Translate this page into:
Neurogenic vision loss: Causes and outcome. An experience from a tertiary center in Northern India
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Vision loss can be a consequence of numerous disorders of eye and neural pathway conveying visual input to brain. A variety of conditions can affect visual pathway producing neurogenic vision loss. The presentation and course of vision loss depends on the site of involvement and underlying etiology. We conducted this unprecedented study to evaluate the characteristics and outcome of various diseases of the visual pathway.
Materials and Methods:
In this prospective cohort study, we evaluated 64 patients with neurogenic visual impairment. Ophthalmological causes were excluded in all of them. Their presentation, ophthalmological characteristics and investigation findings were recorded. These patients were followed up till 6 months.
Results:
Out of 69 patients evaluated, 5 were excluded as they had ophthalmological abnormalities. The remaining 64 cases (113 eyes) were enrolled. 54 cases were due to diseases of anterior visual pathway and rest 10 had cortical vision loss. The etiologic distribution is as follows: Isolated optic neuritis- 12 (19%), multiple sclerosis- 4 (6.3%), neuromyelitis optica- 5 (7.9%), tubercular meningitis- 15 (23.8%), non-arteritic ischemic optic neuropathy, ischemic optic neuropathy complicating cavernous sinus thrombosis, cryptococcal meningitis, malignant infiltration of optic nerve, Crouzon's syndrome, calvarial thickening and traumatic occipital gliosis- 1 (1.6%) case each, idiopathic intracranial hypertension, pituitary adenoma, acute disseminated encephalomyelitis, posterior reversible leukoencephalopathy- 3 (4.8%) cases each, cortical venous thrombosis 5 (7.9%), subacute scleroing panencephalitis- 4 (6.3%) cases.
Conclusions:
The diseases of anterior visual pathway were much more common than cortical vision loss. A majority of our patients had severe impairment of vision at presentation.
Keywords
Cortical venous thrombosis
optic neuritis
vision loss
Introduction
Vision impairment can be a reason of severe disability for an individual. Evaluating patients with neuro-ophthalmic symptoms may sometimes seem to be a daunting task as visual deficits in such patients involve complex neuro-anatomic pathways. The vision can be affected from a myriad of local ophthalmologic conditions and those affecting the neural structures conveying visual information from retina to brain. Such neuro-ophthalmologic diseases can be due to damage at any location from optic disc, optic nerve, optic chiasm, optic tract to optic radiation and occipital cortex. Various causes of neurogenic vision loss include: Optic neuropathy (demyelinating, ischemic, toxic, infectious, secondary to chronically raised intracranial pressure (ICP)), compression of the visual pathway because of space occupying lesions and tubercular arachnoiditis in the optochiasmatic region, ischemic involvement of the post-chiasmatic visual pathway as in case of stroke, cerebral venous thrombosis (CVT), cortical vision loss due to various etiologies such as stroke, posterior reversible encephalopathy syndrome (PRES), subacute sclerosing panencephalitis (SSPE) etc.[12345678]
Thus, the central concept while evaluating these patients is localization of the site of lesion based upon various clinical findings aided by ancillary tests. The involvement of different parts of visual pathway produces characteristic symptomatology and ophthalmological findings which can help to localize the site of lesion. For example, optic neuropathies are characterized by impairment of visual acuity and color vision, presence of relative afferent pupillary defects, abnormal appearance of optic disc, visual evoked responses and visual field defects.[9] On the other hand, damage at optic chiasm onward produces the characteristic visual field defects reflecting the arrangement of nerve fibers at these sites. The course, severity, examination findings and prognosis of visual impairment are further determined by the etiology. It requires a systematic approach to determine the site of involvement and the underlying etiology in order to initiate an appropriate treatment and determine the prognosis. Apart from scattered case reports, there has been no published data which has studied the spectrum of neurogenic vision loss. We planned this study to determine causes of neurogenic vision loss in patients admitted with neurogenic visual impairment in our department and to outline the pattern of presentation, findings of examination and investigations, response to treatment and prognosis.
Materials and Methods
This was a prospective cohort study done in Department of Neurology at King George Medical University, Uttar Pradesh, Lucknow over a span of 2 years (October 2011-September 2013). An approval from the institutional research ethics committee was obtained prior to beginning of the study. A written informed consent was also obtained from every patient or their guardian in the language they understand the best.
Selection criteria
Inclusion criteria
We enrolled patients with visual impairment defined as visual acuity of 6/18 or worse in one or both eyes whereas blindness was defined as visual acuity worse than 3/60 as per the standard WHO definition.[10]
Exclusion criteria
Patients with local ophthalmological causes contributing to visual impairment were excluded from the study.
