Translate this page into:
Prevalence and consequences of stigma associated with migraine in a rural Indian headache clinic
*Corresponding author: Soaham Desai, Department of Neurology, Shree Krishna Hospital, Pramukhswami Medical College, Bhaikaka University, Anand, Gujarat, India. drsoahamdesai@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Shukla S, Joshi D, Desai D, Patel MR, Desai S. Prevalence and consequences of stigma associated with migraine in a rural Indian headache clinic. J Neurosci Rural Pract. 2025;16:61-7. doi: 10.25259/JNRP_308_2024
Abstract
Objectives
Migraine, a prevalent neurological disorder, remains under-recognized and stigmatized, potentially impeding optimal management. This study aimed to quantify migraine-related stigma and its associations in a rural Indian setting, addressing a critical knowledge gap in low-resource contexts. Primary objectives: This study was to assess the prevalence and patterns of perceived stigma among migraine patients in a rural neurology clinic. Secondary objectives: This study was to examine the relationship between stigma levels and headache impact severity and to identify sociodemographic factors associated with higher stigma.
Materials and Methods
This cross-sectional study enrolled 100 migraine patients diagnosed per International Classification of Headache Disorders, 3rd edition criteria at a rural tertiary care hospital in Gujarat, India. Perceived stigma was measured using the culturally adapted stigma scale for chronic illness (SSCI-8), and headache impact was assessed using the headache impact test (HIT-6). Correlations and regression analyses were performed to evaluate associations.
Results
The mean total SSCI-8 score was 16.77 (standard deviation = 5.98), indicating moderate perceived stigma. A significant positive correlation was observed between total SSCI-8 and HIT-6 scores (r = 0.25, P = 0.014), persisting after adjustment for confounders (adjusted r = 0.22, P = 0.027). Participants with only primary education reported significantly higher enacted (P < 0.001) and internalized (P = 0.027) stigma compared to those with higher education. Regular clinic follow-up was associated with lower stigma scores (P = 0.001).
Conclusion
This study revealed substantial perceived stigma among migraine patients in rural India, with a novel finding of a non-linear relationship between education levels and stigma. The significant association between stigma and headache impact underscores the need for targeted interventions. These insights can inform the development of culturally sensitive, community-based anti-stigma initiatives and support services, potentially improving migraine management and outcomes in underserved rural populations.
Keywords
Disability
Migraine
Severity Scores
Stigma
INTRODUCTION
Migraine has been recognized as a significant global health concern, ranking second in years lived with disability according to the global burden of disease study 2016.[1] This highlights its substantial impact on individuals and societies worldwide. In India, the prevalence of migraine is notably high, particularly in rural areas, where it ranges from 14.1% to 25.2%.[2,3] Despite its high prevalence, migraine remains under-recognized and under-treated in these regions, largely due to limited access to healthcare and cultural beliefs.
Stigma, a pervasive issue in chronic illnesses, significantly impacted patients’ quality of life, mental health, and treatment adherence in the past.[4,5] For individuals with migraine, stigma led to social isolation, decreased self-esteem, and reluctance to seek medical help, thereby exacerbating the burden of the disease.[6,7] The previous studies indicated that stigma was a common experience among migraine patients, associated with greater disability and reduced quality of life.[8,9] The invisible nature of migraine, its episodic pattern, and the misconception that it is “just a headache” contributed to its stigmatization.[10,11] Despite the growing recognition of the stigma in migraine, research in low-resource, rural settings like India was scarce, highlighting a critical knowledge gap. Cultural factors and traditional beliefs in these areas may amplify stigma, impacting treatment-seeking behavior and disease management.
This study aimed to assess the prevalence and consequences of stigma associated with migraine in a rural neurology clinic in Western India. By exploring sociodemographic factors and their association with stigma levels, the study sought to inform the development of culturally sensitive interventions to reduce stigma and improve migraine management in underserved rural populations.
MATERIALS AND METHODS
Study design and setting
A cross-sectional study was done at the outpatient neurology department of Shree Krishna Hospital, a rural tertiary care teaching hospital in Karamsad, Gujarat, India, over a 14-month period between January 2020 and April 2021. The hospital serves a predominantly agrarian population of approximately 1.5 million from 150 surrounding villages within a 75-km radius.
