Translate this page into:
Novel free-hand T1 pedicle screw method: Review of 44 consecutive cases
Address for correspondence: Dr. Mark A. Rivkin, 32 Conshohocken State Road, F-3, BalaCynwyd, Pennsylvania-19004, USA. E-mail: rivkin@comcast.net
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Summary of Background Data:
Multilevel posterior cervical instrumented fusions are becoming more prevalent in current practice. Biomechanical characteristics of the cervicothoracic junction may necessitate extending the construct to upper thoracic segments. However, fixation in upper thoracic spine can be technically demanding owing to transitional anatomy while suboptimal placement facilitates vascular and neurologic complications. Thoracic instrumentation methods include free-hand, fluoroscopic guidance, and CT-based image guidance. However, fluoroscopy of upper thoracic spine is challenging secondary to vertebral geometry and patient positioning, while image-guided systems present substantial financial commitment and are not readily available at most centers. Additionally, imaging modalities increase radiation exposure to the patient and surgeon while potentially lengthening surgical time.
Materials and Methods:
Retrospective review of 44 consecutive patients undergoing a cervicothoracic fusion by a single surgeon using the novel free-hand T1 pedicle screw technique between June 2009 and November 2012. A starting point medial and cephalad to classic entry as well as new trajectory were utilized. No imaging modalities were employed during screw insertion. Postoperative CT scans were obtained on day 1. Screw accuracy was independently evaluated according to the Heary classification.
Results:
In total, 87 pedicle screws placed were at T1. Grade 1 placement occurred in 72 (82.8%) screws, Grade 2 in 4 (4.6%) screws and Grade 3 in 9 (10.3%) screws. All Grade 2 and 3 breaches were <2 mm except one Grade 3 screw breaching 2-4 mm laterally. Only two screws (2.3%) were noted to be Grade 4, both breaching medially by less than 2 mm. No new neurological deficits or returns to operating room took place postoperatively.
Conclusions:
This modification of the traditional starting point and trajectory at T1 is safe and effective. It attenuates additional bone removal or imaging modalities while maintaining a high rate of successful screw placement compared to historical controls.
Keywords
Cervicothoracic
free-hand
pedicle screw
technique
thoracic
thoracic starting points
Introduction
Evolution of cervical spinal instrumentation has led to recent advancements in the treatment of complex spinal disorders stemming from numerous pathological processes. Cervical fusions alone have more than doubled over the past decade and reached over 157,000 annual procedures in 2008 just in the United States alone.[1] As a result, multi-level posterior cervical instrumented fusions are becoming more common in current practice. Several authors previously alluded to varying biomechanical stressors at the cervicothoracic junction often necessitating extension of construct to the upper thoracic segments.[234] However, pedicle screw fixation in upper thoracic vertebrae can be technically demanding as improper placement at T1 carries greater risk of canal encroachment and mediastinal compromise that lateral mass screws.
Consequently, safety and efficacy of thoracic screw insertion methods have been extensively described in the literature.[5678] These methods include free-hand placement, fluoroscopic guidance both with and without laminoforaminotomy, and computed tomography neuronavigation systems. Fluoroscopic imaging of the upper thoracic spine, however, presents a challenge due to vertebral anatomy, patient size, interference from skull clamp or surgical table, and positioning difficulties. CT-guided systems are associated with substantial financial commitment and are not readily available at most community medical centers. In fact, a survey of spine surgeons in the UK and Ireland found that only 14% of responders reported using some sort of spinal navigation equipment.[9] Additionally, both techniques increase radiation exposure to the patient and surgical team while often adding to overall surgical time.
We propose a novel free-hand technique for instrumenting the pedicle of the first thoracic vertebra as a part of cervicothoracic fusion. This modification of the classic starting point and trajectory described elsewhere[10] obviates the need for additional bone removal or expensive intraoperative imaging modalities while maintaining a high rate of successful screw placement compared to historical controls. The authors present their experience with this technique in 44 consecutive patients.
Materials and Methods
We performed a retrospective review of 44 consecutive patients at our institution who underwent cervicothoracic fusion requiring T1 pedicle screws for any pathology between June 2009 and November 2012. Institutional Review Board approval was obtained for this series. All procedures were performed by the senior author (S.S.Y.). Subaxial instrumentation consisted of lateral mass screws that were placed via standard techniques described elsewhere. Thoracic pedicle screws at T1 were placed using the method described in detail below. Patients were examined immediately in PACU postoperatively for neurological deficits. If no deficits were identified, every patient underwent a cervical CT on post-operative day 1. Routine continuous intraoperative electromyographic and somatosensory-evoked potential monitoring was not performed.