Assessment procedure
Patients who satisfied the selection criteria were included in the study. After a written informed consent, detailed history was obtained and thorough neurological and systemic examination was done in all patients. An exhaustive evaluation was done by an ophthalmologist. The visual acuity was assessed using Snellen's chart and color vision was assessed using Ishihara chart. Funduscopic examination was done in all the patients to look for evidence of papilledema or optic atrophy. Patients were further categorized into groups based on visual acuity as follows: Visual impairment: <6/18-6/60, severe visual impairment: <6/60-3/60, blind: 3/60-1/60, 1/60-PL, totally blind: No PL.
Various approaches were used by ophthalmologist to rule out ocular conditions as a cause of non-neurogenic visual impairment such as detailed ophthalmological examination including funduscopic evaluation, indirect ophthalmoscopy, pin-hole testing, B-scan wherever necessary The specific investigations included visual evoked potentials (VEP), visual field charting, central nervous system (CNS) imaging using computed tomography or magnetic resonance imaging (MRI) of brain and optic nerve (with gadolinium enhancement), electroencephalogram (EEG). Magnetic resonance venogram (MRV) and magnetic resonance arteriogram (MRA) were obtained in patients suspected to be having cortical venous thrombosis (CVT) and vasculopathy of CNS, respectively. Cerebrospinal fluid examination including total and differential cell count, protein, sugar, staining with gram stain, Zeil-Neilson (Z-N) stain and Indian ink was performed in patients with optic neuritis and meningitis. CSF manometry was performed in patients in whom idiopathic intracranial hypertension (IIH) was suspected.
The patients were further divided depending on portion of visual pathway affected as optic neuropathy, chiasmal lesions, optic tract lesions and cortical blindness, defined by absence of ocular pathology, preserved pupillary light reflex and associated neurologic signs. In the optic neuritis group, CSF oligoclonal band, IgG index and serum aquaporin-4 antibody tests were obtained. In patients with tuberculous meningitis, polymerase chain reaction (PCR) and culture for acid fast bacilli (AFB) were performed. In patients with CVT, thrombophillic profile including the serum vitamin B12, homocysteine level, protein C, protein S, anti-thrombin III level, Leiden factor V, anti-nuclear antibody, anti-cardiolipin antibody and APLA antibody were estimated. The treatment was given according to the etiology.
Follow up
Patients were followed up at 6 months for assessing the improvement in visual acuity by means of Snellen's chart.
Result
