Translate this page into:
Posterior epidural migration of herniated disc: A case series and literature review
*Corresponding author: Maria Ilaria Borruto, Policlinico Agostino Gemelli, IRCSS, Rome, Italy. maria.ilaria.borruto@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Borruto MI, Perna A, Velluto C, Santagada D, Genitiempo M, Tamburrelli F, et al. Posterior epidural migration of herniated disc: A case series and literature review. J Neurosci Rural Pract. 2025;16:1-7. doi: 10.25259/JNRP_374_2024
Abstract
Posterior epidural space migration of fragment herniated discs represents a rare condition related to the spine’s anatomy and only a few cases have been reported. Radiologic differential diagnosis by epidural occupying space lesions is challenging for spinal surgeons. In order to analyze the incidence, anatomy, symptoms, and imaging that can help in differential diagnosis, management, and prognosis of posterior epidural migration of herniated disc fragments, we performed a systematic literature review of all clinical studies of posterior epidural disc fragments published to date. Moreover, we reported five clinical cases from our department, in which good outcomes were obtained after surgical decompression. We identified 108 cases of posterior epidural migration of herniated discs, 50% of patients were aged 40–59, and 82.5% were male. In 63% of cases, motor function was involved, in 56%, there was sensory loss, in 36% hyporeflexia and 37% sphincter disorders. Magnetic resonance imaging was the diagnostic imaging chosen in 78% of cases, but in 32 cases, surgeons could not make a differential diagnosis before seeing intraoperative findings. Open surgery was the treatment choice in 97% of cases, 1 case was treated with an endoscopic approach, and 3 cases reported spontaneous regression. Full recovery was described in 55% of cases, in 31% an improvement without substantial deficits, and in 14% sequelae, usually with complications related to the urinary system. Taking everything into account, open surgery is considered the best choice since surgeons are often unable to make a definitive diagnosis based solely on radiological imaging; pathological confirmation is typically required.
Keywords
Cauda
Herniated disc fragment
Laminectomy
Laminotomy
Posterior migration
INTRODUCTION
Intervertebral disc herniation (IDH) is a very frequent degenerative disease. Low back pain and sciatica related to IDH are one of the most frequent causes of spine surgery.[1] The herniated fragment is usually composed of the pulposus nucleus of the intervertebral disc. Often, disc fragments migrate into epidural space because of the presence of the posterior longitudinal ligament (PLL) and the peridural membrane, the lateral membrane that is linked to PLL.[2] Some authors in the literature estimated that 35–72% of disc herniations in the lumbar spine present a fragment migration, usually in the anterolateral epidural space.[3,4] Posterior epidural space disc fragment migration represents a rare event, and only a few cases have been reported.[5-7]
Literature suggests that in cases of disc herniation, job-related factors like heavy physical strain may cause spinal degeneration and related consequences. Jobs that require lifting with a torqued spine or straight knees have been associated with a higher risk of disc injury; instead, the natural history of dorsal disc herniation is still not well known. When a herniated disc pierces the annulus fibrosus and PLL with the migration of the disc fragment to the epidural space, disc sequestration takes place.[8] In this paper, we reported 4 cases of posterior epidural herniation and conducted a systematic review of the pertinent literature on the epidemiology, clinical and radiological features, treatment protocols, and outcomes.
MATERIALS AND METHODS
Study setting and design
A systematic literature review based on the preferred reporting items for systematic reviews and meta-analyses (PRISMA) guidelines [Figure 1] was performed in the present study.
Inclusion and exclusion criteria
In this review, the full–text articles reporting clinical and radiological characteristics of patients with posterior epidural migration of herniated disc fragments were considered eligible. Only English-language articles were included. No date range for publication was set. Letters to the editors, unpublished reports, in vitro and on animal studies, abstracts from Congress, and book chapters were excluded from the review.