Accuracy of pedicle screw placement was recorded using the 5-grade Heary et al. classification: Grade 1 - screw completely within the vertebral body (VB) and pedicle, Grade 2 - screw contained within pedicle-rib complex with screw tip within VB, Grade 3 - screw tip located laterally or anteriorly to VB, Grade 4 - screw tip perforated inferior or medial pedicle border, Grade 5 - screw position that placed neural or vascular structures at risk and required removal or revision.[11] Post-operative CT scans were evaluated by three neuroradiologists as part of prospective work flow as well as by two neurosurgeons and two senior neurosurgical trainees.
Surgical technique
Patients underwent general endotracheal anesthesia and were placed prone on the operating room table. Rigid fixation utilizing a skull clamp was used for all procedures. A standard midline skin incision and subsequent subperiosteal dissection was used to gain exposure to cervicothoracic regions of interest. A decompressive laminectomy was performed where appropriate prior to instrumenting; however, in no patient this was done for the purpose of localizing the T1 pedicle. The spinous process, lamina, and transverse processes of T1 were meticulously exposed in all cases.
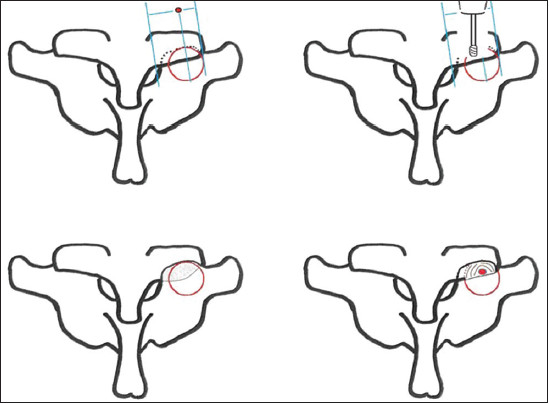
The classic starting point for the T1 pedicle screw has been described at the intersection of a line bisecting the transverse process and a line defining the lateral border of the pars.[1012] [Figure 1]. The new starting point for our free-hand method is more medial and superior. In order to expose the new starting point, electrocautery is used to define the C7/T1 articulation. In the medial-lateral direction, we first locate a point one-third of the way between the lateral border of C7 lateral mass and medial border of T1 lamina along the C7/T1 articulation [Figure 2]. A high speed burr is used to remove approximately 3 mm of bone from the inferior aspect of C7 lateral mass until the smooth cortical surface of the superior articular process of T1 is identified. A pilot hole drilled at the starting point on the T1 superior articular cortex delivers cancellous bone of the pedicle into view [Figure 3]. The 2 mm blunt, straight thoracic pedicle probe is used to cannulate the pedicle. In the cranial-caudal direction, the screw trajectory is perpendicular to the long axis of the T1 lamina [Figure 4]. In the medial-lateral direction, the trajectory parallels the angle between the tip of T1 spinous process and the contralateral starting point [Figure 5]. This trajectory stems from our observation that, in the axial plane, the geometry of the T1 vertebra from the tip of the spinous process to anterior aspect of body consistently resembles a parallelogram, with lateral borders defined by the two starting points. The pedicle probe is carefully advanced to a depth of 24-28 mm. Care is taken to appreciate perforation of cancellous bone the entire length of the pedicle and vertebral body. The probe should advance smoothly with consistent resistance. Abrupt loss of resistance indicates a pedicle breach while an increase in resistance indicates the probe is against cortical bone and trajectory must be re-evaluated prior to further advancement. A ball-tipped probe is then carefully inserted to investigate the integrity of the tract. A floor and four walls must be palpated before proceeding further. If a pedicle violation is suspected, the trajectory can be corrected with the straight pedicle probe. Subsequently, the pedicle is prepared to a depth of 15-20 mm with a tap that is 0.5mm smaller than the potential screw. A ball-tipped probe is once again introduced to confirm the integrity of the tract. Once satisfied with the bony confines of the tract, a 3.5 or 4.5 mm titanium screw is inserted to a predetermined depth of 24-28 mm based on preoperative imaging. Care must be taken to maintain the correct trajectory with screw insertion to avoid breaching the cortical margins of the developed tract.