Participants
Eligible participants were patients with age 18 years and older, attending the neurology clinic and diagnosed with migraine (using the International Classification of Headache Disorders, 3rd edition criteria)[12] by a board-certified neurologist (standard deviation [SD]). Participants were recruited through consecutive sampling during routine clinic visits. Exclusion criteria included severe cognitive impairment (IQ < 50), dementia [Mini-Mental State Examination < 24 and Frontal Assessment Battery < 12], or conditions precluding valid self-reporting.[13,14] The sample size was calculated to be at least 100 participants, accounting for potential subgroup analyses.
Sample size calculation
With a significance threshold of 0.05 and a power of 0.80, the sample size was determined using the G*Power software (version 3.1.9.4), assuming a medium effect size (f2 = 0.15) for the relationship between stigma and headache impact. A sample of 92 participants was needed according to this calculation. To account for potential subgroup analyses and ensure adequate power for detecting smaller effect sizes in secondary analyses, the sample size was increased by 10%, aiming to recruit at least 100 participants.
Study measures
The primary variables were perceived stigma, measured using the stigma scale for chronic illness (SSCI-8),[15] and headache impact, assessed using the - (HIT-6).[16] Both instruments were translated into Gujarati and culturally adapted through forward-backward translation and cognitive debriefing with ten migraine patients.
Data collection
Ethical approval was obtained from the Institutional Ethics Committee (IEC No: IEC/HMPCMCE/105/Faculty/5/237/20). Written informed consent was obtained from all participants before enrolment. Data were collected through in-person interviews using the SSCI-8 and HIT-6, conducted by a trained medicine resident not involved in participants’ clinical care. Sociodemographic and clinical data were collected through interviews and medical record review.
Statistical analysis
Variable distributions in the study were assessed using descriptive statistics. Pearson’s correlation assessed the relationship between SSCI-8 and HIT-6 scores. Partial correlation and multivariate linear regression analyses were done to adjust for confounders, including age, gender, education level, and migraine chronicity.[17] About 95% confidence intervals were included with effect sizes. Missing data were handled using pairwise deletion for correlation analyses and multiple imputation for regression models, assuming data were missing at random. Analyses were performed using Stata 16.1 software, adhering to STROBE guidelines for reporting observational studies.[18]
RESULTS
Participant flow
A total of 112 consecutive migraine patients were assessed for eligibility. Six patients were excluded due to cognitive impairment, and six declined to participate, resulting in a final sample of 100 participants included in the analysis.
Demographic characteristics
The study population comprised 100 participants with a mean age of 38.96 years (SD = 10.96). The majority were female (64%) and married (84%). Educational attainment was high, with 92% having at least a secondary education, including 29% who were graduates. Occupation distribution showed that 48% were housewives, and 31% were employed. Detailed demographic characteristics are presented in Table 1.