A total of 69 patients with vision loss were examined, 5 cases were excluded as they had ocular abnormalities resulting in visual impairment. Thus, 64 patients were included in the study. Study progress is depicted in flow chart. Among the excluded patients, two had retinal detachment, two had vitreous hemorrhage and one patient had panuveitis. Out of 64 cases included in study, 27 cases were male and 37 cases were female. The distribution of cases as per the etiology is depicted in Figure 1. Majority of cases were due to affection of the optic nerve. The distribution of disease as per location is depicted in Figure 2.
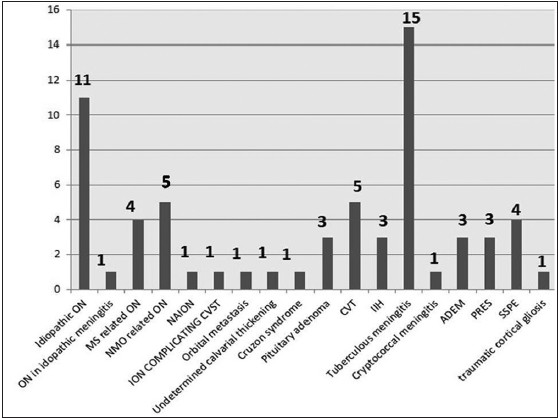
- Distribution of cases according to etiology
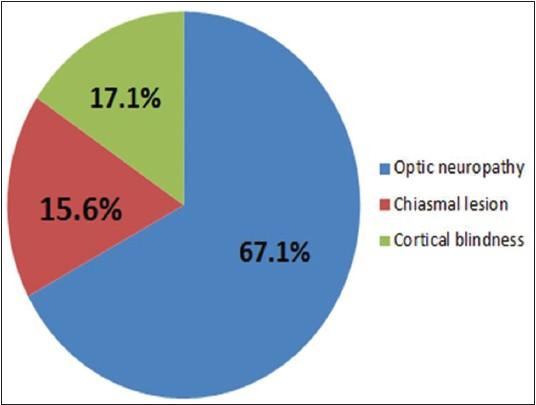
- Distribution of cases according to the site of lesion
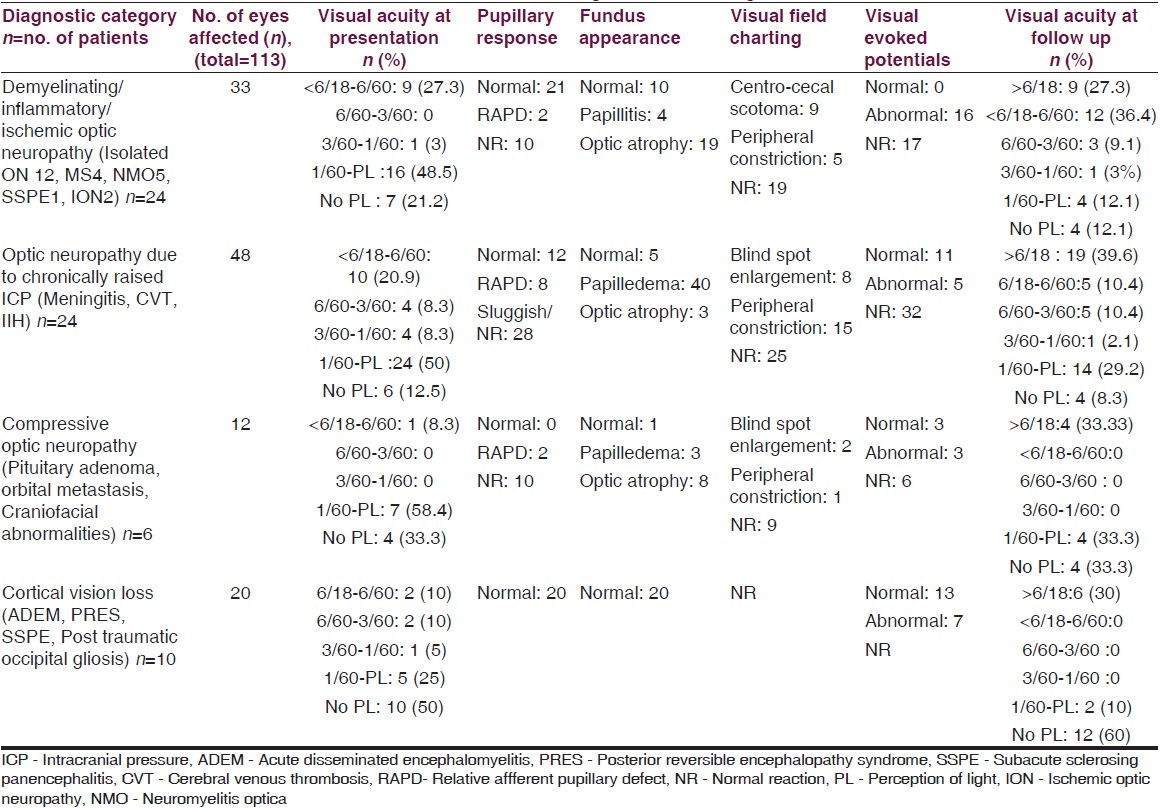
Among the 64 patients (113 affected eyes), 24 (37.5%, 33 affected eyes) had demyelinating/inflammatory/ischemic optic neuropathy, 24 (37.5%, 48 affected eyes) had optic neuropathy due to chronically raised ICP, 6 (9.4%, 12 affected eyes) had compressive optic neuropathy [pituitary adenoma, orbital metastasis, craniofacial abnormalities] and 10 (15.6%, 20 affected eyes) had cortical vision loss. Their major clinical characteristics are summarized in Table 1.
Anterior visual pathway
Optic neuritis
Among 21 cases of optic neuritis, the average age was 27.3 years, the youngest being 10 years and eldest being 51 years. Females (66.7%) outnumbered males. Eleven had idiopathic optic neuritis where an etiology was not identified, 5 were part of neuromyelitis optica, 4 were part of multiple sclerosis and 1 patient had idiopathic meningitis with recurrent facial palsy. Optic neuritis was unilateral in 13 (61.9%) and bilateral in 8 (38.1%) cases. The number of days of vision deterioration ranged from 6 to 20 days. Peri-orbital pain was reported by seven patients (33.3%). Visual acuity was poor in most; perception of light or worse in 14 (66.7%). Color vision was impaired in cases with poor vision. Papillitis was observed in 4 eyes, disc was normal at onset in 10 eyes indicating retrobulbar optic neuritis (RBN) and optic atrophy was seen in rest 14. Retinal folds and vascular sheathing was noted in one case with bilateral papillitis. The visual field charting could not be performed in 17 cases owing to poor acuity. Central/centrocaecal scotoma in nine and peripheral constriction of field in four patients was demonstrated. VEP was not recordable in eight patients and was prolonged in rest of the patients indicating reduction in conduction velocity. The initial MRI brain showed white matter hyperintensity on a T2-weighted sequence in only 1 out of 11 and the repeat MRI too in this case turned out to be normal. Optic nerve T2 hyperintensity was observed in two cases only on MRI. On follow up (6 months to 1 year) visual acuity improved to 6/18 or better in 8 (38.1%) patients only.
