Translate this page into:
Obsessive-Compulsive Inventory-Revised: Factor Structure, Reliability, Validity, and Suicide Risk Screening Characteristics among Nigerian Patients with Schizophrenia
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Objective:
This study attempted to explore the feasibility of use of the 18-item Obsessive-Compulsive Inventory-Revised (OCI-R) as a subjective suicide risk assessment tool in a cross-sectional sample of Nigerian patients with schizophrenia.
Materials and Methods:
Two hundred and thirty-two outpatients with schizophrenia were recruited from the mental health clinic of a university teaching hospital in Southwestern Nigeria. They completed the OCI-R in addition to the Social and Occupational Functioning Assessment Scale, the Positive and Negative Syndrome Scale, and a sociodemographic and illness-related questionnaire. The patients were objectively interviewed with the Mini-International Neuropsychiatric Interview suicidality module items to assess their suicide risk.
Results:
The 18-item OCI-R demonstrated satisfactory sensitivity (0.900) and specificity (0.662) at a total cutoff score of 10 in relation to the identification of Nigerian patients with schizophrenia with significant suicide risk. At this cutoff score, the area under the receiver operating characteristic curve was 0.817 (95% confidence interval: 0.735–0.898), and positive predictive value (0.726) and negative predictive value (0.869) were also satisfactory. The OCI-R also demonstrated satisfactory internal consistency and construct validity.
Conclusion:
The OCI-R has demonstrated to be useful as a subjective suicide risk assessment tool among Nigerian schizophrenia patients.
Keywords
Nigerian schizophrenia patients
Obsessive-Compulsive Inventory-Revised
sensitivity
specificity
suicidality
INTRODUCTION
Schizophrenia is a disabling mental disorder that affects 4.6/1000 of the population at some point in their lifetime.[1] In this affected population, mortality is not an uncommon event.[2] The report of a meta-analysis indicates that 4.9% of patients with schizophrenia will commit suicide during their lifetime.[3] The risk factors for suicide in these patients are similar to those in the general population and they include young age, male gender, higher level of education, recent loss, previous suicide attempts, and drug use.[45] In addition to these risk factors, obsessive-compulsive symptoms (OCS) have also been found to complicate suicidal behaviors among patients with schizophrenia.[678] The prevalence of obsessive-compulsive phenomena in schizophrenia ranges from 3% to 64% in both epidemiological and clinical studies across different countries.[89] Few studies have been done in Africa. The prevalence of OCS among patients with schizophrenia was reported as 2.5% in a study conducted in South Africa.[10] OCS correlate with more suicide attempts, greater disability, and deficits in social functioning.[678] Sevincok et al. reported that OCS may account for the emergence of suicidality in patients with schizophrenia, and these symptoms are also significant predictors of suicide.[2] They also reported that schizophrenia patients with OCS had a previous history of greater number of suicide attempts and suicidal ideations. In addition, it was reported in a systematic review that the presence of OCS in schizophrenia is associated with higher global, positive, and negative symptoms of psychosis.[11] However, it should be noted that there is no study in Nigeria that has used a psychometrically validated scale to assess OCS among patients with schizophrenia.
The Obsessive-Compulsive Inventory-Revised (OCI-R) is one of the instruments that have been utilized to assess the severity of OCS across different cultures.[12131415] It is preferred to the other lengthier 42-item version because of its brevity and good psychometric properties.[12131415] In this study, we attempted to examine how the 18-item OCI-R can be adapted as a subjective suicide risk assessment instrument among Nigerian patients with schizophrenia. Although the OCI-R was primarily designed to quantify the severity of OCS, we are of the opinion that due to the inadequate number of trained personnel to objectively evaluate suicide risk applying the structured interview techniques such as the Mini-International Neuropsychiatric Interview (MINI), a self-reported scale with adequate sensitivity and specificity for the indirect identification of high suicidal risk Nigerian patients with schizophrenia will be advantageous.[16] This study attempted to explore the feasibility of use of the 18-item OCI-R as a subjective suicide risk assessment tool in a cross-sectional sample of Nigerian patients with schizophrenia. We also examined the basic psychometric characteristics of OCI-R in terms of its reliability, validity, and factor structure.