- Top: An image demonstrating the difference between the classic starting point and one proposed in this report. Bottom: Location of the T1 pedicle with respect to adjacent superficial bony landmarks
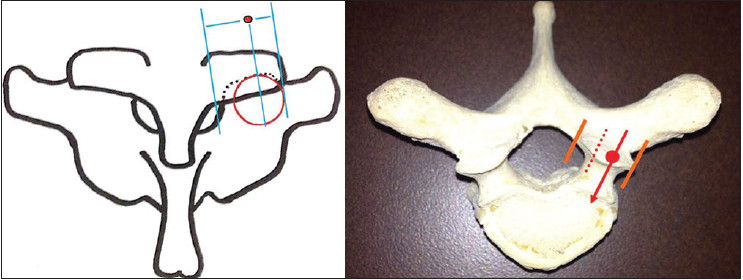
- An illustration (top) and a model (bottom) demonstrating the location of the starting point in the medial to lateral projection
- Top left: Medial to lateral orientation of the proposed starting point with respect to C7/T1 articulation. Top right: High speed drill is used to removing the inferior few millimeters of C7 lateral mass. Bottom left: The smooth cortical surface of T1 superior articular facet if uncovered once drilling is complete. Bottom right: High speed drill is used to break the cortex to deliver the cancellous bone of the T1 pedicle

- A model (top left), an illustration (bottom left), and post-operative CT scan (right) demonstrating the cranial-caudal trajectory of the T1 pedicle screw. The screw is inserted perpendicular to the long axis of the T1 lamina
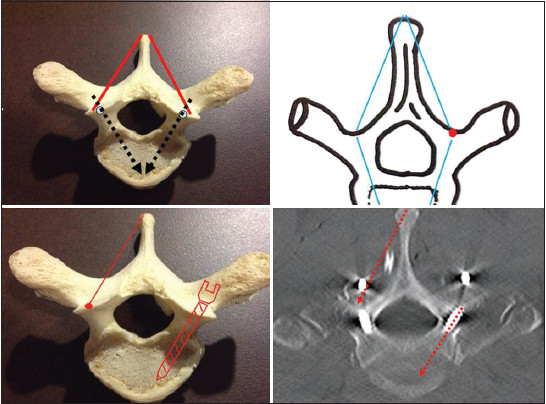
- A model (top left) and an illustration (top right) showing the parallelogram orientation of T1 vertebra. The medial-lateral screw trajectory is parallel to the angel between the tip of spinous process and contralateral starting point. Bottom left: A model demonstrating a phantom screw inserted according to the proposed trajectory. Bottom right: A post-operative CT scan showing a T1 pedicle screw following the proposed trajectory
After successful placement of thoracic screws, subaxial instrumentation is completed. Parallel titanium rods are placed bilaterally. The wound is copiously irrigated and closed in standard layered fashion. A detailed neurological examination is performed in PACU in the immediate post-op period.
Results
Between June 2009 and November 2012, 44 consecutive patients underwent a posterior cervicothoracic instrumented procedure with pedicle screws placed to at least T1. For all cases, T1 pedicle screws were inserted utilizing the above-described technique. There were 21 males and 23 females in the study and the mean age of the patient cohort was 60.9 years. There were 87 total T1 pedicle screws included in the final analysis [Table 1]. One patient underwent C2 to T2 fixation with placement of only a unilateral left T1 pedicle screw due to right T1 pedicle fracture. All 44 patients were subjected to a postoperative CT on day 1. A C3-T1 fusion was the most common construct, placed in 30 (68.2%) patients. There were no new neurologic deficits or returns to the operating room secondary to hardware placement.

Heary Grade 1 placement occurred in 72 (82.8%) screws, Grade 2 in 4 (4.6%) screws and Grade 3 in 9 (10.3%) screws. All Grade 2 and 3 screws breached by <2 mm with one Grade 3 screw breaching 2-4 mm laterally. Two screws (2.3%) were Grade 4 placements, breaching medially by less than 2 mm [Figure 6]. Both of these patients remained asymptomatic postoperatively. Seventy-six screws (87.4%) terminated within the T1 vertebral body. At last follow-up, no hardware failures were noted at T1 level.