Ischemic optic neuropathy
Ischemic optic neuropathy was found in two patients: One was 72-year-old with atherosclerotic bilateral carotid artery stenosis and another was 15-year-old boy with fungal sinusitis complicated by cavernous sinus thrombosis. In both of them presentation was quite similar and consistent with vascular optic neuropathy: Rapid progression (<12 hours), no PL and presence of optic atrophy in the affected eye at onset, VEP and field charting were unrecordable. Visual acuity improved to 6/60 in first case while PL was absent in left eye even after 6 months in second case.
Meningitis
15 patients of tubercular meningitis (TBM) and one patient of cryptococcal meningitis reported with vision impairment.
TBM
In 15 cases of TBM (8 males, 7 females), the mean age was 20.5 years, and among them optochiasmatic tuberculoma (OCT) and optochiasmatic arachnoiditis (OCA) were present on brain imaging in 6 and 2 cases, respectively. Hydrocephalus was observed in all of them. An interval of 16-24 weeks between initiation of anti-tubercular drugs and onset of vision complaints was observed in three patients of OCT. In the rest, the mean duration of vision deterioration was 36.7 days. Visual acuity was quite poor in patients with OCT/OCA (HM to PL) compared to patients without these findings. Chronic papilledema was noted in 13 and optic atrophy in 2 patients. The average CSF protein concentration was 2.57 g/L.
Cryptococcal meningitis
This patient presented with bilateral vision loss of 20 days duration. The visual acuity in each eye deteriorated to no PL acutely over 24 hours. Fundus examination revealed optic atrophy in right and chronic papilledema in left eye. CSF pressure was 327 mm of CSF. CSF India ink staining and crypotococcal antigen titer by latex agglutination test were positive. There was no improvement in vision and patient expired after 6 month of antifungal therapy.
Cortical venous thrombosis
Five patients presenting with vision loss and headache were diagnosed as CVT. The mean age was 22.8 years (10-34): Three females and two males. The mean duration of vision loss was 24.2 days. Out of 10 affected eyes, the visual acuity ranged from <6/60 in 4 to worse than 3/60 in 6 eyes. Chronic papilledema was observed at presentation in all of them. VEP was not recordable in 7/10 eyes and was abnormal in the remaining patients. Visual field was constricted with enlargement of blind spot in four and in other eyes it was not recordable as the vision was too poor. MRI was normal but MRV showed superior sagittal sinus thrombosis in four patients and transverse and sigmoid sinus thrombosis in three patients. Hyperhomocystinemia was found in one patient and in rest no underlying predisposing factor was identified. On follow up vision had improved to better than 6/18 in 4/10 eyes.
Idiopathic intracranial hypertension
All three patients diagnosed as IIH were young women aged 22-37 years. The duration of vision loss in these patients ranged from 29 to 41 days and visual acuity was worse than FC. Chronic papilledema was noted in all of them. VEP was abnormal in two and not recordable in rest. Visual field charting field charting was not feasible owing to poor vision. The CSF pressure ranged from 297 to 325 mm of CSF. The CSF cytology and biochemistry were normal, and no secondary causes of raised ICP were found. MRI and MRV were normal. The vision remained static in them.
Pituitary macroadenoma
Three patients admitted with complaints of vision loss and headache were diagnosed as having pituitary adenoma. Their age ranged between 42 and 60 (two females and one male), duration of vision impairment was 2 days in one patient to 8 weeks in other two patients. In three of them visual acuity was poor PL to FC at 1 m. Optic atrophy was noted in two patients with slowly progressive vision loss. Visual field charting was not possible due to poor vision in all of them. One patient had clinically obvious acromegaly. MRI showed well-circumscribed heterogeneous mass lesions arising from sella extending into the supratentorial region. Fluid level was observed in the patient with acute worsening of vision. Post-operatively vision improved to 6/9 in the patient with intra-tumoral fluid level; however, vision was limited to finger counting (FC) at 2 m in the remaining two.
Malignant compression of intra-orbital optic nerve
A 12-year-girl presented with bilateral vision loss of 1 week duration along with headache for past 1 month and fever with right ankle pain since 3 months. Bilateral proptosis was present, pupillary reaction to light reflex was sluggish on both sides. Visual acuity in right eye and left eye was 6/24 and finger counting at 1 m. Bilateral papilledema was present. Enlarged blind spot in both eyes with peripheral constriction in left eye were observed. Computed tomography revealed intra-orbital mass around the optic nerve bilaterally and, in addition, metastatic lesions invading the calvarium and in the falx cerebrum. Patient was diagnosed as Ewing's sarcoma (primary in right ankle) on biopsy from orbital lesions. After receiving chemotherapy and radiotherapy for 6 months visual acuity improved to 6/6 bilaterally.
