Translate this page into:
Paradoxical response in spinal tuberculosis: Lessons learnt
Address for correspondence: Dr. Alugolu Rajesh, Department of Neurosurgery, Nizam's Institute of Medical Sciences, Punjagutta, Hyderabad - 500 082, Telangana, India. E-mail: drarajesh1306@gmail.com
This is an open access article distributed under the terms of the Creative Commons Attribution NonCommercial ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Patients with spinal tuberculosis started on antituberculous treatment (ATT) empirically and showing increasing size of the lesion on follow-up are a treatment challenge. We describe our experience in managing such cases.
Materials and Methods:
We treated 80 patients with spinal tuberculosis at our institute from January 2012 to June 2014. Of these, 50 were managed by surgical intervention and the rest 30 were managed conservatively only on anti-tubercular drugs. Six patients out of these 30 patients, showed a paradoxical increase in the size of lesion without any neurological deficits after 3 months of starting ATT. Surgical intervention was done in three cases, whereas other three were managed by ultrasound-guided tapping of the lesion with continuation of ATT.
Results:
There was an improvement in the symptoms with weight gain and normalcy of appetite. However, all these patients had lymphopenia on differential leukocyte counts at the outset which normalized at 3 months.
Conclusion:
The mainstay of management of paradoxical response in spinal tuberculosis should be conservative with drainage or aspiration of abscesses along with the continuation of ATT. Surgical decompression and stabilization may be necessary in few cases who develop new neurological deficits or deformity or instability.
Keywords
Paradoxical response
spinal
tuberculosis
Introduction
Spinal tuberculosis is endemic in India and is largely diagnosed with noninvasive methods and treated empirically with anti-tubercular drugs as therapeutic diagnosis. Though this is not the ideal protocol, in a resource-limited setup, it is the most commonly followed protocol. Magnetic resonance imaging (MRI) protocols with scoring systems have been devised for objectivating the diagnosis of spinal tuberculosis. We devised one such criterion and are working on its validity presently.[1] The problem started when the response to the empirical treatment was unexpected. The best solution in the situation was to have an histopathological/culture proof that our diagnosis was indeed true. However, working with limited resources, you are pushed to the wall.
What are the possibilities and what can be done in such a situation? The possibilities are wrong diagnosis, unresponsive organisms (multidrug/extremely resistant), noncompliant patient, and many more.
In this article, we are highlighting such an issue and its response with special reference to paradoxical responses in spinal tuberculosis.
Materials and Methods
We had treated 80 patients of spinal tuberculosis from January 2012 to June 2014. We analyzed the prospectively collected data retrospectively and found this interesting phenomenon. Of these, 50 patients were treated by surgical debridement and fixation as they presented with neurological deficits. The rest 30 were started on anti-tubercular drugs following diagnosis using MRI criteria.[1] We started them on four drugs (isoniazid, rifampicin, pyrazinamide, and ethambutol in accordance with body weight).
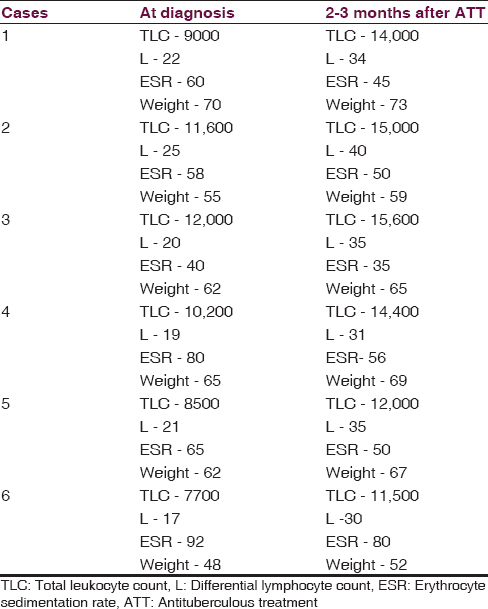
Among these 30 patients, on the first follow-up at 3 months, six patients complained of painless swelling in the paraspinal region. There were no neurological deficits in these patients and they had improved appetite with weight gain [Table 1]. As they presented with new onset fullness over the back, an MRI was done which revealed an increase in size of the spinal lesion with epidural/paraspinal collections in all the patients [Figures 1–3]. Their body weights increased and their erythrocyte sedimentation rate showed a decreasing trend. One peculiar observation that we noticed in retrospect was though they had normal total leukocyte counts, the differential counts had low lymphocytic counts at the outset, which increased at 3 months follow-up.