Search strategy and study selection
Scopus, MEDLINE via PubMed, Cochrane Library database, and Embase, were searched using the keywords: “Posterior epidural space,” “herniated disc,” “disc migration,” “discal hernia,” “dorsal migration,” “sequestered lumbar disc” and their medical subject headings (MeSH) terms in any possible combinations using the logical operators “AND” and “OR.” The reference lists of relevant studies were forward-screened to identify other studies of interest. The search was reiterated until January 30, 2024.
The PRISMA was followed as reported in Figure 1.
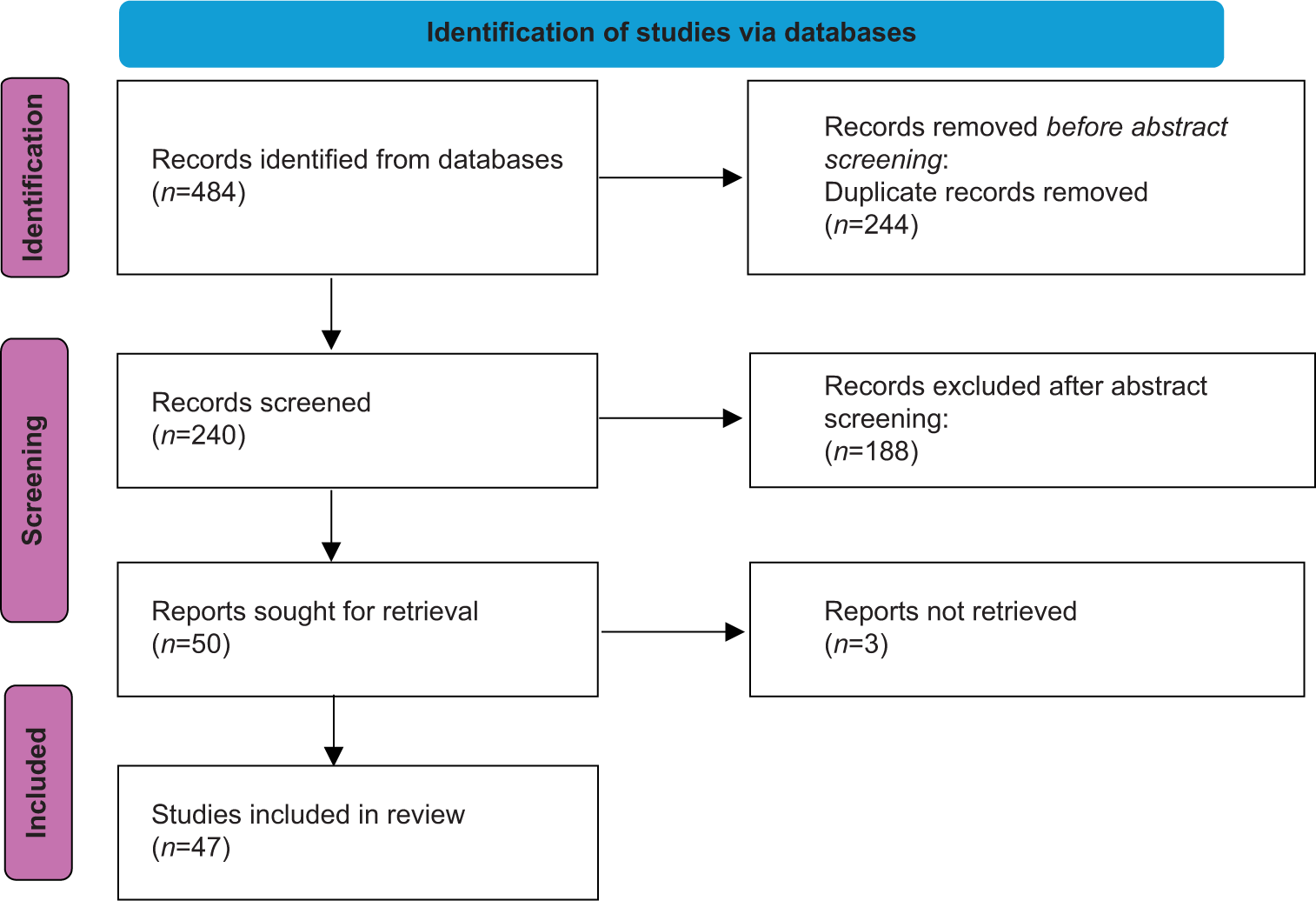
- Preferred reporting items for systematic reviews and meta–analyses flow–chart.