| Parameters | Frequency (%) Migraine (N=100) |
SSCI enacted stigma Mean (SD) |
SSCI internalized stigma Mean (SD) |
HIT-6 Mean (SD) |
|---|---|---|---|---|
| Age | ||||
| 18–20 years | 3 (3.0) | 11.00 (5.29) | 8.00 (5.00) | 60.67 (7.02) |
| 21–30 years | 23 (23.0) | 7.65 (3.17) | 7.61 (3.47) | 61.17 (7.34) |
| 31–40 years | 31 (31.0) | 9.03 (3.98) | 8.32 (3.06) | 59.45 (10.87) |
| 41–50 years | 26 (26.0) | 8.85 (3.65) | 8.31 (3.02) | 60.54 (9.64) |
| 51–60 years | 16 (16.0) | 8.69 (4.00) | 8.12 (2.83) | 61.69 (8.54) |
| 61–70 years | 0 (0.0) | NA | NA | NA |
| 71–80 years | 1 (1.0) | 9.00 (NA) | 7.00 (NA) | 58.00 (NA) |
| Gender | ||||
| Male | 36 (36.0) | 8.14 (3.28) | 7.47 (2.65) | 56.67 (9.29) |
| Female | 64 (64.0) | 8.97 (3.94) | 8.45 (3.30) | 62.67 (8.42) |
| Marital status | ||||
| Unmarried | 11 (11.0) | 8.91 (4.37) | 7.91 (3.83) | 60.64 (6.68) |
| Married | 84 (84.0) | 8.69 (3.74) | 8.19 (3.09) | 60.58 (9.49) |
| Divorced | 1 (1.0) | 10.00 (NA) | 8.00 (NA) | 45.00 (NA) |
| Widow | 4 (4.0) | 7.25 (1.26) | 6.75 (0.96) | 62.50 (6.61) |
| Education | ||||
| Uneducated | 2 (2.0) | 8.00 (1.41) | 4.00 (1.41) | 66.50 (0.71) |
| Primary | 6 (6.0) | 12.0 (5.02) | 10.17 (4.02) | 57.83 (9.26) |
| Secondary | 24 (24.0) | 9.92 (4.52) | 8.75 (3.05) | 61.8 (10.12) |
| Higher secondary | 16 (16.0) | 10.5 (3.71) | 9.38 (2.75) | 61.38 (7.70) |
| Diploma | 18 (18.0) | 7.00 (2.06) | 7.11 (2.74) | 58.11 (7.59) |
| Graduate | 29 (29.0) | 7.59 (2.64) | 7.76 (2.90) | 60.1 (10.11) |
| Postgraduate | 5 (5.0) | 5.40 (0.89) | 5.60 (2.79) | 63.4 (10.99) |
| Occupation | ||||
| Unemployed | 1 (1.0) | 11.00 (NA) | 10.00 (NA) | 66.00 (NA) |
| Housewife | 48 (48.0) | 8.90 (4.00) | 8.79 (3.13) | 63.38 (7.89) |
| Laborer | 9 (9.0) | 10.8 (4.47) | 8.89 (2.71) | 54.2 (11.77) |
| Student | 7 (7.0) | 8.43 (3.99) | 7.29 (3.30) | 60.57 (8.00) |
| Employed | 31 (31.0) | 7.90 (3.04) | 6.97 (3.03) | 58.00 (9.77) |
| Retired | 4 (4.0) | 7.00 (1.83) | 7.75 (2.22) | 58.25 (3.69) |
| Disease in family | ||||
| Present | 39 (39) | 8.74 (3.70) | 8.51 (3.34) | 59.79 (9.09) |
| Absent | 61 (61) | 8.62 (3.76) | 7.84 (2.94) | 60.97 (9.26) |
| Follow-up | ||||
| Irregular | 20 (20.0) | 10.8 (4.56) | 9.15 (3.36) | 60.8 (11.22) |
| Regular | 80 (80.0) | 8.14 (3.30) | 7.84 (3.00) | 60.44 (8.66) |
| Duration | ||||
| Months | 28 (28.0) | 9.18 (4.89) | 8.21 (2.73) | 60.36 (8.36) |
| Years | 72 (72.0) | 8.47 (3.17) | 8.06 (3.25) | 60.57 (9.52) |
| Other medical illness | ||||
| None | 60 (60.0) | - | - | - |
| Anxiety | 14 (14.0) | - | - | - |
| Depression | 7 (7.0) | - | - | - |
| Hypertension | 4 (4.0) | - | - | - |
| Diabetes mellitus | 7 (7.0) | - | - | - |
| Dysthymia | 6 (6.0) | - | - | - |
| Thyroid disorder | 1 (1.0) | - | - | - |
| COPD | 1 (1.0) | - | - | - |
SSCI: Stigma scale for chronic illness, HIT-6: Headache impact test-6, SD: Standard deviation, N: Number of individuals with migraine, NA: Not available, COPD: Chronic obstructive pulmonary disease
Migraine characteristics
Participants had a mean duration of migraine of 6.8 years (SD = 5.1), with 39% reporting a positive family history of migraine. The mean attack frequency was 5.2 per month (SD = 3.8), and 32% experienced ≥ 8 attacks monthly.
