Translate this page into:
Ossified Occipital Pseudomeningocele following Ventriculoperitoneal Shunt Malfunction
Bevinahalli N. Nandeesh, MD Department of Neuropathology, National Institute of Mental Health and Neurosciences Hosur Road, Bengaluru 560029, Karnataka India nandeeshbn@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Ossification of pseudomeningocele is a rare occurrence and is one of the rare complications of ventriculoperitoneal (VP) shunt malfunction. We report a case of 12-year-old boy who came with features of raised intracranial pressure following shunt malfunction which was placed as a treatment to the aqueductal stenosis. Computed tomography showed ventriculomegaly and hypodense collection in the occiput with posterior rim of calcification. The findings were confirmed on histopathology. Although ossified pseudomeningocele is a rare entity following VP shunt placement, it should be suspected if patients present with aggravated symptoms, especially if there is shunt malfunction as the treatment option varies with the presence or absence of resultant symptoms and ossification.
Keywords
ossified pseudomeningocele
shunt malfunction
ventriculoperitoneal shunt
Introduction
Pseudomeningocele, as described by Harvey Cushing, is an extradural collection of cerebrospinal fluid (CSF) that communicates with subarachnoid space.1 Ossification of pseudomeningocele is very rare. We present a case of ossified pseudomeningocele in the occiput following ventriculoperitoneal (VP) shunt malfunction.
Case Report
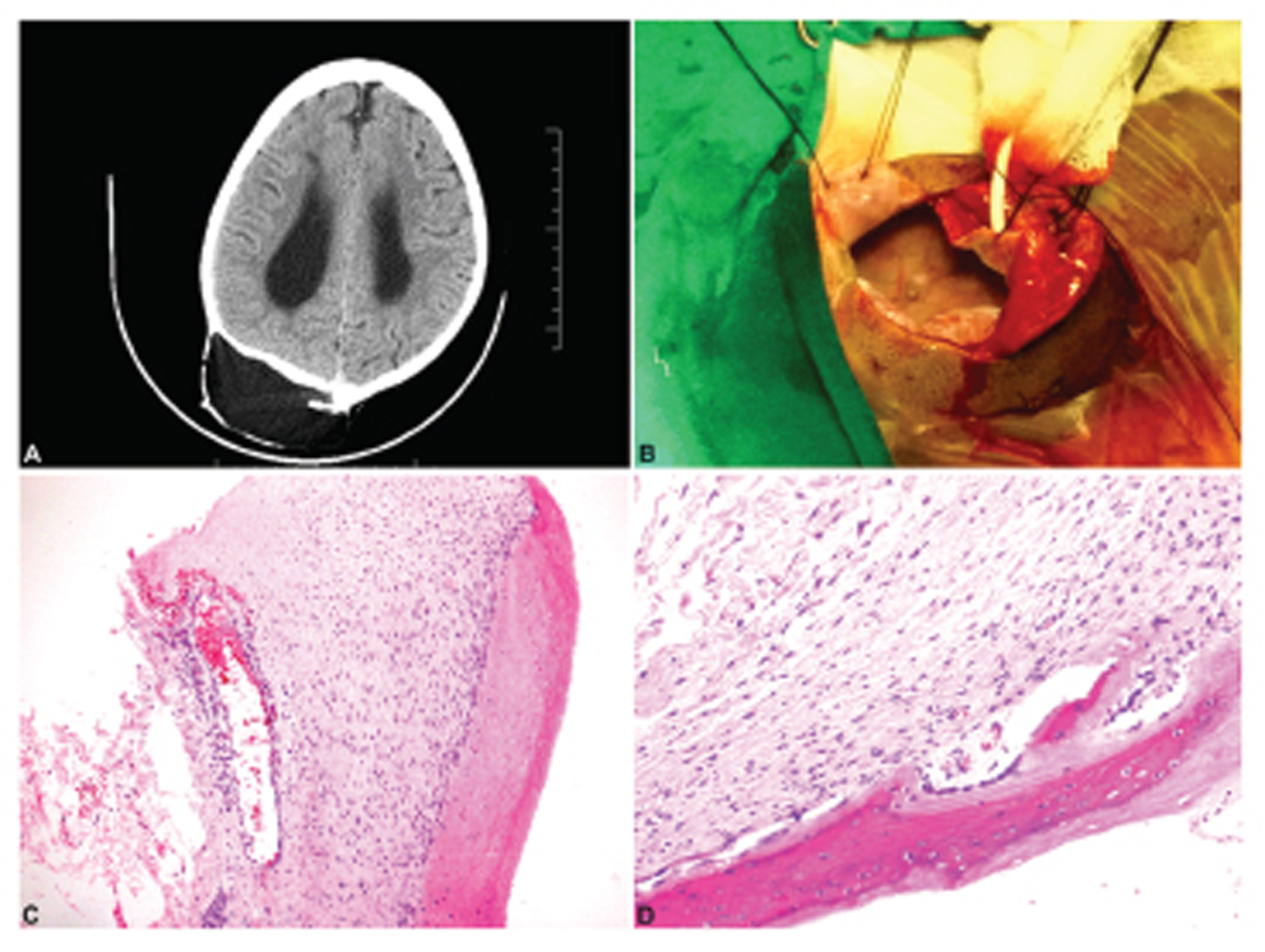
A 12-year-old boy, a known case of aqueductal stenosis with hydrocephalus, had undergone right Frazier's shunt for the same in 2004 followed by endoscopic third ventriculostomy in 2011 for shunt malfunction. The child was doing well for the next 6 years; but in 2017, he again presented with symptoms of raised intracranial pressure. Computed tomography scan revealed supratentorial ventriculomegaly with hypodense collection in the right occiput, with a thin rim of calcification posteriorly ( Fig. 1A ). The child underwent revision of the right Frazier's VP shunt with excision of the ossified pseudomeningocele ( Fig. 1B ).
