Translate this page into:
Migraine and Mood Disorders: Prevalence, Clinical Correlations and Disability
This is an open access journal, and articles are distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 4.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as appropriate credit is given and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Introduction:
Both migraine and mood disorders are prevalent disorders with many studies demonstrating that they are comorbid with each other with increased migraine-related disability in such patients.
Aim:
The aim of the study is to test the hypothesis that mood disorders are comorbid with migraine with increased disability and to identify any clinical features in migraineurs which may be associated with mood disorders.
Materials and Methods:
Patients presenting with complaints of headache to the Neurology Outpatient Department of a Tertiary CARE Hospital from August 01, 2016 to February 28, 2017, were subjected to International Classification of Headache Disorder 3 beta criteria to satisfy a diagnosis of migraine and were assessed in detail as to headache characteristics. Mood disorders were assessed by Hospital Anxiety and Depression Scale and migraine-related disability was assessed by Migraine Disability Assessment Questionnaire. Patients with serious medical complaints, known previous psychiatric disease, other types of headaches and recent prophylactic drug intake were carefully excluded.
Results:
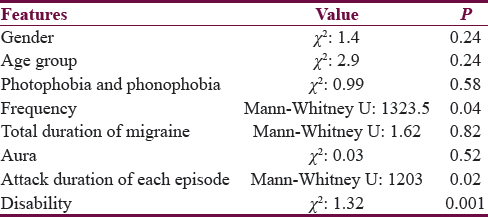
A total of 133 patients were studied. The duration and frequency of migraine headaches were found to correlate with the presence of mood disorders and the migraine-related disability in patients with comorbid mood disorders was significantly higher. Factors such as total duration of migraine, aura, vomiting, phono, and photophobia were not found to be statistically correlated with mood disorders.
Conclusions:
Rates of depression and anxiety in migraine vary widely in various studies due to variations in study criteria, population characteristics and various scales used. We found a prevalence of 16.54% of anxiety and 9.02% of depression in migraineurs, a rate comparable to or less than many studies in international literature and a significantly increased disability in individuals with comorbid mood disorders and migraine. Routinely including questionnaires such as HAD in screening patients with migraine to rule out comorbid mood disorders may be warranted. Because we have carefully excluded all other primary (especially tension and medication overuse headaches) and secondary headaches and selected prophylactic drug naïve patients, we contend that this study provides a clear clinical profile of migraineurs with mood disorders.
Keywords
Comorbidity
meta-analysis
migraine
mood disorders
INTRODUCTION
Migraine is one of the most prevalent disorders in the world. Mood disorders, such as depression and anxiety similarly, have a high prevalence rate across various geographic locations and populations. Comorbidity means the coexistence of any additional ailment in a person with an index disease.[1] It has been definitely established by numerous population and clinical research studies that mood disorders are comorbid with migraine with a frequency more than would be expected by chance.[2] For example, major depression was present in 8.6%–47.9% of individuals with migraine in a meta-analytic study[3] while one study found migraineurs to be 4 or 5 times more likely to suffer from generalized anxiety disorder.[4] These issues are of more than academic interest for the following reasons. One, in diagnosis, as the presence of one disorder, migraine, should prompt the clinician proactively to search for mood disorders and vice versa. Secpndly it helps in the management, as management of both migraine and mood disorders is necwsasay for optimum and quick recovery. For example, the presence of untreated depression has been found to be a risk factor for conversion of low-frequency episodic migraine to chronic migraine.[5] Third, comorbid depression and anxiety also are associated with poorer long-term headache outcomes, higher medical costs, healthcare utilization, and increased headache-related disability.[6] Hence, from a public health perspective, measures to reduce the disability of migraine should include both disorders. Finally, a detailed study of the common epidemiological as well as anatomical and neurochemical associations between the two disorders may well give valuable clues regarding their etiology and pathogenesis. We hypothesized that comorbid mood disorders are more common in migraineurs and that the disability in such patients would be more. The present study was conducted to study the prevalence of mood disorders in migraineurs uncomplicated by other types of headache, to identify any migraine-related clinical features which may be associated with co-morbid mood disorders, and to compare migraine-related disability in patients with and without comorbid mood disorders
MATERIALS AND METHODS
The index cases were obtained from patients attending the Neurology Outpatient of a tertiary care hospital (Government TD Medical College, Alappuzha) during a period from August 01, 2016 to February 28, 2017. The cases were identified to have migraine by International Classification of Headache Disorder 3 beta criteria by the first author (RM). Each patient was evaluated in detail with a questionnaire with details regarding the duration of headache, frequency and duration of each episode, site, quality and severity of pain, auras, migraine accompaniments such as photo or phonophobia, nausea, vomiting as well as triggers. To assess disability, Migraine Disability Assessment Questionnaire (MIDAS) was applied to all patients. The MIDAS is a well-validated method[7] and consists of five questions to be answered by the patient about the impact of migraine headaches in the past 3 months on their personal, professional and social lives as well another section regarding severity and frequency of these headaches. A score of 6 or more is taken as positive with cutoffs for mild, moderate, and severe disability. The presence of concurrent anxiety and mood disorders was assessed by the Hospital Anxiety and Depression Scale (HADS).[8] This consists of 14 items in two subscales, HADS-Anxiety and HADS-Depression, each with 7 items. Each item expresses the subjective experience of the respondent in the preceding week and is rated 0–3, with zero indicating the maximum symptom severity. The sum of each subscale has a potential range from 0 to 21. A score of 11 or more was taken as positive for either anxiety or depression depending on the subscale. Neuro-imaging studies (magnetic resonance imaging) were done in all patients to rule out structural lesions, in addition to blood counts, erythrocyte sedimentation rate, and routine blood biochemistry.