After the screening of 474 titles and abstracts, (243 after screening duplicates), 56 papers were considered fit for selection for the full–text analysis. Ultimately, fifty–one studies that met the inclusion criteria were included in the review. In summary, including our report, 108 patients affected by posterior epidural migration of herniated discs were analyzed in this systematic review [Supplementary Table 1].[5,6,9-57]
Data extraction and analysis
Two independent authors (M.I.B. and A.P.) conducted the search and collected data from the included studies. Any discrepancies were resolved through consensus with a third author (D.A.S.). The following data were extracted: Demographic information, affected discal level, surgical treatment, radiological diagnosis, and radiological description. Numbers software (Apple Inc., Cupertino, CA) was used to collect and categorize the obtained data. Categorical variables are presented as frequencies and percentages, while continuous variables are presented as means and standard deviations. Only one decimal place was reported and rounded accordingly.
CASE SERIES
Case 1
A 76-year-old male affected by non–Hodgkin’s lymphoma was transferred to our emergency unit for lower back pain for 3 days, left leg iposteny, and weakness in both legs. He had a history of colon adenocarcinoma, non-Hodgkin’s lymphoma, and multiple percutaneous coronary interventions (PCI). A neurologic examination revealed plegia of the left leg, and the power in hip flexion was 3/5. Reflexes were absent in both legs, and hyporeflexia was present in both arms. X–rays showed no sign of fractures. Magnetic resonance imaging (MRI) showed a disc protrusion L1–L2 [Figure 2], and at the same level, an epidural mass, isointense on T1– T1-weighted images, hyperintense on T2–weighted images. The imaging was consistent with the epidural abscess. L1– L2 left laminotomy was performed. After removing the ligamentum flavum, a disc fragment was identified on the left lateral and posterior aspect of the dural sac [Figure 3], we proceeded with the herniotomy. At the end of the procedure, the dural sac appeared loose of compressions. Pathologic analysis confirmed intraoperative findings. Microbiological analysis was carried out on the presence of Staphylococcus Epidermidis in 1 sample of 6, which was considered, according to specialists in infectious disease, a contaminant. A few days after surgery, we observed pain relief and an improvement in both leg’s strength. Due to his cardiologic history, he was undergoing antiaggregant and anticoagulant therapy that caused an important hematoma, which slowed rehabilitation.

- T2–weighted images, showing (a) herniated disc that compresses dural sac, moreover an hyperintense lesion posterior to the vertebral canal, (b) intraoperative findings.

- Disc fragment after removal.
Case 2
A 47-year-old man was admitted to our emergency unit for lower radiculopathies [visual analogue scale (VAS) leg 8], and urinary and fecal retention. A neurologic examination was performed. The motor power in knee flexion bilaterally was 3/5. Hypoesthesia was found in the L4–L5 region bilaterally. In a blood test, no alterations in erythrocyte sedimentation rate, leukocyte, and activated protein C were found. A preoperative MRI of the lumbosacral spine was performed. A big fragment of the intervertebral disc was expelled posteriorly to the dural sac causing compression of the nerves of the cauda equina. A huge bladder for urinary retention is clearly evident, as an incidental feature, on wide MRI sagittal view. The diagnosis was compatible with acute onset of cauda equina syndrome (CES) due to L4–L5 disc herniated disc disease. The operation was performed 12 h after admission. We used a left hemi-laminectomy at the L3 level with the posterior approach. After the removal of the ligamentum flavum, a big disc herniation migrates in the dorsal epidural space was found. We proceeded with the herniotomy. At the end of the procedure, the dural sac appeared loose of compressions. The day after the operation, we observed substantial pain relief (Vas leg 4). The motor power in knee flexion was 4/5 on the right side and 3/5 on the left side. Fifteen days after the operation, urinary retention was resolved. At the one-month follow-up evaluation, the motor power in left knee flexion was 4/5; no other deficit was found.