Stigma scores
The mean total SSCI-8 score was 16.77 (SD = 5.98), with a median of 16 (Interquartile range = 12–20) and a range of 8–34. The enacted stigma subscale had a mean score of 8.67 (SD = 3.72), while the internalized stigma subscale averaged 8.10 (SD = 3.10). The HIT-6 mean score was 60.51 (SD = 9.17), indicating substantial impact on daily life.
Correlations
A weak but statistically significant positive correlation was observed between total SSCI-8 scores and HIT-6 scores (r = 0.25, P = 0.014) [Figure 1]. Enacted stigma showed a significant correlation with HIT-6 scores (r = 0.20, P = 0.047), while internalized stigma did not (r = 0.15, P = 0.14).
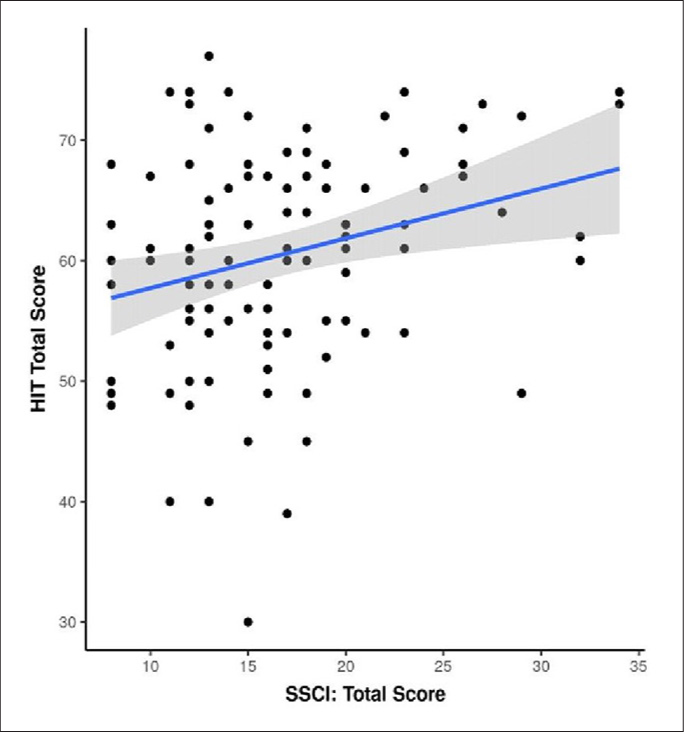
- Scatterplot depicts the correlation between SSCI: Total score and HIT score. The blue trendline represents the general trend of correlation between the two variables. The shaded gray area represents the 95% confidence interval of this trendline. There is a positive correlation between perceived stigma levels (Total SSCI-8 score) and headache impact severity (HIT-6) (r = 0.25). SSCI: Stigma scale for chronic illness, HIT: Headache impact test.
Regression analysis
Regression analysis revealed significant associations between demographic factors and stigma scores. Widowed status was associated with significantly lower total SSCI-8 scores compared to unmarried participants (β = –14.43, P = 0.006). Education level showed a nonlinear relationship with stigma, where primary, secondary, higher secondary, and graduate education levels were associated with higher SSCI-8 scores compared to uneducated participants [Figure 2]. Regular follow-up was associated with significantly lower stigma scores (mean difference = –4.32, 95% CI: –6.89 to –1.75, P = 0.001), and this association persisted after adjusting for disease severity and sociodemographic factors (adjusted β = –0.20, 95% CI: –0.34 to –0.06, P = 0.005). There were no statistically significant correlations between HIT-6 scores and demographic characteristics, indicating that headache impact was consistent across subgroups. Multiple imputations for missing data (3.5% of total data points) did not substantially alter the main findings, indicating minimal impact on results.