On histopathology, fragments of fibrocollagenous tissue composed of dense collagen with a variable degree of hyalinization were noted. On the inner aspect of the membranes, there were congested vessels, proliferating vessels, and fibroblastic proliferation. Foci of ossification were noted on the inner aspect ( Fig. 1C, D ). The membrane was lined by arachnoidal cells which appeared indistinct to flatten.
-
Fig. 1 (A) Computed tomography axial image showing a large right parietal pseudomeningocele with ossification in the periphery, (B) preoperative image of the pseudomeningocele, (C and D) H&E sections showing fibroplastic proliferation on inner aspect with ossification with osteoblastic lining on the external aspect (×4, ×10). H&E, hematoxylin and eosin.
Fig. 1 (A) Computed tomography axial image showing a large right parietal pseudomeningocele with ossification in the periphery, (B) preoperative image of the pseudomeningocele, (C and D) H&E sections showing fibroplastic proliferation on inner aspect with ossification with osteoblastic lining on the external aspect (×4, ×10). H&E, hematoxylin and eosin.
Discussion
Pseudomeningocele refers to CSF collections in cavities within the soft tissues or localized in calvarial bone diploe.2 Pseudomenigocele can be congenital (nontraumatic) or traumatic.3 4 The traumatic cause can be blunt trauma, inadvertent trauma to the dura, planned dural opening (surgery/ iatrogenic), infection, or intramural hemorrhage.3 4 5 6 Following dural tear, if the arachnoid remains intact, a meningocele is then formed. Pseudomeningocele is formed when there is an arachnoid breach following the dural tear.4
Theories as to why pseudomeningoceles are formed include the following: one school of thought is that the pseudomeningocele results from one-way flow of CSF from the normal CSF space to the extradural space,4 6 whereas another theory for the formation of intradiploic pseudomeningocele states that the diploe plays an important role in the absorption of CSF into the venous system.7 8 9 When this fails, there occurs accumulation of CSF within the diploe, leading to widening of outer and inner tables due to the water-hammer effect of CSF accumulations.2 In the present case, the pseudomeningocele is probably a result of shunt malfunction followed by increased CSF pressure, leading to accumulate CSF in the extradural space.