Case 3
A 45-year-old man was admitted to our emergency unit for acute right sciatica with hypoesthesia in the L4–L5 right region. At the admission, the VAS leg was 8. The patient was a workman affected by chronic lower back pain. Acute sciatica was presented after moving a heavy object during work. A neurologic examination was performed. No deficit was found. In a blood test, no alterations in erythrocyte sedimentation rate, leukocyte, and activated protein C were found. An MRI of the lumbosacral spine was performed. A big fragment of the intervertebral disc was expelled in the right side of the posterior epidural space from the L4 to L5 disc. In the axial section of the MRI, the disk fragment compressed and dislocated the dural sac. The operation was performed 48 h after admission. We used right hemilaminectomy at the L4 level with a posterior approach. After the removal of the ligamentum flavum, a big disc herniation migrates in the dorsal epidural space was found. We proceeded with the herniotomy. At the end of the procedure, the dural sac appeared loose of compressions. The day after surgery, we found good pain relief (VAS leg 2). The patient was discharged 2 days after the operation. At 1-month follow-up evaluation, no hypoesthesia was found and the patient had no pain.
Case 4
A 52-year-old man was admitted to our emergency room for low back pain and sciatica for 8 days and urinary retention. A neurological examination revealed saddle sensory loss, no loss in leg strength, plantar and Achilles reflexes were decreased in both legs, and cremasteric reflex was absent on the left side. Computed tomography (CT) scan and MRI were performed and showed at L4–L5 level a rent in the posterior annulus through which a coarse disc fragment found a path to the dorsal aspect of the dural sac.
A right laminectomy L4–L5 was performed, after which the dural sac was no longer compressed.
A week after surgery, he experienced an improvement in all neurological deficits, and after three weeks, he had a full recovery.
Case 5
A 47-year-old man presented to the emergency department with acute low back pain and urinary retention. Neurological examination revealed motor and sensory deficits in the lower limbs, prompting an MRI, which showed posterior compression suggestive of an epidural abscess. The patient underwent urgent laminectomy, during which a posteriorly migrated disc fragment was discovered posterior to the dural sac and subsequently removed. He was then transferred to neurological rehabilitation, where he demonstrated a full recovery, confirmed at the 3-month follow-up.
RESULTS AND DISCUSSION
Epidemiology of dorsal disc migration
Although sequestered disc fragments account for 28.6% of all disc herniations,[58] migration to the posterior epidural space or into the dural sac is rare, with an incidence rate of about 0.27–1.04%.
We identified 108 patients, including our report, with posterior epidural migration of herniated disc, of mean age 53,58 (Standard deviation = 11,18201527). Most patients (n = 52; 50%) were aged 40–59. In addition, of the identified patients, 86 (82.5%) were male, which suggests that posterior epidural lumbar disc fragment occurs mainly in middle-aged men, and these results agreed with previous research.[40]
The most frequently involved levels are L3–L4 (32%) and L4–L5 (35%), followed by L2–L3 (15%), L5–S1 (9%), 5 cases L1–L2, 3 cases thoracic spine, 1 case cervical spine.
In 25% of the cases, patients had a history of spine disorders (chronic low back pain, spondylolisthesis, infective spondylitis, previous surgery, and trauma).
Mechanism of dorsal migration: Why not L5–S1 in young patients?