MATERIALS AND METHODS
Sample
This is a cross-sectional descriptive study and the participants were outpatients receiving treatments for schizophrenia at the mental health clinic of the Department of Psychiatry, Ladoke Akintola University of Technology Teaching Hospital, Osogbo, in Southwestern Nigeria. The participants were consecutively recruited over a period of 6 months from the outpatient clinic. In order to be eligible for the study, the participants must be 18 years old and above and are on treatment for schizophrenia, a diagnosis which had been made based on International Classification of Diseases-10 (ICD-10). Those participants who had evidence of organic disorder or any significant comorbid physical illness that could prevent the individuals from participating in the study were excluded from the study. Furthermore, those who were psychopathologically too disturbed to the extent that they could not respond to questions and were not able to complete the self-administered questionnaires were excluded from the study. In addition, those who had family history of mood or anxiety disorder were also excluded from the study. The ethical approval for the study was obtained from the research ethics committee of the study center. A total number of three researchers were involved with the recruitment of outpatients during the study. On each clinic day, after the purpose of the study has been explained to the outpatients and informed consent obtained, they were ushered into a consulting room for privacy, following which the study measures were administered. During the period of recruitment, 17 outpatients refused to give consent. A total of 232 outpatients participated in this study.
Assessment
The study participants completed a research inventory which consists of a sociodemographic and illness-related questionnaire as well as the OCI-R version. The psychotic module of the MINI was used to confirm the diagnosis of schizophrenia among the outpatients while the suicidality module section was employed to evaluate the suicidal risk among them.[16] The level of psychopathology was assessed using the Positive and Negative Syndrome Scale (PANSS) while their functioning was assessed with the Social and Occupational Functioning Assessment Scale (SOFAS).[1718]
Sociodemographic and illness-related questionnaire
This was a specially designed pro forma to collect information from each participant. The variables included were age, gender, number of years of education, age at onset of active symptoms of schizophrenia, duration of treatment, and number of medications. The information obtained from the patients or caregivers was supplemented with information from the medical records of the patients.
Obsessive-Compulsive Inventory-Revised
This is a shorter version of the 42-item Obsessive-Compulsive Inventory developed by Foa et al. in 1998.[12] It is a self-report scale for assessing symptoms of obsessive-compulsive disorder. It consists of 18 questions rated on a 5-point Likert scale. Total scores are generated by adding the item scores. The possible range of scores is 0–72 with higher scores indicating greater OCS severity.[12]
Mini-International Neuropsychiatric Interview
The MINI is designed as a brief structured interview for the major Axis I psychiatric diagnoses in the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition and ICD-10.[16] The lifetime diagnosis version was used in this study to confirm the diagnosis of schizophrenia. The suicidality module of this instrument which is grouped as “C module” was used to assess suicidality in the participants. There are nine questions in this module labeled C1 to C9. Questions C1 to C8 assess suicidality-related events in the previous 1 month while question C9 assesses for lifetime suicide attempt. This module was objectively used to assess suicidality which included suicidal intent, plan, and attempt. Cumulative scores were graded either as low risk (1–8 points), moderate risk (9–16 points), or high risk (17 points and above).[16] Those patients with cumulative scores of 17 and above on the MINI suicidality module were categorized as “positive for high suicide risk,” while the other patients with scores below 17 were grouped as “negative for high suicide risk.”
Positive and Negative Syndrome Scale
Psychopathological symptoms were assessed with the PANSS which included a structured interview to assess patients on 30 items covering positive (7 items), negative (7 items), and general symptoms of psychosis (16 items).[17] Each item on the three subscales was rated on a 7-point Likert scale.
Social and Occupational Functioning Assessment Scale
The SOFAS was used to assess the social and occupational functioning of the patients. This scale differs from the Global Assessment of Functioning scale in that it focuses exclusively on the individual's level of social and occupational functioning and is not directly influenced by the overall severity of the individual's psychological symptoms.[18]
Statistical analysis
The Statistical Product and Service Solutions (SPSS) software (IBM Corp, Armonk, New York, USA), 21st version, was used for statistical analysis. Descriptive statistics such as the mean (standard deviation [SD]) and frequency (percentages) were utilized in depicting the patients’ sociodemographic and illness variables and scores on the study measures. The construct validity of the OCI-R was examined through correlational analyses with the MINI suicidality module, SOFAS score, and PANSS subscales scores. The reliability of the OCI-R was determined by calculating the Cronbach's alpha and the items of total scale correlations. The factor loading of the scale's items was examined by applying principal axis factoring (PAF) with oblimin rotation since we expected the factor extracted to correlate.