Craniofacial abnormalities
A 9-year-old girl diagnosed as Crouzon's syndrome and other 27-year-old male presented with painless bilateral symmetrical vision loss 1-2.5 years duration. In both of them the visual acuity after presentation was HM and worse, bilateral optic atrophy was noted, VEP and visual field were unrecordable.
Sub-acute sclerosing panencephalitis (SSPE)
A 3-year-old girl presented with spastic quadriparesis following bilateral acute vision loss in the preceding year. Optic atrophy was present bilaterally and VEP was unrecordable. Sub-acute sclerosing panencephalitis (SSPE) was diagnosed by the presence of stereotyped myoclonus, type I periodic complexes on EEG and positive measles antibody titer was 1/512 in CSF. MRI brain and spine were normal.
Cortical vision loss
Acute disseminated encephalomyelitis
Among three patients (two males, one female) visual acuity was in the range of 6/18-6/60 in two, 6/60-1/60 in three and 1/60-PL in one eye. Color perception was lost in three of them. MRI brain revealed multiple T2 hyperintense lesions which enhanced after gadolinium administration. After a course of intravenous methylprednisolone, vision improved to 6/18 or better in all 3 patients.
SSPE
All three were young adults (two males, one female) in the age group 15-20 years and they had vision impairment as their presenting complaint which progressed over one to three months. At presentation blindness was present in all. Multiple non-enhancing T2 hyperintense lesions in parieto-occipital white matter were observed on MRI. The diagnosis was established based on presence of periodic myoclonus with characteristic periodic epiletiform discharges and significantly elevated anti-measles IgG titre in CSF as per Dyken's criteria.[1]
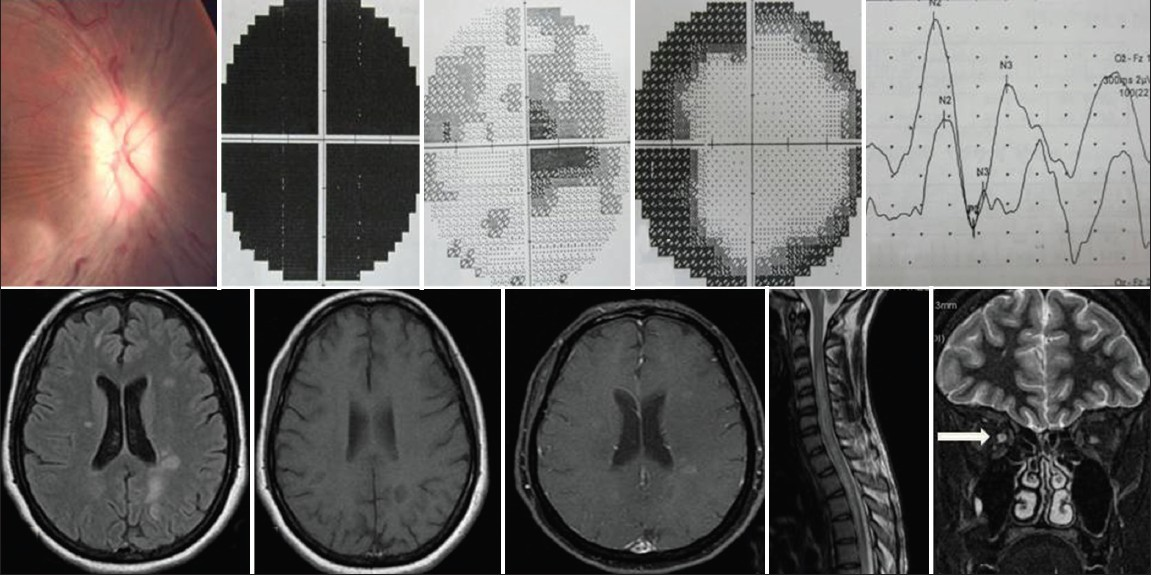
Posterior reversible leukoencephalopathy syndrome
Three women in their peripartum period developed painless, bilaterally simultaneous difficulty in vision along with eclampsia. At presentation visual acuity was 1/60-PL in 2 and no PL in 4 eyes. MRI brain showed T2 hyperintense lesions in parieto-occipital white matter with restriction on Diffusion weighted imaging along with high apparent diffusion coefficient values. Magnetic resonance angiograpghy (MRA) revealed non-visualization of left internal carotid artery with segmental constriction in right vertebral, bilateral superior cerebellar and posterior cerebral arteries in one patient and constriction of posterior cerebellar artery in other two patients. There was only modest improvement to 6/36 in one patient and in other two only perception of light was present at 6 months after onset [Figures 3 and 4].