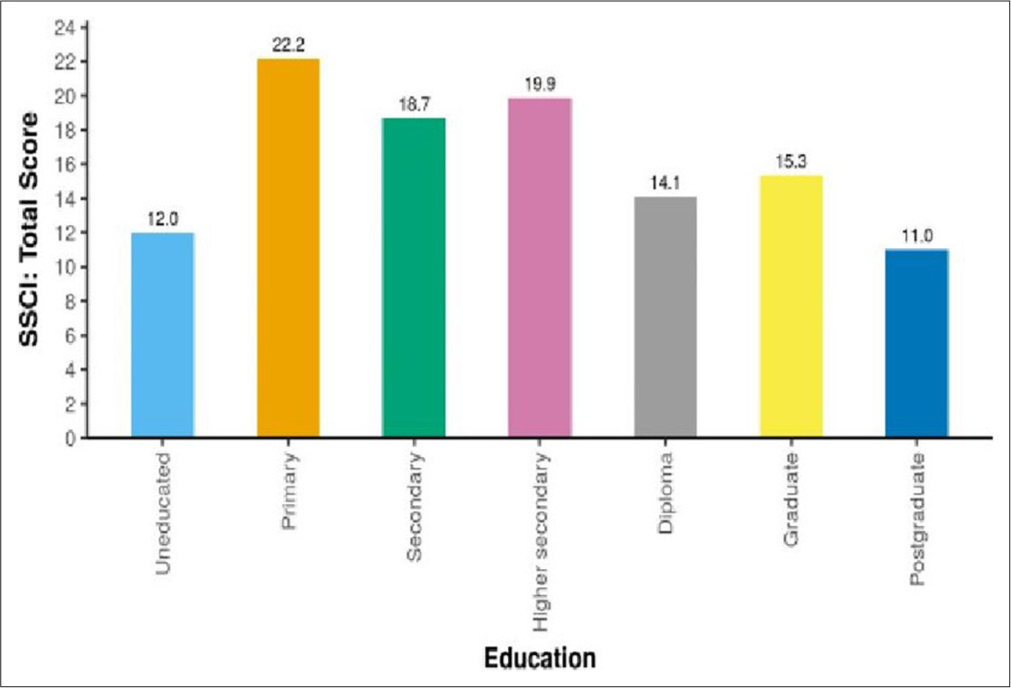
- Association between education and stigma severity in chronic illness (SSCI: Total Score) depicting highest stigma scores in patients with primary education followed by higher secondary and secondary education, respectively. Postgraduates have least stigma scores. SSCI: Stigma scale for chronic illness.
DISCUSSION
This study provides novel insights into the prevalence and patterns of perceived stigma among individuals with migraine in a rural Indian setting, addressing a critical gap in our understanding of migraine-related stigma in low-resource regions. Our findings reveal a complex interplay between sociodemographic factors, clinical characteristics, and perceived stigma, with important implications for migraine management and public health interventions in rural populations.
According to the HIT-6 instrument, there was a positive link between higher perceived stigma and more severe headache effect, a finding that is consistent with other studies conducted in different contexts.[19] This association persisted after adjusting for potential confounders, suggesting a robust relationship between stigma and migraine burden. Several mechanisms may underlie this relationship. Stigma-related stress could exacerbate migraine pathophysiology through allostatic load mechanisms.[20] In addition, perceived stigma may create barriers to care-seeking and treatment adherence, potentially leading to suboptimal management and increased disability.[6] The visibility of severe migraine phenotypes may also heighten experiences of enacted stigma, creating a potential feedback loop.
Our study revealed lower overall stigma scores compared to previous research in other settings [Table 2].[9,19] This unexpected finding warrants careful consideration. Several factors may contribute to this difference. Studies show migraine to be more prevalent with a greater global burden of disease in high-income countries than in South Asian countries.[1,21] This might cause individuals to contemplate on the diseases that are more prevalent in a particular geographical region. Along with geographical variations, disease is influenced by geo-economic and psychosocial factors.[22] Cultural variations in the conceptualization and expression of stigma could play a role, with rural Indian populations potentially having different frameworks for understanding and reporting stigma experiences. The adaptation of the SSCI-8 instrument to the local context may have also influenced response patterns. In addition, the lower scores could reflect a genuine difference in stigma experiences in this population, possibly due to stronger community support systems or different societal attitudes toward neurological disorders in rural India.