Receiver operating characteristic (ROC) curve analysis was conducted to examine the screening qualities of the OCI-R in relation to the identification of schizophrenia patients with significant suicidal risk, and the total cutoff score was delineated by the Youden's index, which is the optimal trade-off point between the sensitivity and specificity.[19] The other parameters that were calculated to evaluate the effectiveness of the OCI-R as a screening tool for high suicide risk schizophrenia patients include sensitivity, specificity, accuracy, positive predictive value (PPV) and negative predictive value (NPV), and the positive (LR +ve) and negative (LR −ve) likelihood ratios. The area under the ROC curve (AUC) was also measured. The presence of the null value of 0.5 in the 95% confidence interval (CI) of the AUC is indicative of a screening tool with poor discriminative power and an AUC value closer to 1 is indicative of a scale with more satisfactory discriminatory ability.[20] All statistical tests were two-tailed and the level of significance was set at P < 0.05.
RESULTS
Sociodemographic, illness-related, and other measure details (n = 232)
As shown in Table 1, the mean age of the patients was 36.23 (SD 8.83) years. Males constituted 50.4% of the sample. The mean age at onset of symptoms was 31.34 (SD 7.84) years. The mean total score on the OCI-R was 8.91 (SD 12.62). The mean scores on the PANSS positive, PANSS negative, and PANSS general were 8.64 (SD 3.24), 8.81 (SD 3.80), and 17.88 (SD 4.08), respectively. The mean SOFAS score was 69.44 (SD 15.23). According to the MINI suicidality module, 10 (4.3%) of the patients were categorized as moderate/high suicide risk.

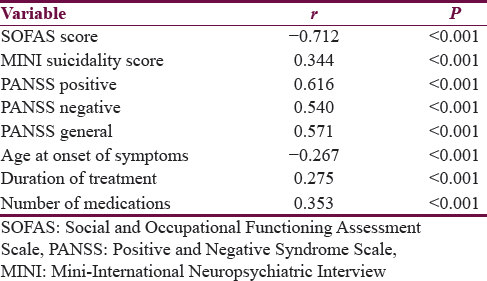
Correlational analyses between the Obsessive-Compulsive Inventory-Revised and other study measures (n = 232)
Table 2 shows that there were statistically significant moderate negative correlation between OCI-R and SOFAS score (r = −0.712, P < 0.001), and weak negative correlation between OCI-R and age at onset of symptoms (r = −0.267, P < 0.001). There were modest positive correlations between OCI-R and PANSS subscale scores; positive (r = 0.616, P < 0.001), negative (r = 0.540, P < 0.001), and general (r = 0.571, P < 0.001). Positive correlations were also observed between OCI-R and MINI suicidality module score (r = 0.344, P < 0.001), duration of treatment (r = 0.275, P < 0.001), and the number of medications (r = 0.353, P < 0.001).
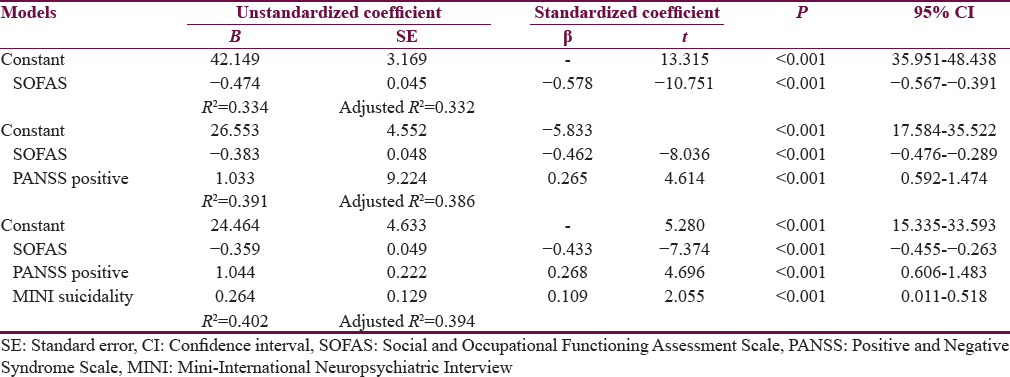
Linear regression model
Table 3 depicts the linear regression model indicating the percentage of the variance taken up at each step as each variable is added into the model. The score on the OCI-R was significantly predicted by the SOFAS score (R2 = 0.334, P ≤ 0.001), PANSS-positive scores (R2 = 0.391, P < 0.001), and the MINI suicidality module score (R2 = 0.402, P = 0.011); these 3 variables accounted for 33%, 39%, and 40% of the variance in the OCI-R score, respectively, with the largest variance contributed by the patients’ functioning (SOFAS).