- (a) Fundus photograph showing papillitis. (b) Visual field charting showing diffuse attenuation in a patient of optic neuritis. (c and d) Predominantly centrocecal scotoma and peripheral constriction of field in patients of optic neuritis are shown. (e) VEP (flash) with delayed latency of P2 with normal amplitude in a patient of optic neuritis. (f-h) Classical MRI findings in a patient of multiple sclerosis are shown. (i and j) Involvement of cervical and thoracic cord in a patient of NMO and bilaterally hyperintense (T2-weighted sequence) optic nerves
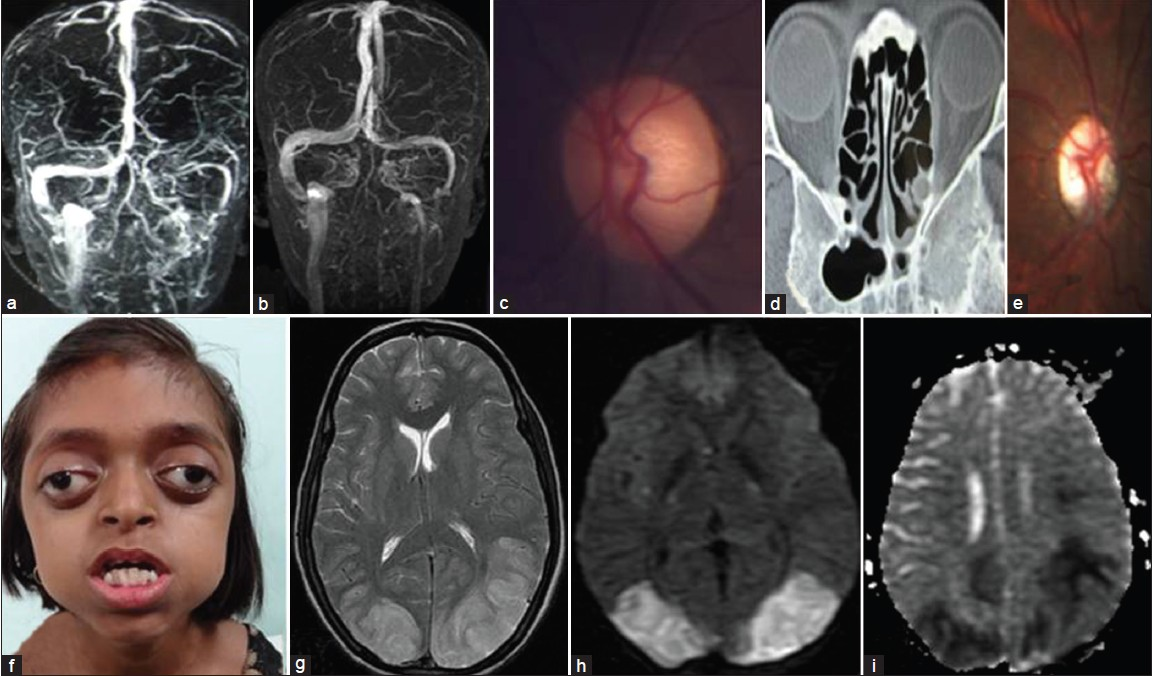
- (a-c) Thrombosis of superior sagittal sinus and left transverse sinus seen on baseline MRV which has resolved on repeat MRV, and normal optic disc on follow up. (d and e) Severe bilateral orbital canal stenosis and optic atrophy in a patient with calvarial thickening of undetermined etiology. (f) Photograph of a girl depicting the typical facies of Crouzon syndrome. (g-i) Bilateral hyperintensity in occipito-parietal region on T2 weighted sequence with restricted diffusion on diffusion-weighted imaging (DWI) and apparent diffusion coefficient mapping in a patient of PRES
Discussion
Anterior visual pathway
Optic neuritis
The typical optic neuritis is characterized by following features: Onset 20-50 year age group, unilateral, progression for less than 2 weeks, recovery by 90 days and optic atrophy usually after 4-6 weeks, visual acuity better than perception of light, pain (90%), Uhthoff's phenomenon, Moore's lighting streaks and overall better prognosis with visual acuity better than 6/12 in 90% of cases. In Asia and Africa following atypical features have been noted: Usually bilateral, much severe visual disability, papillitis and peripapillary hemorrhage and exudates, and overall a poorer prognosis as compared to typical optic neuritis.[2]
The majority of patients in our study were in the younger age group with a female preponderance which is similar to that reported in Optic Neuritis Treatment Trial (ONTT) and Asian studies with the exception of Jain et al who noted a male preponderance.[34] A substantial proportion of cases (38.1%) had bilateral presentation, higher than in ONTT. Incidence of pain accompanying vision loss was 33%, comparable to Asian data where this feature is seen less often compared to western population. The rate of improvement (only 31.0% improving to acuity ≤6/18) was far lower than that reported in ONTT (93.4%) and even the Asian studies.[3411] It is noteworthy that vision improved to 6/18 in all four cases of MS corroborating with findings of ONTT while only one out of five patients of NMO had similar recovery. None of the non-MS, non-NMO case of optic neuritis progressed to MS.