| Parameters | Present study (%) | Young et al.[9] (%) | Martínez-Fernández et al.[19] (%) | |||
|---|---|---|---|---|---|---|
| M (N=100) | P–value | EM (N=123) | CM (N=123) | EM (N=56) | CM (N=18) | |
| Age | 38.96±10.98 | 0.65 | 44.76±12.5 | 40.96±12.2 | 38.4±11.9 | 46.1±10.4 |
| Gender | 0.38 | |||||
| Male | 36.0 | 17.1 | 15.4 | 5.4 | 5.6 | |
| Female | 64.0 | 82.9 | 84.6 | 94.6 | 94.4 | |
| Education | <0.001 | |||||
| Uneducated | 2.0 | - | - | - | - | |
| Primary | 6.0 | - | - | 1.8 | 0 | |
| Secondary | 24.0 | - | - | 17.9 | 33.3 | |
| Higher Secondary/Some College | 16.0 | 27.6 | 41.4 | 80.4 | 66.7 | |
| Graduate/Bachelor | 29.0 | 66.7 | 49.6 | |||
| Post-graduation | 5.0 | - | - | |||
| Diploma/Associate | 18.0 | 5.7 | 8.9 | |||
| Total SSCI Score | 16.77±5.98 | 41.76±14.8 | 54.06±20.2 | 45.0±13.5 | 51.06±15.0 | |
| SSCI-I | 8.10±3.10 | 26.16±10.0 | 34.56±12.9 | 29.1±9.7 | 33.0±11.1 | |
| SSCI-E | 8.67±3.72 | 14.96±5.8 | 19.56±8.3 | 15.8±5.2 | 18.6±5.8 | |
| HIT-6 | 60.51±9.17 (median 61) | - | - | 64.4±6.0 (median 66) | 64.3±7.9 (median 65) | |
| MIDAS | - | 28.54±38.7 | 86.5±77.86 | - | - | |
M: Migraine, EM: Episodic migraine, CM: Chronic migraine, SSCI-I: Stigma scale for chronic illness internalized, SSCI-E: Stigma scale for chronic illness enacted, HIT-6: Headache impact test-6; N: Frequency, MIDAS: Migraine disability assessment scale. P< 0.05 is considered statistically significant
A key finding of our study is the non-linear relationship between education levels and stigma scores. Comparing participants with basic to undergraduate education to those with graduate or postgraduate education, the former showed noticeably greater levels of stigma. This contrasts with the linear relationship often assumed in health disparities research. Several factors may contribute to this pattern. Individuals with very low education may have limited exposure to societal misconceptions about migraine, while those with higher education may have better access to accurate information and resources to counter stigmatizing attitudes. The intermediate group may be more vulnerable to internalized stigma due to greater awareness of societal attitudes without the tools to effectively challenge them. This finding highlights the need for tailored anti-stigma interventions targeting vulnerable groups with lower education levels. Public health campaigns and educational programs should be designed to address the specific needs and misconceptions prevalent in these populations. Healthcare providers in rural settings should be trained to recognize and address stigma-related barriers to care, particularly among patients with intermediate education levels.
Our study revealed an unexpected finding: Widowed women with migraine reported significantly lower stigma scores compared to unmarried women. This could be attributed to differing social perceptions, with widows potentially experiencing more empathy, while unmarried women face stricter societal expectations. However, as the sample size of widowed participants was low, this observation should be interpreted cautiously. To confirm this conclusion and investigate the underlying sociocultural elements that can affect stigma experiences among various marital status groups in the migraine community, future studies with larger, more diverse populations are required.
The association between regular clinic follow-up and lower stigma scores is an intriguing finding with potential implications for clinical practice. This relationship may be reciprocal: people who feel less stigmatized are more likely to seek care on a frequent basis, and regular medical follow-up may lessen stigma by providing support and knowledge. Clinicians should be aware of the potential benefit of regular follow-up and consider strategies to encourage consistent engagement with care, particularly for patients at higher risk of experiencing stigma.
This study has a number of limitations that should be noted. Causal judgments about the observed connections are not possible due to the cross-sectional design. Our study sample size is adequate for the primary analysis but may have limited power for detecting smaller effect sizes in the subgroup analyses. Selection bias is possible, as individuals seeking care at a tertiary center may differ systematically from those who do not access such care. The study population might not be representative of all migraine sufferers because it was selected from a single rural tertiary care facility. The self-report scales used in the study may have recall bias and social desirability effects. Future research should address these limitations through longitudinal designs, larger and more diverse rural and urban samples, and the inclusion of other objective measures of migraine severity, psychiatric comorbidity, and impact. Qualitative studies could provide deeper insights into the lived experiences of stigma among rural Indian migraine patients and help elucidate the mechanisms underlying the observed associations. In addition, intervention studies testing targeted anti-stigma programs in this population are needed to translate these findings into improved patient outcomes.