Posterior epidural migration of extruded disc fragments is a rare condition due to the presence of PLL with Trolard’s ligament, peridural or lateral membrane, epidural fat, dural venous plexus, and the nerve root itself.[24] The sagittal midline septum of the PLL joins the space between the vertebral body and PLL. Another membrane, the peridural or lateral membrane, extends from the PLL to the wall of the spinal canal, preventing posterolateral migration. Any failure of these tissues may facilitate the posterior epidural migration of an extruded disc fragment.[15]
When the sequestrated disc fragment is located proximal or distal to the intervertebral foramen, the nerve root is no longer in its position as an anatomical barrier, allowing the free fragments to migrate more easily posteriorly.[39]
This pattern may result from a combination of:
Age-related degeneration: Patients with herniation at L3–L4 and L4–L5 levels are significantly older than patients with L5–S1 herniation; and disc degeneration in elders may be associated with impaired ligaments;
Anatomical factors: The L3–L4 disc is horizontal and the spinal canal is larger, which appears to weaken the nerve root’s protective function at the L3–L4 level;[51]
Load: Biomechanical models have shown that the load on the L3 and L4 vertebrae in both sitting and standing positions with flexion is two and a half times the total body weight.[58]
Previous studies demonstrated a relationship between heavy physical jobs and disc degeneration.
There is an evaluation bias with these patients: The cases that come to medical attention are often those with significant deficits, where MRI and surgery are performed in an emergency setting. As a result, it is often challenging to document natural history.
Radiological features and differential diagnosis
MRI is the diagnostic gold standard, with or without contrast. It was the diagnostic imaging choice in 78% of cases. The herniated disc usually appears similar to the cerebral spinal fluid signal intensity and exhibits ring enhancement on the post-contrast sequences.[26]
The MRI findings of posterior epidural lumbar disc fragments include: on T1-weighted images, a concave indentation of the posterior thecal sac due to a mass surrounded by hyperintense fat tissue; and rim enhancement on gadolinium-enhanced MRI. The first finding is a particularly decisive clue that the lesion is located in the epidural space.[39]
CT scan was the radiological exam in 14% of cases, more accessible in the emergency room. CT scans usually demonstrate a soft tissue nodule indenting and displacing the dural sac anteriorly. In 5 cases CT scan studies required the integration with MRI. Other radiologic imaging used was myelography (4%), a more invasive procedure. In a few cases, further tests were performed such as muscle or sensory– evoked potential. There are several differential diagnoses including abscess,[59] meningioma, tumors, lymphoma, hemangioma, and synovial cyst,[11] especially in Baastrup’s disease because cysts are located between spinous processes and may extend in the epidural space,[60,61] infection and epidural hematoma. Other rarer differential diagnoses are benign tumors: lipomas that are usually asymptomatic,[62] but can become, much more rarely, the cause of neurologic impairment syndrome due to the compression of the neural elements inside the spinal canal, hemangioma, usually symptomless and discovered incidentally, but condition, such as pregnancy, can lead to rapid onset of neurologic symptoms.[63]
Meningiomas, metastasis, tumors, and hemangiomas usually reveal a ring–like peripheral enhancement, which is not specific. In cases of metastases and lymphomas the patients usually present with multisystem involvement and marrow abnormalities. Abscesses are associated with an infectious illness and hematomas with rheumatologic diseases [ankylosing spondylitis and diffuse idiopathic skeletal hyperostosis (DISH)] or trauma in patients with elevated INR.[55]
The differential diagnosis between posterior epidural herniation of a lumbar disc fragment and epidural hematoma can be quite challenging. Disc herniation with migration often maintains contact with the disk space from which the fragment originated, while hematomas typically have less direct contact with the disk space.[37]
Clinical manifestation
Clinical manifestations of posterior epidural migration of herniated disc range from low back pain without neurological deficit to CES. Among the 108 patients included in this review, in 63% of cases, motor function was involved, in 56% there was a sensory loss, in 36% hyporeflexia and in 37% sphincter disorders. Akhaddar et al. reported no correlation between the size of the migrating disk hernia and the degree of neurological deficits.[24]
We found no statistically significant correlations between the level of the herniated disc and the gravity of the clinical manifestations. Obviously, neurological deficits guide surgery timing.