Ischemic optic neuropathy
Among the patients who presented with ischemic optic neuropathy, the elderly male presented with history of noting vision loss on waking up in morning which is considered to be quite typical in non-arteritic ischemic optic neuropathy (NAION). This feature of NAION has been attributed to hypotension occurring during sleep in predisposed individuals. Though classically optic disc edema is seen acutely in NAION, optic atrophy was noted first in our patient probably as the presentation was delayed by 2 weeks.[9] In 75% of cases moderate to severe visual acuity impairment with poor recovery of vision is reported, this explains the poor outcome in our case.
The other, young boy, with septic cavernous sinus thrombosis had vision loss in left due to ischemia of optic nerve head which is a rare occurrence. The most likely mechanism of ischemia would be vasculitis induced by infective cavernous sinus thrombosis.[5]
Meningitis
TBM
The prognostic factors for poor vision in TBM as proposed by Sinha et al. include: Papilledema, cranial nerve palsies, raised cerebrospinal fluid protein (>1g/L), and presence of optochiasmatic arachnoiditis in MRI.[6] In our series of 15 cases above-mentioned features were noted; all had hydrocephalus and CSF protein >1 g/L, papilledema in 10, OA in 2, cranial palsy in 9/15 and 53.3% had inflammatory changes at the optic chiasm.
Crypotococcal meningitis
Rex et al. assessed risks factors for vision loss in patients of cryptococcal meningitis and observed that the presence of combinations of three factors: Papilledema, elevated CSF opening pressure and positive India ink staining correlated with vision impairment (P < 0.00001).[12] In our patient too all the above-mentioned three characteristics were observed.
Cortical venous thrombosis
CVT may present as: Isolated intracranial hypertension, focal cerebral signs, cavernous sinus thrombosis, subacute encephalopathy or unusual presentations. It is known that superior sagittal sinus thrombosis usually leads to raised ICP and vision impairment, though it can also cause venous infarcts leading to paraparesis. Moreover, the lateral venous sinus occlusion is notorious for presenting as only headache due to raised ICP.[7] In our cases none had focal parenchymal lesions, though, one patient had multiple cranial nerve palsies. The poor vision was noted when the duration of vision loss was prolonged and the outcome was dismal in those who had poor vision at presentation.
Idiopathic intracranial hypertension
The major neurologic complication of IIH is progressive impairment of vision. Baheti et al. in their study of 43 patients, 80 eyes were found to have moderate to severe vision loss. The duration of progression of vision impairment ranged from 10 to 270 days.[13] They observed that early severe vision loss was associated with poor visual prognosis. The patients in our study had relatively early severe vision loss, the duration ranging from 29 to 41 days with poor outcome.
Pituitary macroadenoma
All three patients had very low vision at presentation, progressive in two and acute in one. Prompt decompression resulted in marked improvement in the patient with pituitary apoplexy. However, in rest of the two, poor vision persisted even after tumor resection which could be explained by the long duration of vision impairment before treatment, presence of optic atrophy and large tumor size.[1415]
Malignant compression of intra-orbital optic nerve
Ewing's sarcoma of bone is seen in adolescent individuals, arising from the diaphysis and frequently metastasizing to bone, lungs and bone marrow. Its propensity to metastasize to CNS is very low (6.3%).[16] Though fundus is either normal or atrophic in compressive optic neuropathy, papilledema occurs if optic nerve compression is intra-orbital.
Craniofacial abnormalities
A 9-year-old girl had facies typical of Crouzon syndrome including shallow orbits with proptosis, hypertelorism with slanting eyes, maxillary hypoplasia with mal-occlusion and a pinched nose. The causes of vision impairment in Crouzon syndrome are strabismus, keratoconus, chronic papilledema, chronic optic nerve compression and exposure keratitis.[17] In our case most likely it resulted from long-standing hydrocephalus.
In other case, the optic nerve was compressed within the narrowed optic canal (inner diameter: 1mm). The normal diameter of optic canal is 3.57 ± 0.61 mm as observed by Liu et al. in study of 200 normal subjects.[18] The etiology of calvarial thickening in this patient remained undetermined.
