal Article, from 2020 to 2021
Relevant journals and search
Asian journal of psychiatry (12), Indian Journal of psychiatry (94), Indian Journal of social psychiatry (87), Indian Journal of psychological medicine (105), Annals of Indian psychiatry (15), Journal of mental health and human behavior (21), Journal of Family Medicine and Primary Care (289),International Journal of community medicine and public health (37), Indian Journal of psychiatric nursing (12), Kerala journal of psychiatry (1), Indian journal of community medicine (29), Indian journal of public health (64).
Search terms used: COVID-19, India, anxiety, depression
5. APA psych Info (search hits=359)
Topic: Any Field: COVID-19 AND Any Field: India AND Publication Type: Peer Reviewed Journal
-
Supplementary Material-2 Funnel Plot. Outcome: Prevalence of anxiety symptoms during COVID-19 pandemic among general population of India.
-
Supplementary Material-3 Funnel Plot. Outcome: Prevalence of depressive symptoms during COVID-19 pandemic among general population of India.
References
- Wuhan to world: The COVID-19 pandemic. Front Cell Infect Microbiol. 2021;11:596201.
- [CrossRef] [PubMed] [Google Scholar]
- Covid-19 infection in India: A comparative analysis of the second wave with the first wave. Pathogens. 2021;10:1222.
- [CrossRef] [PubMed] [Google Scholar]
- COVID-19, India, lockdown and psychosocial challenges: What next? Int J Soc Psychiatry. 2020;66:830-2.
- [CrossRef] [PubMed] [Google Scholar]
- The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113:531-7.
- [CrossRef] [PubMed] [Google Scholar]
- The mental health impact of the COVID-19 pandemic across different cohorts. Int J Ment Health Addict. 2022;20:380-6.
- [CrossRef] [PubMed] [Google Scholar]
- Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ. 2009;339:b2535.
- [CrossRef] [PubMed] [Google Scholar]
- Methodological guidance for systematic reviews of observational epidemiological studies reporting prevalence and cumulative incidence data. Int J Evid Based Healthc. 2015;13:147-53.
- [CrossRef] [PubMed] [Google Scholar]
- Measuring inconsistency in meta-analyses. BMJ. 2003;327:557-60.
- [CrossRef] [PubMed] [Google Scholar]
- A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1:97-111.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological impact of mass quarantine on population during pandemics-the COVID-19 lock-down (COLD) study. PLoS One. 2020;15:e0240501.
- [CrossRef] [PubMed] [Google Scholar]
- A study on the anxiety level and stress during Covid19 lockdown among the general population of West Bengal, India-a must know for primary care physicians. J Family Med Prim Care. 2021;10:978-84.
- [CrossRef] [PubMed] [Google Scholar]
- Dynamics of psychological responses to COVID-19 in India: A longitudinal study. PLoS One. 2020;15:e0240650.
- [CrossRef] [PubMed] [Google Scholar]
- Mental health concerns related to COVID-19 outbreak in the middle-aged and elderly population: A web-based, cross-sectional survey from Haryana, North India. J Geriatr Ment Health. 2020;7:100-4.
- [CrossRef] [Google Scholar]
- Depression, anxiety, and stress and socio-demographic correlates among general Indian public during COVID-19. Int J Soc Psychiatry. 2020;66:756-62.
- [CrossRef] [PubMed] [Google Scholar]
- Psychological impact of COVID-19 lockdown (Phase 2) among Indian general population: A cross-sectional survey. Int J Sci Res. 2020;9:51-6.
- [CrossRef] [Google Scholar]
- Impact of the COVID-19 pandemic on the mental health of college students in India: Cross-sectional web-based study. JMIRx Med. 2021;2:e28158.
- [CrossRef] [PubMed] [Google Scholar]
- Association of sociodemographic parameters with depression, anxiety, stress, sleep quality, psychological trauma, mental well-being, and resilience during the second wave of COVID-19 pandemic: A cross-sectional survey from India. Cureus. 2021;13:e16420.