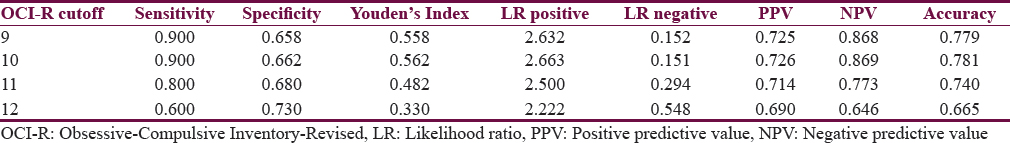
Screening characteristics of the Obsessive -Compulsive Inventory-Revised at different cutoff scores among the patients (n = 232)
Table 4 indicates that after subjecting the OCI-R scores to a ROC curve analysis, it was observed that the scale demonstrated a modestly excellent performance against the schizophrenia patients’ MINI suicidality module categorization. The OCI-R as an adapted suicide risk screening tool demonstrated satisfactory psychometric properties with the maximum Youden's index at a cutoff total score of 10 which was associated with the highest sensitivity (0.900) and specificity (0.662) among our patients. Figure 1 showed that the ROC curve at this cutoff score has an AUC of 0.817 (95% CI = 0.735–0.898).

- The ROC curve of the OCI-R at a cut-off score of 10 against the patients’ suicide risk categorization according to the MINI (AUC = 0.817; 95% Confidence Interval = 0.735-0.898; Std. Error = 0.042)
Descriptive characteristics, internal consistency, and factor loadings of the Obsessive-Compulsive Inventory-Revised items
As shown in Table 5, PAF analysis with oblimin rotation yielded 2 factors. The adequacy of our sample for factor analysis is reflected by a Kaiser-Meyer-Olkins measure of sampling adequacy of 0.914. The overall Cronbach's alpha was 0.939. All the items in the OCI-R correlated fairly well and none of the correlation coefficients was particularly large; we, therefore, had no reason to eliminate any of the scale's items. Item 4 had the highest loading (0.851). The corrected item total correlations for the factor 1 items ranged from 0.495 to 0.783, while those of factor 2 ranged from 0.503 to 0.599.

DISCUSSION
The aim of this study was to explore the applicability of the OCI-R as a screening instrument for the identification of Nigerian schizophrenia patients with a significant suicidal risk. We examined the ability of the inventory to distinguish between schizophrenia patients categorized as low suicide risk and those categorized as moderate/high suicide risk according to the MINI suicidality module section.[16] We plotted a ROC curve to explore the best aggregate cutoff score that would optimize the sensitivity and the specificity of the inventory in relation to the identification of high suicidal risk among the Nigerian schizophrenia patients. Additional psychometric characteristics of the OCI-R that we examined included the internal consistency, factorial loading, and construct validity. This study has shown preliminary evidence that in a clinical sample of Nigerian schizophrenia patients, the OCI-R to a significant extent has satisfactory psychometric properties as a suicidal behavior-related assessment tool. The full scale had a satisfactory internal consistency which is comparable to the finding of the original developers of the OCI-R and other authors.[1221] The relationships between the OCI-R and the other study measures were all toward the expected directions. Patients with higher scores on the OCI-R are expected to have lower scores on the SOFAS and higher scores on the MINI suicidality and the PANSS subscale scores. In our study, patients with higher scores on OCI-R had significantly more psychopathological disturbances and lower social functioning. These findings are in harmony with what have been previously reported in other studies.[611] As shown by the highest Youden's index, an OCI-R cutoff total score of 10 had the most optimal trade-off points between the sensitivity and specificity for the patients with significant suicidal risk. At a cutoff point of 10, the questionnaire could identify 90% of the significantly suicidal risk schizophrenia patients and 66.2% of those not having such risk. Furthermore, this cutoff score was associated with the maximum PPV (72.6% of patients belonging to the significant suicidal risk group who truly had a significant risk for suicidality) and NPV (86.9% of patients recognized as not belonging to the significant suicidal risk group who truly are not highly suicidal). The AUC of 0.817 also supports the discriminatory ability of the OCI-R at this cutoff score.[2021] Furthermore, at this total cutoff score, the value of the likelihood ratio for a positive test (LR +ve) reflects a moderate probability of correctly identifying those schizophrenia patients who have a high risk for suicidal behavior (true positives) while the value of the likelihood ratio for a negative test (LR −ve) indicates a high probability that the schizophrenia patients who do not have a high risk for suicidal behavior (true negatives) will be correctly identified.[22]
Some of the identified limitations include the fact that this study was carried out in the southwestern Nigeria; hence, it may not be appropriate to generalize the findings of this study. Another limitation is that our sample size was relatively small. However, this is the first study in Nigeria and Sub-Sahara Africa to examine not only the basic psychometric properties of OCI-R but also its application as a suicide screening tool among patients with schizophrenia. The use of OCI-R as a suicide screening tool is important, especially in the developing world, where there is scarcity of trained personnel to objectively evaluate suicide risk through the application of structured interview techniques such as the MINI.[16]
CONCLUSION
Patients with schizophrenia who completed this instrument with high scores may require further evaluations. We are of the opinion that this study using the OCI-R as a suicide screener among schizophrenia patients will encourage further studies in Nigeria and in Africa as a whole.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Suicidality in schizophrenic patients with and without obsessive-compulsive disorder. Schizophr Res. 2007;90:198-202.