CONCLUSION
Our research indicates a moderate level of perceived stigma among migraine patients in rural India, with a significant positive correlation between stigma and headache impact. Interestingly, education level showed a non-linear association with stigma, with higher stigma reported among those with primary to undergraduate education compared to those with higher educational attainment. Participants who attended regular clinic follow-ups reported lower levels of stigma. Our study results suggest that tailored interventions are needed to fight stigma and make things better for people with migraine.
Data availability statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethical approval
The research/study approved by the Institutional Review Board at H M PATEL CENTRE FOR MEDICAL CARE AND EDUCATION, KARAMSAD, number IEC/HMPCMCE/105/Faculty/5/237/20, dated 13/05/2019.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Global, regional, and national burden of migraine and tension-type headache, 1990-2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. 2018;17:954-76.
- [CrossRef] [PubMed] [Google Scholar]
- Headache disorders and public ill-health in India: Prevalence estimates in Karnataka State. J Headache Pain. 2015;16:67.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence, burden, and risk factors of migraine: A community-based study from Eastern India. Neurol India. 2017;65:1280-8.
- [CrossRef] [PubMed] [Google Scholar]
- The social psychology of stigma. Annu Rev Psychol. 2005;56:393-421.
- [CrossRef] [PubMed] [Google Scholar]
- Stigma and migraine: Developing effective interventions. Curr Pain Headache Rep. 2021;25:75.
- [CrossRef] [PubMed] [Google Scholar]
- The health stigma and discrimination framework: A global, crosscutting framework to inform research, intervention development, and policy on health-related stigmas. BMC Med. 2019;17:31.
- [CrossRef] [PubMed] [Google Scholar]
- Migraine-related stigma and its relationship to disability, interictal burden, and quality of life: Results of the OVERCOME (US) study. Neurology. 2024;102:e208074.
- [CrossRef] [PubMed] [Google Scholar]
- The passing dilemma in socially invisible diseases: Narratives on chronic headache. Soc Sci Med. 2007;65:1619-29.
- [CrossRef] [PubMed] [Google Scholar]
- Headache classification committee of the international headache society (IHS) the international classification of headache disorders In: Cephalalgia Vol 38. (3rd edition). 2018. p. :1-211.
- [CrossRef] [PubMed] [Google Scholar]
- “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189-98.
- [CrossRef] [PubMed] [Google Scholar]
- The FAB: A frontal assessment battery at bedside. Neurology. 2000;55:1621-6.
- [CrossRef] [PubMed] [Google Scholar]
- The stigma scale for chronic illnesses 8-item version (SSCI-8): Development, validation and use across neurological conditions. Int J Behav Med. 2013;20:450-60.
- [CrossRef] [PubMed] [Google Scholar]
- Validation of the Headache Impact Test (HIT-6™) across episodic and chronic migraine. Cephalalgia. 2011;31:357-67.
- [CrossRef] [PubMed] [Google Scholar]
- The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet. 2007;370:1453-7.
- [CrossRef] [PubMed] [Google Scholar]
- Psychosocial repercussion of migraine: Is it a stigmatized disease? Neurol Sci. 2020;41:2207-13.
- [CrossRef] [PubMed] [Google Scholar]
- Taking the headache out of migraine. Neurol Clin Pract. 2015;5:317-25.
- [CrossRef] [PubMed] [Google Scholar]
- The global prevalence of headache: An update, with analysis of the influences of methodological factors on prevalence estimates. J Headache Pain. 2022;23:34.
- [CrossRef] [PubMed] [Google Scholar]
- Migraine: Epidemiology and systems of care. Lancet. 2021;397:1485-95.
- [CrossRef] [PubMed] [Google Scholar]