SSPE
Optic atrophy is relatively uncommon in SSPE; it was reported in three cases by Khadilakar et al. Our case had resemblance to neuromyelitis optica. A similar case was reported by Sharma et al. described a similar case of SSPE in a young adult lady who had vision loss followed years later by myelopath.[19]
Cortical vision loss
In our 10 cases of cortical blindness vision was worst in patients suffering from SSPE, PRES and traumatic cortical gliosis with a poor outcome while the outlook was much better in cases of acute disseminated encephalomyelitis (ADEM). Only one lady with PRES had denied her blindness. EEG was abnormal in patients of SSPE, PRES and traumatic occipital gliosis (absence of alpha rhythm) while no abnormality was noted in ADEM. Visual evoked potentials recorded during blindness were abnormal in 6 patients. In a study VEPs have been recorded in patients from cortical blindness and are probably mediated by the extra-geniculocalcarine connections between the optic nerve and the secondary visual cortex of the occipital convexit.[20]
Acute disseminated encephalomyelitis
In ADEM vision loss is classically due to optic neuritis, cortical vision loss is unusual. In our patients the bilateral parieto-occipital white matter lesions that disrupted the visual signals to the primary visual cortex. The prognosis in this group was excellent compared to other causes of cortical blindness in our study.
Posterior reversible leukoencephalopathy syndrome
Even though this is a reversible condition by definition, the persistence of poor vision in our cases is due to infarction of parieto-occipital white matter as indicated by restricted diffusion on diffusion weighted imagin.[8] The cytotoxic edema in PRES has been explained as result of compromised microcirculation secondary to raised interstitial pressure exerted by massive vasogenic edema.[21]
SSPE
The ophthalmic changes are seen in 10-50% cases of SSPE, they are papillitis, papilledema, optic atrophy, macular or peri-macular chorioretinitis, cortical blindness and Anton's syndrome.[21] Presentation with cortical vision loss is considered atypical and is seen commonly when the onset is in adolescence/young adulthood.[22] Our three cases had similar age of onset and cortical vision loss in them was the presenting complaint. The diagnosis was made once the myoclonus appeared after few months.
To conclude, a variety of etiologies of neurogenic vision loss were observed in this study. The majority of patients with neurogenic vision loss had diseases of anterior visual pathway. Among optic neuropathies the most important etiologies were demyelinating diseases and chronic meningitis with elevated intracranial pressure. In the demyelinating group, the characteristics of patients with idiopathic optic neuritis and neuromyelitis optica were similar to that of atypical optic neuritis. On the other hand, all cases of multiple sclerosis behaved like the typical optic neuritis. A large proportion of patients in our study had severe impairment to blindness 78.6% and improvement to acuity 6/18 or better than was noted in only 33.6% of affected eyes, respectively. Patients with severe impairment of vision and late presentation had poor prognostic in this study.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- The clinical profile of optic neuritis. Experience of the optic neuritis treatment trial. Optic Neuritis Study Group. Arch Ophthalmol. 1991;109:1673-8.
- [Google Scholar]
- Profile of optic neuritis in Chandigarh and surrounding areas. Indian J Ophthalmol. 1981;28:195-200.
- [Google Scholar]
- Anterior ischemic optic neuropathy and branch retinal artery occlusion in cavernous sinus thrombosis. J Clin Neuroophthalmol. 1990;10:193-6.
- [Google Scholar]
- Vision impairment in tuberculous meningitis: Predictors and prognosis. J Neurol Sci. 2010;290:27-32.
- [Google Scholar]
- Cerebral venous thrombosis: Update on clinical manifestations, diagnosis and management. Ann Indian Acad Neurol. 2008;11:79-87.
- [Google Scholar]
- International Statistical Classification of Diseases and Health Related Problems, 10th Revision-ICD-10. Geneva: World Health Organization; 1992.
- Catastrophic visual loss due to Cryptococcus neoformans meningitis. Medicine (Baltimore). 1993;72:207-24.
- [Google Scholar]
- Long-term visual outcome in idiopathic intracranial hypertension. Ann Indian Acad Neurol. 2011;14:19-22.
- [Google Scholar]
- Visual outcome of blind eyes in pituitary apoplexy after transsphenoidal surgery: A series of 14 eyes. Surg Neurol. 2005;63:42-6.
- [Google Scholar]
- Predictive factors for the development of visual loss in patients with pituitary macroadenomas and for visual recovery after optic pathway decompression. Can J Ophthalmol. 2010;45:404-8.
- [Google Scholar]
- Intracranial dural metastasis of Ewing's sarcoma: A case report. Korean J Radiol. 2008;9:76-9.
- [Google Scholar]
- CT anatomic measurement of the optic canal and its clinical significance. Zhonghua Er Bi Yan Hou Ke Za Zhi. 2000;35:275-7.
- [Google Scholar]
- Case report: Cervical spinal cord signal changes in a case of adult-onset subacute sclerosing panenchephalitis. Indian J Radiol Imaging. 2010;20:202-4.
- [Google Scholar]
- Visual evoked potentials and postmortem findings in a case of cortical blindness. Ann Neurol. 1977;2:531-4.
- [Google Scholar]
- Posterior leukoencephalopathy without severe hypertension: Utility of diffusion weighted MRI. Neurology. 1998;51:1369-76.
- [Google Scholar]