- [Google Scholar]
- The lifetime risk of suicide in schizophrenia: A reexamination. Arch Gen Psychiatry. 2005;62:247-53.
- [Google Scholar]
- Suicide and schizophrenia: A systematic review of rates and risk factors. J Psychopharmacol. 2010;24:81-90.
- [Google Scholar]
- Schizophrenia and suicide: Systematic review of risk factors. Br J Psychiatry. 2005;187:9-20.
- [Google Scholar]
- Obsessive-compulsive symptoms in schizophrenia: Associated clinical features, cognitive function and medication status. Schizophr Res. 2005;75:349-62.
- [Google Scholar]
- Obsessive-compulsive symptoms in schizophrenia: Prevalence, correlates and treatment. Expert Rev Neurother. 2009;9:99-107.
- [Google Scholar]
- Obsessive-compulsive symptoms in schizophrenia: Prevalance and clinical correlates. Psychiatry Clin Neurosci. 2005;59:291-5.
- [Google Scholar]
- Obsessive-compulsive disorder in schizophrenia: Clinical characteristics and treatment. CNS Drugs. 2004;18:989-1010.
- [Google Scholar]
- Prevalence and clinical characteristics of obsessive-compulsive disorder and obsessive compulsive symptoms in Afrikaner schizophrenia and schizoaffective disorder patients. Afr J Psychiatry (Johannesbg). 2007;10:219-24.
- [Google Scholar]
- Relationships between obsessive-compulsive symptomatology and severity of psychosis in schizophrenia: A systematic review and meta-analysis. J Clin Psychiatry. 2009;70:70-82.
- [Google Scholar]
- The obsessive-compulsive inventory: Development and validation of a short version. Psychol Assess. 2002;14:485-96.
- [Google Scholar]
- The obsessive-compulsive inventory-revised (OCI-R): Validation of the German version in a sample of patients with OCD, anxiety disorders, and depressive disorders. J Anxiety Disord. 2008;22:734-49.
- [Google Scholar]
- Validation of a French version of the obsessive – Compulsive inventory-revised in a non-clinical sample. Eur Rev Appl Psychol. 2006;56:151-5.
- [Google Scholar]
- Psychometric properties and construct validity of the obsessive-compulsive inventory –Revised: Replication and extension with a clinical sample. J Anxiety Disord. 2006;20:1016-35.
- [Google Scholar]
- The mini-international neuropsychiatric interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22-33.
- [Google Scholar]
- The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261-76.
- [Google Scholar]
- Revising axis V for DSM-IV: A review of measures of social functioning. Am J Psychiatry. 1992;149:1148-56.
- [Google Scholar]
- The meaning and use of the area under a receiver operating characteristic (ROC) curve. Radiology. 1982;143:29-36.
- [Google Scholar]
- Research Methods in Applied Settings: An Integrated Approach to Design and Analysis. Abingdon: Routledge; 2011.
- Office of Medical Education and Research and Development. M.S.U.n.d. Likelihood Ratios Part 1: Introduction. Available from: http://www.omerad.msu.edu/ebm/Diagnosis/Diagnosis6.html