Ossification of pseudomeningocele was first described by Verbiest in 195111, while describing unusual forms of cauda equina compression.10 One of the main factors considered for calcification/ossification is the length of time.4 It is proposed that there occurs metaplasia of the surrounding soft tissue to cartilage which later ossifies.4 10 This is supported by the histological presence of fibroblasts, cartilage, and ossified bone.10 The process is said to be fastened by the presence of blood which in turn initiates inflammation.10 Ossification is noted on the posterior wall, at the boundary of CSF and posterior soft tissue. In the present case, rim of calcification was noted on imaging, and further ossification was proved on histology. This requires a histopathologist to be aware of this entity to accurately diagnose it microscopically.
The treatment varies depending on the location and symptomatology, ranging from surgical treatment to observation. Symptomatic cases require surgical intervention. The presence of ossification requires its surgical excision with or without focal reconstruction. The selection of the new-entry point in the cranium is also dictated by the complexity of the pseudomeningocele with ossification. In the current case, the same-entry point was used for shunt insertion. However, in contrast, the cases with a lack of ossification may be managed with routine CSF diversion alone. The present case underwent surgical excision of the ossified pseudomeningocele sac and shunt revision.
Conclusion
It is important to be aware of this very rare complication of VP shunt malfunction for the better management in the form of excision, shunt revision with or without reconstruction. The imaging may help in the identification of calcification and ossification. This can be further proven on histopathology by the presence of the ossified bone and cartilage.
Conflict of Interest
None declared.
Funding None.
References
- Experiences with cerebellar medulloblastomas: a critical review. Acta Pathol Microbiol Immunol Scand. 1930;7:1-86.
- [Google Scholar]
- Intradiploic pseudomeningocele and ossified occipitocervical pseudomeningocele after decompressive surgery for Chiari I malformation: report of two cases and literature review. Neurosurg Rev. 2017;40(2):345-350.
- [Google Scholar]
- Spinal extradural cysts: with report of an ossified spinal extradural cyst. Am J Roentgenol Radium Ther Nucl Med. 1963;90:1227-1230.
- [Google Scholar]
- Calcified pseudomeningocele of the lumbar spine: a review. Eur Spine J. 2013;22(03):S443-S449.
- [Google Scholar]
- Postsurgical calcified pseudocyst of the lumbar spine. J Comput Assist Tomogr. 1982;6(3):627-629.
- [Google Scholar]
- Postsurgical meningeal pseudocysts of the lumbar spine. Clin Orthop Relat Res. 1971;75(75):167-178.
- [Google Scholar]
- Access to cerebrospinal fluid absorption sites by infusion into vascular channels of the skull diplö. J Neurosurg. 2007;107(4):841-843.
- [Google Scholar]
- Intraosseous infusion into the skull: potential application for the management of hydrocephalus. J Neurosurg. 2007;106(2):120-125.
- [Google Scholar]
- Cerebrospinal fluid drainage through the diploic and spinal epidural veins. J Anat. 2015;227(3):297-301.
- [Google Scholar]
- Ossified pseudomeningocele following Chiari decompression surgery in a patient with Kleeblattschadel deformity. J Neurosurg Pediatr. 2008;2(3):203-206.
- [Google Scholar]
- Unusual forms of compression of the cauda equina. 1951. Report of two cases of lumbo-sacral extradural cysts and of one case of ‘knotting’ of a caudal nerve root. Paper presented at the meeting of the Luso-Spanish Society and the British Society of Neurological Surgeons
- [Google Scholar]