Exclusion criteria were:
-
Presence of other headaches, both secondary and primary, including tension and medication overuse headaches
-
Recent onset of headaches within the past 6 months of study inclusion
-
Recent use of hormonal contraceptives
-
Individuals s with severe medical complaints
-
Individuals previously diagnosed to have psychiatric disease
-
Individuals who had taken prophylactic medicines for migraine within the past 6 months.
RESULTS
A total of 133 patients were studied during the study.
The sample consisted mostly (n = 108, 82%) of middle age (25–50 years) Individuals with mean (standard deviation [SD]) of age of 34.13 (8.49) years. It was a female predominant sample (n = 103, 78%). As per HADS score, among the 12 patients (9.02%) suffering from depressive symptoms, 41.7% (n = 5) had borderline abnormal score and 58.3% (n = 7) had abnormal score whereas among the 22 persons (16.54%) suffering from anxiety 18.2% (n = 4) had borderline score and 81.8% (n = 18) had abnormal score. Mean HADS score (SD) of depression was 11.25 (3.05) while that of anxiety was 13.82 (2.72). Median of duration of headache was 6 years with SD of 6.6 years. Here, duration of disease was not normally distributed, so nonparametric statistics were applied. Though female individuals had more duration of illness (mean rank: 69.88), it was not significantly different (P = 0.05) from males (mean rank: 58.48). Middle-aged individuals suffered more duration of illness than other age groups (P < 0.05). Mean rank of the frequency of headache attacks in case of females was 71.43 (P < 0.05). Thus, females had more frequency of illness. No correlation between gender/age group and frequency of headache attacks was found. 61.4% (n = 81) of individuals had nausea and vomiting. No association with gender or age group with nausea or vomiting was found. 76.5% (n = 101) had photophobia and photophobia. The clinical correlates between migraine and mood disorders are summarized in the appended Table 1. No association was found between mood symptoms and age or gender group with mood changes. 25% (n = 34) of patients suffered from mood changes. No association was found between mood changes and gender or age group. In addition, no association was found between photo and phonophobia symptoms and mood changes. The correlation was found between mood changes and frequency of headache attacks (P = 0.04) which signifies that the more the frequency of migraine headaches the more the chance of having mood symptoms and vice versa. There was no correlation between occurrence/severity of mood changes and total duration of illness. 16% (n = 21) individuals had aura with the migraine episodes. There was no association between aura and mood changes. Median (SD) of the duration of attack (h) was 8 (9.5). The more the attack duration, the more severe were the mood changes (mean rank 80.12), and this was significantly correlated (P = 0.02). Only 15% (n = 20) had menstrual headache and 3% (n = 4) had menstrual mood changes. There was no significant correlation with mood changes and menstrual headaches. Regarding disability, as per MIDAS, 32.8% (n = 43) had no disability, 0.7% (n = 1) had mild disability, 40.3%(n = 53) had moderate disability, and 26.1% (n = 35) had severe disability. A significant association was present between MIDAS score severity with mood changes (P < 0.001) and between severity of the mood changes with severity of disability [Table 1].
DISCUSSION
Migraineurs are 2.5 times more likely to be depressed than those without migraine[910] and 2–5 times more likely to have anxiety disorders.[4] However, various studies have demonstrated highly variable prevalence rates of mood disorders in migraine. For example, the meta-analytic study[3] alluded to above, reported the existence of comorbid major depressive disorder in 8.6%–47.9% of migraineurs. Indeed, a few studies have not found an association between migraine and depression.[11] This is likely due to differences in the inclusion criteria (for example the presence of other type of concurrent headaches), clinicoepidemiological variations between different geographic populations as well as differences between the different scales used to demonstrate psychopathology.