Treatment
Surgery is the most common treatment choice (97% of cases), including hemilaminectomy or laminectomy, facetectomy, and discectomy (24%). One case was treated using an endoscopic approach.[47]
Tarukado et al. reported 3 cases treated with spontaneous regression of posterior epidural herniated disc: Two over 3 cases showed hypoesthesia, 1 over 3 showed a mild reduced strength of one leg, and none of them showed hyporeflexia or sphincter involvement.[30]
Open surgery is considered the best choice because surgeons are often unable to make a definitive diagnosis using radiological findings. Moreover, pathologic confirmation can be performed, and in case of the presence of signs of infection surgeons using a minimally invasive approach can decompress the spinal cord, isolate the pathogen, and evacuate the abscess.[64]
Early surgery should be performed to prevent severe neurological deficits. Previous studies indicate that prognosis is better for patients who receive surgical treatment promptly.[39]
Outcomes
There were 14% incomplete recovery with sequelae, usually with complications related to the urinary system (5 cases). A full recovery was reported in 55% of cases, while 31% experienced improvement without significant deficits. Delayed diagnosis often results in late surgical decompression, increasing the likelihood of sequelae.[39]
Limitations
The rarity of this condition makes it difficult to perform prospective studies which would be helpful to decide the diagnostic algorithm and surgery timing.
CONCLUSION
Posterior epidural migration of herniated discs should be taken into consideration in patients with CES or sudden symptoms of radiculopathy. An accurate examination of MRI should be performed in order to avoid misdiagnosis. Although there are some radiological findings that can help differential diagnosis, open surgery is recommended to perform microbiological and pathological examination.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Medical management of acute non-specific low back pain: Comparison of different medical treatments, one center’s retrospective analysis. J Biol Regul Homeost Agents. 2018;32:121-9.
- [Google Scholar]
- The posterior longitudinal ligament and peridural (epidural) membrane. Clin Anat. 2006;19:487-92.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of an extruded lumbar disc fragment causing cauda equina syndrome. Clinical and magnetic resonance imaging evaluation. Spine (Phila Pa 1976). 1998;23:378-81.
- [CrossRef] [PubMed] [Google Scholar]
- Dorsal epidural intervertebral disk herniation with atypical radiographic findings: Case report and literature review. J Spinal Cord Med. 2010;33:268-71.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural herniation of a lumbar disk fragment at L2-3 that mimicked an epidural hematoma. Korean J Spine. 2017;14:115-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of a sequestrated lumbar disk fragment causing cauda equina syndrome in an old patient: A case report. Clin Med Insights Case Rep. 2016;9:39-41.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of a lumbar disc fragment causing cauda equina syndrome: Case report and review of the relevant literature. Eur Spine J. 2001;10:348-51.
- [CrossRef] [PubMed] [Google Scholar]
- Lumbar spinal block by posterior rotation of anulus fibrosus. Case report. J Neurosurg. 1973;39:642-7.
- [CrossRef] [PubMed] [Google Scholar]
- Cauda equina compression due to posterior epidural migration of extruded lum-bar disk. Neurosurg Rev. 1992;15:311-3.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior thecal lumbar disc herniation mimicking synovial cyst. Neuroradiology. 1995;37:192-4.
- [CrossRef] [PubMed] [Google Scholar]
- A migrated lumbar disc herniation simulating a dumbbell tumor. J Spinal Disord. 1999;12:307-9.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of sequestered lumbar disc fragments. Report of two cases. J Neurosurg. 1999;90:264-6.
- [CrossRef] [PubMed] [Google Scholar]
- Dorsal compression of the epidural cord due to free sequestral lumbar prolapse. Diagnostic problems in magnetic resonance imaging and computed tomography. Arch Orthop Trauma Surg. 2001;121:238-40.
- [CrossRef] [PubMed] [Google Scholar]
- Cauda equina syndrome caused by posterior epidural migration of an extruded lumbar disc fragment. Turk Neurosurg. 2001;11:108-10.
- [Google Scholar]
- Posterior epidural migration of extruded lumbar disc mimicking epidural mass: Case report. Turk Neurosurg. 2003;13:3-4.