- Right T1 pedicle screw (top) and left T1 screw (bottom) breached medially by less than 2 mm. These were the only two Grade 4 perforations in the study
Discussion
As multilevel cervical instrumented fusions have become increasingly common over the past decade, many surgeons have adapted the practice of extending posterior cervical constructs past the cervicothoracic junction (CTJ).[23] Lapsiwala and Benzel described several fundamental guidelines to reduce construct failure in this region.[2] Key aspects include traversing the CTJ to a neutral vertebra for longer cervical fusions and the avoidance of ending constructs at the CTJ. Extending longer cervical constructs to at least T1 is desirable for biomechanics purposes. First thoracic vertebra has a relatively consistent pedicle size and transverse angle.[13] The T1 facet joint is oriented in the coronal plane, and limits motion in flexion and extension more than at the cervical joints.[23] At all thoracic levels, the medial pedicle cortex is two to three times thicker than the lateral cortex conferring added strength against pedicle breach.[14] Additionally, T1 pedicle screws have greater pull-out strength and impart enhanced stability of three-column fixation to cervical constructs when compared to lateral mass screws alone.[3101516] Yet another consideration supporting extension of posterior cervical constructs to T1 level is the difficulty of instrumenting the pedicle at C7, thus presenting the option of skipping C7 altogether if necessary.
Pedicle screw accuracy rates in the present series are similar to slightly higher than historical controls, without the use of additional imaging or navigation. In our study, there were 87 free-hand pedicle screws placed at T1. Of these, 85 (97.7%) were Heary Grade 1-3, with two Grade 4 placements. Of note, 72 (82.8%) T1 screws inserted were contained completely within the pedicle and VB. Furthermore, there were no clinically significant screw misplacements as defined by neurologic deficit or returns to OR, further supporting the safety and efficacy of our method.
Several previous reports assessed the utility of free-hand thoracic pedicle screw placement. Kim and colleagues[10] reviewed placement of 577 thoracic pedicle screws, with 36 (6.2%) screws demonstrating moderate cortical perforation, 10 (1.7%) of which violated the medial pedicle cortex. After a 10 year follow-up however, no patients in their series demonstrated any evidence of neurologic, visceral, or vascular complications, leading the authors to conclude that free-hand method of placement was accurate, reliable, and safe. Gelalis et al. conducted a meta-analysis of prospective trials comparing various pedicle screw insertion methods. The authors reported the range of thoracic free-hand screws that were contained within the pedicle to be 69-94%.[5]
Placement accuracy specifically for upper thoracic pedicle screws has also been reviewed by several groups. Lee et al. compared accuracy of pedicle screw insertion at the CTJ by “open” technique with lamino-foraminotomy or laminectomy windows, versus “closed” insertion with either 2D fluoroscopy or 3D CT technique.[17] The accuracy for screws completely within the pedicles was 70.9%, 81%, and 89%, respectively. In a recent retrospective review, Sugimoto et al. assessed pedicle screw placement utilizing three-dimensional fluoroscopy.[8] Of 90 pedicle screws placed from C7 to T2, 87 (96.7%) were classified as grade 1. Specifically, 30/30 (100%) of T1 pedicle screws were grade 1.
The classic starting point for the T1 pedicle screw as described by Kim et al.[10] is at the intersection of a line bisecting the transverse process and a line defining the lateral border of the pars. We propose a starting point medial and superior to the traditional method. A more cephalad starting point minimizes the risk of inferior pedicle breach. A more medial starting point facilitates visualizing the “parallelogram”, as previously described, which is crucial for medial-lateral trajectory of the proposed method. Medial breaches occurred with just two of our screws, both less than 2 mm and asymptomatic, despite a more medial starting position. In the medial-lateral direction, the trajectory parallels as the angle between the tip of the T1 spinous process and the contralateral starting point. In the cranial-caudal direction, the screw trajectory is perpendicular to the long axis of the T1 lamina. The steep trajectory appears to be sufficient to compensate for starting higher on the pedicle as evidenced by no superior pedicle breaches in our cohort.
We envision several advantages of the proposed free-hand method. Utilization of bony landmarks as opposed to predetermined angles for screw trajectory equips this approach with an inherent mechanism to adjust for anatomic variability as compared to alternative approaches. This method eliminates the need for any imaging modalities during thoracic instrumentation. The CTJ is not easily imaged with fluoroscopy in the lateral position as surrounding bony structures obstruct direct view. Moreover, determining entry point in AP view is challenging secondary to patient anatomy, skull clamp, surgical table, and positioning.[8] Hence, removing the need for imaging allows for less radiation exposure to the patient and surgical team while potentially decreasing the operative duration by eliminating fluoroscopy set-up time. Moreover, the present method does not necessitate any additional bone removal or laminotomy windows. We also experienced less difficulty with rod contouring when connecting long cervicothoracic segments as the more medial screw head position at T1 is in line with lateral mass instrumentation.