- Serial images of patient 1 (a) sagittal and axial magnetic resonance images before starting antituberculous treatment (b) sagittal and axial magnetic resonance images showing paradoxical increase 3 months after starting antituberculous treatment (c) sagittal and axial magnetic resonance images showing resolution of lesion at completion of antituberculous treatment

- Serial images of patient 3 (a) sagittal and axial magnetic resonance images before starting antituberculous treatment (b) sagittal and axial magnetic resonance images showing paradoxical increase 3 months after starting antituberculous treatment (c) sagittal and axial magnetic resonance images showing resolution of lesion at completion of antituberculous treatment

- Serial images of patient 6 (a) sagittal and axial magnetic resonance images before starting antituberculous treatment (b) sagittal and axial magnetic resonance images showing paradoxical increase 3 months after starting antituberculous treatment (c) sagittal and axial magnetic resonance images showing resolution of lesion at completion of antituberculous treatment
The possible causes thought were (1) wrong diagnosis, (2) resistant organism, and (3) noncompliance to the treatment. After ascertaining the compliance, we proceeded for the other two. At this stage, even if we were dealing with resistant organisms, we could not change the anti-tubercular drugs to second line in the absence of culture and resistant pattern. And, hence, surgical debridement and stabilization were offered for obtaining tissue for analysis at the same time stabilizing the spine, prophylactically. Hence, all of them were offered surgical debridement, and spinal stabilization in view of the unexpected course of disease.
Three of them refused surgical intervention of any kind and were managed by ultrasound-guided aspiration of the swelling, cultures, and histopathological examination while continuing on the first-line antituberculous treatment (ATT). In the other three, posterior decompression with debridement and spinal fixation was performed, and the debrided material was sent for cultures and histopathological examination was performed. All the surgically intervened patients had nonhealing wounds with discharge of purulent material, necessitating implant removal in all the three. Following implant removal, they were advised bed rest for 3 months while continuing ATT.
HPE was suggestive of granulomatous infection in all the six patients. Tuberculosis cultures were negative in all the patients. ATT was continued in all these patients for a total duration of 18 months.
Discussion
Paradoxical response is seen in 6–30% of patients receiving antituberculosis therapy.[2] It is more commonly described in HIV-positive patients with reported incidence of 11–36% in patients receiving highly active antiretroviral therapy (HAART).[34] All the patients described in our series are HIV-negative with an incidence 7.5%. The delay between the introduction of the ATT and the appearance of these lesions ranged from 1 to 3 months.[5] Paradoxical manifestations may occur in the site of primary diagnosis as in our series or in a new uninvolved site. Paradoxical response is seen more commonly in patients with extrapulmonary tuberculosis with central nervous system being the most common site (50%) followed by respiratory system (25%) and lymph nodes.[6] A high propensity for spinal and paraspinal involvement was observed by few.[6]
The pathophysiology of paradoxical response in HIV-positive patients is the phenomenon of “immune restitution” after starting HAART.[7] In HIV-negative patients, paradoxical response occurs because of ATT-induced disinhibition of the cell mediated immunity that normally accompanies the tubercular infections. After starting ATT, there is restoration of a specific immunity, combined with the release of mycobacterial debris during the lysis of the pathogenic agent, which explains the paradoxical reaction.
All our 6 patients, though had normal/elevated leukocyte counts had low lymphocytes on differential counts at the outset which improved at 3 months follow-up [Table 1]. This was also seen in earlier studies.[6] All the patients, however, had improvement in constitutional symptoms, appetite, and weight. Moreover, despite progression of the size of the lesion, there were no neurological deficits. All of them completed 18 months of treatment and had hematological and radiological improvement at completion. The diagnosis of paradoxical response can be made only after exclusion of other reasons for deterioration. High clinical suspicion in case of new onset symptoms and signs, monitoring clinical and radiological response to ATT, monitoring lymphocyte counts before and after starting ATT aids in the diagnosis.
The probable risk factors for paradoxical response are extrapulmonary tuberculosis with or without pulmonary involvement, low baseline lymphocyte counts, and an upsurge in lymphocyte counts during paradoxical deterioration.[6]
Conclusion
Paradoxical response in spinal tuberculosis, though is a diagnosis of exclusion, has to be kept in mind in spinal tuberculosis diagnosed by noninvasive means. The mainstay of management of paradoxical response in spinal tuberculosis should be conservative with drainage or aspiration of abscesses along with the continuation of ATT reserving surgical intervention for those developing neurological deficits/spinal deformities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Novel magnetic resonance imaging scoring system for diagnosis of spinal tuberculosis: A preliminary report. J Neurosci Rural Pract. 2013;4:122-8.
- [Google Scholar]
- Clinical spectrum of paradoxical deterioration during antituberculosis therapy in non-HIV-infected patients. Eur J Clin Microbiol Infect Dis. 2002;21:803-9.
- [Google Scholar]
- Paradoxical worsening of tuberculosis following antiretroviral therapy in patients with AIDS. Am J Respir Crit Care Med. 1998;158:157-61.
- [Google Scholar]
- Paradoxical worsening of tuberculosis in HIV-infected persons. Chest. 2001;120:193-7.
- [Google Scholar]
- Immunorestitution diseases in patients not infected with HIV. Eur J Clin Microbiol Infect Dis. 2001;20:402-6.
- [Google Scholar]
- Risk factors for development of paradoxical response during antituberculosis therapy in HIV-negative patients. Eur J Clin Microbiol Infect Dis. 2003;22:597-602.
- [Google Scholar]
- Immunorestitution disease involving the innate and adaptive response. Clin Infect Dis. 2000;30:882-92.
- [Google Scholar]