- [CrossRef] [Google Scholar]
- Prevalence of posttraumatic stress disorder and depression in general population in India during COVID-19 pandemic home quarantine. Asia Pac J Public Health. 2021;33:154-6.
- [CrossRef] [PubMed] [Google Scholar]
- Anxiety, obsession and fear from coronavirus in Indian population: A web-based study using COVID-19 specific scales. Int J Community Med Public Health. 2020;7:4570-7.
- [CrossRef] [Google Scholar]
- Perceived stress and generalized anxiety in the Indian population due to lockdown during the COVID-19 pandemic: A cross-sectional study. F1000Res. 2020;9:1233.
- [CrossRef] [PubMed] [Google Scholar]
- Mental health problems and impact on youth minds during the COVID-19 outbreak: Cross-sectional (RED-COVID) survey. Soc Health Behav. 2020;3:83-8.
- [CrossRef] [Google Scholar]
- The psychological impact of the COVID-19 pandemic and associated risk factors during the initial stage among the general population in India. Open J Psychiatry Allied Sci. 2021;12:31-5.
- [CrossRef] [PubMed] [Google Scholar]
- A study of depression, anxiety and insomnia during COVID-19 lockdown (Special Issue: COVID-19 and demographic impact) Demogr India. 2020;49:140-52.
- [Google Scholar]
- Impact on anxiety of COVID-19 and lockdown. J Mar Med Soc. 2020;22:78-82.
- [CrossRef] [Google Scholar]
- Impact of lockdown following COVID-19 on the gaming behavior of college students. Indian J Public Health. 2020;64:S172-6.
- [CrossRef] [PubMed] [Google Scholar]
- Impact of COVID-19 pandemic on psychological responses of the general population in India: A nationwide survey. Int J Pharm Res. 2020;12:2349-57.
- [CrossRef] [Google Scholar]
- Psychological impact of COVID-19 lockdown: An online survey from India. Indian J Psychiatry. 2020;62:354-62.
- [CrossRef] [Google Scholar]
- Mental health and quality of life during COVID-19 pandemic in Indian population. Int J Pharm Pharm Sci. 2020;12:74-9.
- [CrossRef] [Google Scholar]
- Impact of COVID-19 pandemic on mental health of general population in Kashmir Valley, India. Int J Res Med Sci. 2020;8:4011-6.
- [CrossRef] [Google Scholar]
- Psychosocial impact of COVID-19 lockdown on mental wellbeing among 11 states of India: A markov modeling approach. J Psychiatry Psychiatr Disord. 2020;4:158-74.
- [CrossRef] [Google Scholar]
- The psychological impact of COVID-19 and the subsequent social isolation on the general population of Karnataka, India. J Ideas Health. 2020;3:190-5.
- [CrossRef] [Google Scholar]
- Impact of COVID-19 pandemic on mental health in the general population: A systematic review. J Affect Disord. 2020;277:55-64.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Global Health. 2020;16:57.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of anxiety, depression, and psychological distress among the general population during the COVID-19 pandemic: A systematic review and meta-analysis. Int J Soc Psychiatry. 2021;67:892-906.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020;288:112954.
- [CrossRef] [PubMed] [Google Scholar]
- Second wave of COVID-19 pandemic in India: Barriers to effective governmental response. EClinicalMedicine. 2021;36:100915.
- [CrossRef] [PubMed] [Google Scholar]
- 2015-2016 Prevalence, Patterns and Outcomes, Supported by Ministry of Health and Family Welfare, Government of India, and, Bengaluru: Implemented by National institute of Mental Health and Neurosciences (NIMHANS). In Collaboration with Partner Institutions. 2015-2016. Available from: https://www.ruralindiaonline.org/en/library/resource/national-mental-health-survey-of-india-2015-16-summary [Last accessed on 2022 Apr 30]
- [Google Scholar]
- Mental health and psychosocial aspects of COVID-19 in India: The challenges and responses. J Health Manag. 2020;22:197-205.
- [CrossRef] [Google Scholar]
- COVID-19 and psychological distress: Lessons for India. PLoS One. 2021;16:e0255683.
- [CrossRef] [PubMed] [Google Scholar]