- [Google Scholar]
- Cauda equina syndrome seconday to posterior epidural migration of a lumbar disc fragament: A rare phenomenon. Eur J Orthop Surg Traumatol. 2004;14:30-1.
- [CrossRef] [Google Scholar]
- Posterior epidural migration of sequestered lumbar disc fragment causing cauda equina syndrome. Br J Neurosurg. 2005;19:257-9.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of lumbar disk fragments: Report of two cases and review of the literature. Surg Neurol. 2008;70:668-71.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual sequestered disc fragments simulating spinal tumors and other space-occupying lesions. Clinical article. J Neurosurg Spine. 2009;11:42-8.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural mass: Can a posteriorly migrated lumbar disc fragment mimic tumour, haematoma or abscess? Acta Orthop Belg. 2009;75:423-7.
- [Google Scholar]
- A lumbar disc herniation mimicking spinal tumor with intra-and extradural components. Spine J. 2011;11:90-1.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of lumbar disc fragment: Three cases and review of literature. Korean J Spine. 2011;8:66-9.
- [CrossRef] [Google Scholar]
- Posterior epidural migration of a lumbar disc fragment: A series of 6 cases. J Neurosurg Spine. 2011;15:117-28.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of herniated lumbar disc fragment. J Neurosurg Spine. 2011;14:313-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior migration of lumbar disc herniation-imaging dilemma due to contrast contraindication: A case report. Radiol Bras. 2012;45:170-2.
- [CrossRef] [Google Scholar]
- Lumbar disc hernia migrating to the epidural posterior space: A rare entity. Internet J Neurosurg. 2014;10:1-6.
- [Google Scholar]
- Posterior epidural migration of sequestered lumbar disc fragment causing cauda equina syndrome. Coluna Column. 2013;12:78-80.
- [CrossRef] [Google Scholar]
- Posterior epidural migration of an extruded lumbar disc mimicking a facet cyst: A case report. Korean J Spine. 2015;12:12-4.
- [CrossRef] [PubMed] [Google Scholar]
- Spontaneous regression of posterior epidural migrated lumbar disc fragments: Case series. Spine J. 2015;15:57-62.
- [CrossRef] [PubMed] [Google Scholar]
- Two cases of dorsal epidural migration of lumbar disk fragments. Neurosurg Q. 2015;25:131-6.
- [CrossRef] [Google Scholar]
- Posterior epidural migration of a sequestered lumbar intervertebral disc fragment. Turk Neurosurg. 2015;27:85-94.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical presentation of a sequestered posterolateral disc fragment. Cureus. 2016;8:e502.
- [CrossRef] [Google Scholar]
- Postdural disc herniation at L5/S1 level mimicking an extradural spinal tumor. Eur Spine J. 2016;25(Suppl 1):80-3.
- [CrossRef] [PubMed] [Google Scholar]
- An unusual case of dorsally sequestrated disk mimicking tumor with cauda equina syndrome. J Spinal Surg. 2016;3:15.
- [CrossRef] [Google Scholar]
- Dorsal lumbar disc migrations with lateral and ventral epidural extension on axial MRI: A case series and review of the literature. Am J Neuroradiol. 2016;37:2171-7.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of lumbar disc: Will the real “disc” please stand up? Surg Neurol Int. 2017;8:302.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural disc fragment masquerading as spinal tumor: Review of the literature. J Back Musculoskelet Rehabil. 2018;31:685-91.
- [CrossRef] [PubMed] [Google Scholar]
- Discography aids definitive diagnosis of posterior epidural migration of lumbar disc fragments: Case report and literature review. BMC Musculoskelet Disord. 2017;18:151.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of a lumbar disk: An entity not to ignore. Pan Afr Med J. 2018;29:59.