The novel free-hand method eliminates the need for expensive navigation equipment that is not readily available at most institutions. This may facilitate cost reduction in both capital and operational budgets. The cost of certain navigation systems can approach $500,000.[18] Additionally, these systems may prolong surgical times and the price of utilizing an operating suite has been estimated at $93 per minute.[18] Even fluoroscopic imaging comes at a price. The operational cost of intraoperative fluoroscopy can reach as much as $233.35 per case (2011, US$).[19]
There are several limitations to the present study. The data was obtained in a retrospective fashion. There were also no clinical outcome measures recorded except that no patient returned to the operating room for screw reposition or experienced a new neurological deficit throughout the duration of the study. Lastly, no cadaveric biomechanical investigations were performed with respect to T1 screw pull out strength utilizing this method.
Conclusion
Our modification of the classical starting point and trajectory maintains a high accuracy rate of successful screw placement in a safe, cost-effective fashion. It obviates the need for additional bone removal and imaging while maintaining a high rate of successful screw placement compared to historical free-hand methods. This technique allows for the potential expansion of the surgical armamentarium by encompassing more complex cervicothoracic procedures, especially at community medical centers with limited resources.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Spinal fusion in the United States: Analysis of trends from 1998 to 2008. Spine (Phila Pa 1976). 2012;37:67-76.
- [Google Scholar]
- Surgical management of cervical myelopathy dealing with the cervical-thoracic junction. Spine J. 2006;6(Suppl 6):268S-73S.
- [Google Scholar]
- Subaxial cervical and cervicothoracic fixation techniques-indications, techniques, and outcomes. OrthopClin North Am. 2012;43:19-28, vii.
- [Google Scholar]
- Biomechanics of stabilization after cervicothoracic compression-flexion injury. Spine (Phila Pa 1976). 2005;30:1505-12.
- [Google Scholar]
- Accuracy of pedicle screw placement: A systematic review of prospective in vivo studies comparing free hand, fluoroscopy guidance and navigation techniques. Eur Spine J. 2012;21:247-55.
- [Google Scholar]
- Accuracy of image-guided pedicle screw placement using intraoperative computed tomography-based navigation with automated referencing. Part II: Thoracolumbar spine. Neurosurgery. 2011;69:1307-16.
- [Google Scholar]
- Image-guided pedicle screw insertion accuracy: A meta-analysis. IntOrthop. 2009;33:895-903.
- [Google Scholar]
- Clinical accuracy of three-dimensional fluoroscopy (IsoC-3D)-assisted upper thoracic pedicle screw insertion. Acta Med Okayama. 2010;64:209-12.
- [Google Scholar]
- Pediclescrewsurgery in the UK and Ireland: A questionnairestudy. Open Biomed Eng J. 2011;5:90-7.
- [Google Scholar]
- Free hand pedicle screw placement in the thoracic spine: Is it safe? Spine (Phila Pa 1976). 2004;29:333-42.
- [Google Scholar]
- Thoracic pedicle screws: Postoperative computerized tomography scanning assessment. J Neurosurg. 2004;100(Suppl Spine 4):325-31.
- [Google Scholar]
- Posterior thoracic segmental pedicle screw instrumentation: Evolving methods of safe and effective placement. Neurol India. 2005;53:458-65.
- [Google Scholar]
- Thoracic pedicle screw placement: Free-hand technique. Neurol India. 2005;53:512-9.
- [Google Scholar]
- Internal architecture of the thoracic pedicle. An anatomic study. Spine (Phila Pa 1976). 1996;21:264-70.
- [Google Scholar]
- Placement of pedicle screws in the thoracic spine. Part I: Morphometric analysis of the thoracic vertebrae. J Bone Joint Surg Am. 1995;77:1193-9.
- [Google Scholar]
- Morphometry of the thoracic and lumbar spine related to transpedicular screw placement for surgical spinal fixation. Spine (Phila Pa 1976). 1988;13:27-32.
- [Google Scholar]
- Clinical accuracy of cervicothoracic pedicle screw placement: A comparison of the “open” lamino-foraminotomy and computer-assisted techniques. J Spinal Disord Tech. 2007;20:25-32.
- [Google Scholar]
- Cost-effectiveness of confirmatory techniques for the placement of lumbarpediclescrews. Neurosurg Focus. 2012;33:E12.
- [Google Scholar]






