Translate this page into:
Partially thrombosed distal orbitofrontal artery aneurysm mimicking an A1 segment aneurysm
Address for correspondence: Dr. Dhananjaya Ishwar Bhat, Department of Neurosurgery, National Institute of Mental Health and Neurosciences, Bangalore - 560 029, Karnataka, India. E-mail: dibhat@rediffmail.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
Distal orbitofrontal arteries (OFAs) are very rare.[1] The location of these aneurysms can be identified with digital subtraction angiography. However, when it is partially thrombosed the filling portion of the aneurysm may partially overlap on a larger vessel wrongly implicating the vessel as the site of origin. A 63-year-old lady presented with history of sudden onset severe headache. She was not a hypertensive and had no significant past medical or surgical history. CT scan revealed blood in the anterior interhemispheric fissure. Digital subtraction angiography (DSA) revealed a small aneurysm apparently arising from the left A1 segment, proximal to the AcomA region. The aneurysm was seen only in oblique views [Figure 1a and b]. There were no branching vessels at the origin. She underwent a left pterional craniotomy and exploration. At surgery there was no aneurysm along the A1 segment, however buried in the gyrus rectus was a partially thrombosed aneurysm [Figure 2a and b]. On further dissection the left OFA origin on A2 was identified. It was dissected distally and was found to enter into the aneurysm. The distal portion of the OFA emerged from the aneurysm. The recurrent artery of Heubner (RAH) which arose just distal to the anterior communicating artery (Acom) junction was identified separately from the aneurysm. Excision of the aneurysm along with the vessel was done. Post operatively the patient recovered well with no neurologic deficits. CT head on the following day showed no significant infarctions. Histopathological examination of the aneurysm was suggestive of thrombosed wall of aneurysm with no evidence of inflammation or infection.
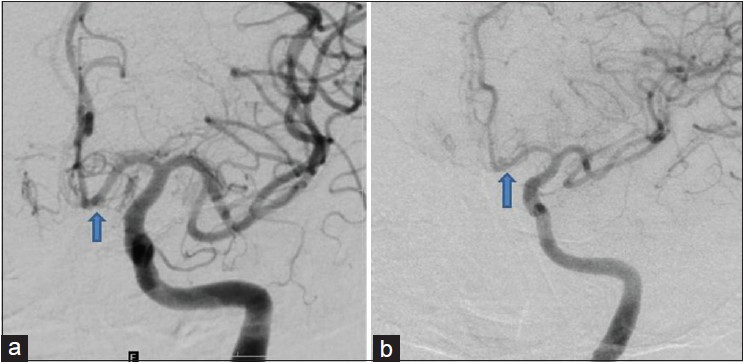
- Digital subtraction angiography left internal carotid artery injection. (a) AP view: No definite aneurysm except for a double density shadow in distal A1 (arrow). (b) Oblique view which shows an aneurysm arising from the distal A1 (arrow)
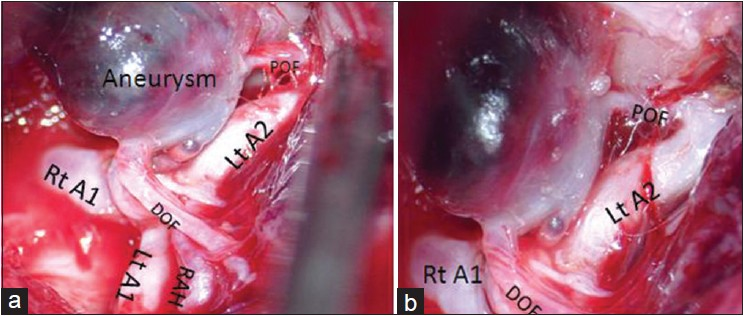
- (a) Intraoperative picture. (b) Magnified view: Showing a partially thrombosed aneurysm arising from the orbitofrontal artery distal to its origin. DOF = Distal orbitofrontal artery, POF = Proximal orbitofrontal artery, RAH = Recurrent artery of Heubner, Rt = Right, Lt = Left
OFA aneurysms are rare and have been reported along with associated vascular malformations and multiple aneurysms.[1] We report an isolated case of a partially thrombosed distal OFA aneurysm in a patient with no predisposing factors. As it was partially thrombosed and was arising from a small vessel, preoperatively it was mistakenly thought that it was arising from the A1 segment. However, only at surgery was the exact nature of the aneurysm defined. It is important to distinguish RAH from the OFA. The RAH usually originates within 4 mm of Acom region (most commonly in the proximal 0.5 mm of A2). Usually it is single but rarely can be duplicated or absent.[2] The OFA arises from the A2 about 5 mm from the AcomA junction. It then courses across the gyrus rectus and olfactory tract supplying the orbital gyri, gyrus rectus and the olfactory tract and bulb. Hence, before sacrificing a vessel the above distinguishing points must be kept in mind, it is important to dissect the vessel distally to confirm that it is not RAH prior to sacrifice.
We report a rare case of partially thrombosed OFA aneurysm arising distal to the origin of the vessel in a patient who had no predisposing factors. Such a case has not been described before. Partially thrombosed aneurysms may give a misleading picture of its origin. It is important to distinguish the OFA from RAH prior to sacrifice of the vessel.
References
- Multiple aneurysms of distal anterior cerebral artery associated with a cerebral arteriovenous malformation. NeurolIndia. 2010;58:968-70.
- [Google Scholar]
- Microsurgicalanatomy of the anteriorcerebral-anterior communicating-recurrent artery complex. J Neurosurg. 1976;45:259-72.
- [Google Scholar]