- [CrossRef] [PubMed] [Google Scholar]
- Misdiagnosis of posterior sequestered lumbar disc herniation: Report of three cases and review of the literature. Spinal Cord Ser Cases. 2018;4:61.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of a lumbar disc herniation causing cauda equina syndrome: A case report. Cureus. 2018;10:e2739.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual posterior epidural migration of intervertebral herniated disc: A report of two cases. Malays Orthop J. 2018;12:47-9.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of extruded lumbar disc fragment mimicking epidural mass: A case report. Interdiscip Neurosurg Adv Tech Case Manag. 2018;11:31-3.
- [CrossRef] [Google Scholar]
- Posterior epidural migration of a lumbar intervertebral disc fragment resembling a spinal tumor: A case report. Ann Rehabil Med. 2018;42:621-5.
- [CrossRef] [PubMed] [Google Scholar]
- Full-endoscopic interlaminar discectomy for the treatment of a dorsal migrated thoracic disc herniation: Case report. Medicine (Baltimore). 2019;98:e15541.
- [CrossRef] [PubMed] [Google Scholar]
- A Successful outcome despite delayed intervention for cauda equina syndrome in a young patient with a posterior epidural disc extrusion. Cureus. 2019;11:e4645.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior epidural migration of a lumbar disc herniation. Surg Neurol Int. 2020;11:4.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior and anterior epidural and intradural migration of the sequestered intervertebral disc: Three cases and review of the literature. J Spinal Cord Med. 2022;45:305-10.
- [CrossRef] [PubMed] [Google Scholar]
- Dorsal migration of prolapsed intervertebral disc causing cauda equina syndrome. BMJ Case Rep. 2020;13:e238017.
- [CrossRef] [PubMed] [Google Scholar]
- Missing disc fragment: A rare surgical experience. Asian J Neurosurg. 2020;15:674-7.
- [CrossRef] [PubMed] [Google Scholar]
- Difficulty differentiating between a posterior extradural lumbar tumor versus sequestered disc even with gadolinum-enhanced MRI. Surg Neurol Int. 2021;12:267.
- [CrossRef] [PubMed] [Google Scholar]
- Hyperacute onset of adjacent segment disease with dorsally migrated herniated nucleus pulposus causing cauda equina syndrome: A case report. Br J Neurosurg. 2024;38:1006-9.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior spinal cord injury due to dorsal migrated disc herniation caused by thoracolumbar fusion surgery: A case report. J Orthop Sci. 2024;29:445-8.
- [CrossRef] [PubMed] [Google Scholar]
- A Review of the diagnostic features of posteriorly migrated lumbar discs with reports of two cases. Neurol India. 2022;70:1213-6.
- [CrossRef] [PubMed] [Google Scholar]
- Posterior migration of lumbar disc herniation: A case report. Radiol Case Rep. 2024;19:1097-9.
- [CrossRef] [PubMed] [Google Scholar]
- Biomechanics of intervertebral disk degeneration. Orthop Clin North Am. 2011;42:487-99.
- [CrossRef] [PubMed] [Google Scholar]
- Etiopathogenesis of traumatic spinal epidural hematoma. Neurospine. 2018;15:101-7.
- [CrossRef] [PubMed] [Google Scholar]
- The form and structure of the extruded disc. Spine (Phila Pa 1976). 1992;17:1457-61.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology, diagnosis and management of Baastrup's diseases: A systematic review. J Neurosurg Sci. 2022;66:519-25.
- [CrossRef] [PubMed] [Google Scholar]
- Thoracic spine fracture associated with an extradural lipoma: Case report and systematic review of the literature. Orthop Rev (Pavia). 2020;12:8684.
- [CrossRef] [PubMed] [Google Scholar]
- Symptomatic vertebral hemangioma during pregnancy period: A case series and systematic literature review. Orthop Rev (Pavia). 2020;12:8685.
- [CrossRef] [PubMed] [Google Scholar]
- Extensive spinal epidural abscesses resolved with minimally invasive surgery: Two case reports and review of the recent literature. Acta Neurochir Suppl. 2019;125:345-53.
- [CrossRef] [PubMed] [Google Scholar]