Similarly, many studies have confirmed the comorbidity of migraine and anxiety disorders.[4121314] In fact, the association between migraine and anxiety disorders is even stronger than affective disorders.[15] The majority of migraineurs (51%–58%) will meet criteria for at least one anxiety disorder during their lifetimes.[16] Generalized anxiety disorders and social phobia were the most commonest anxiety disorders associated with migraine. Many epidemiological studies indicate that anxiety disorders are nearly twice as common among migraineurs as is depression.[161718] Several authors have proposed that the onset of anxiety disorders precedes migraine which in turn precedes depression onset.[3]
Analysis of data obtained from our study confirms our hypothesis. 16.54% of the study population had anxiety, and 9.02% had depressive symptoms. Mood disorders occur more commonly in migraine than would be expected by chance and the disability in these patients is significantly more than in individuals without mood disorders. We have carefully excluded cases with other types of headaches especially tension-type headaches and analgesic overuse headaches. This is of vital importance as tension-type headaches are independently strongly associated with depression[1920] while analgesic dependent headaches can significantly worsen disability in migraineurs. Hence, we have also carefully excluded individuals on prophylactic migraine medicines. This is to nullify the effect of commonly used prophylactic medicines such as beta-blockers, flunarizine, and topiramate which can cause adverse mood reactions such as depression and cognitive slowing. The HADS score was selected as it is a well-validated, convenient and suitable to application in an outpatient department setting as well as the fact that it emphasizes the subjective manifestations of anxiety and depression and does not include any questions regarding somatic or pain symptoms which may paradoxically include headache as well.
The figures obtained by us are comparable to the rates of 19% and 7% of comorbid anxiety and depression in migraineurs found in the Eurolight project.[21] The Eurolight project was a large cross-sectional headache survey sampling from the adult populations of 10 European Union countries. Several questionnaires were utilized including HADS to assess disability and the presence of associated mood disorders. An important finding in this study was that comorbid psychiatric disorders when present, adds significantly to migraine-related disability and if not identified and properly treated leads to unsuccessful headache management. The authors suggested that in view of the significant morbidity due to mood disorders associated with migraine, there is a case for screening migraine patients with HADS even in primary care settings where time is ata premium.
The relationship between mood disorders and migraine could be multi-factorial. For example, depressive symptoms and anxiety could emerge after recurrent headache episodes or by themselves they could be risk factors for migraine, and finally, they could be associated with some other (confounding) factor which drives the headache.[22] This has led to the question whether this relationship is unidirectional or bidirectional and if so in which direction. A population-based study from the United States demonstrated that chronic migraine sufferers were much more likely to have depression or anxiety.[23] while Ashina et al.[24] studied patients enrolled in the American Migraine Prevalence and Prevention study and found that depression had a significant effect in the evolution of chronic headache and that there was a depression-dose relationship in that patients with moderate and severe depression were more at risk than those with mild depression after adjusting for confounding factors. In fact, depression is considered the most important risk factor of migraine.[5] However, other studies have suggested a bidirectional relation between migraine and depression, namely, the presence of one increasing the risk of the other.[2526] In our patients’ duration and frequency of headache, attacks were found to be associated with the occurrence of mood disorders. In this regard, some studies[1626] have found a correlation between the frequency of headaches and occurrence of mood disorders in migraine. Indeed, Baldacci et al.[16] have postulated an interesting template for the etiopathology of comorbid mood disorders based on this. They hypothesized that a combination of increased time of headache attacks with increased sensory sensitivity in migraineurs which persists at a lower level in between the attacks is associated with mood disorders. Hence, in migraine, there is dysmodulation of normal sensory processing leading to a state of cortical hyperexcitability for both inherited and acquired causes. They postulate that this hypersensitivity is more pronounced in migraineurs with mood disorders and provide evidence from their study the facts that cutaneous allodynia during headache and higher susceptibility to trigger factors are present more commonly in their individuals with mood disorders. Another putative model for etiology of comorbid mood disorders is from the so-called neuro-limbic model of migraine in which there is an altered functional connectivity between the brainstem modulating circuits and the limbic centers.[27] During the process of central sensitization, there is a simultaneous activation of pain modulating pathways originating in the periaqueductal grey and rostroventral medulla which communicate with higher cortical and subcortical centers such as amygdala and anterior cingulate cortex[28] which process the unpleasant and distressing aspects of pain with descending connections to the serotoninergic raphe and brainstem adrenergic nuclei. Neuro-imaging studies have shown that mood and anxiety disorders share several anatomical and functional areas (amygdala, anterior cingulate, and periaqueductal gray) in common with migraine suggesting a common matrix.[1629]
Numerous studies have shown a poorer quality of life with restriction of activities, job absenteeism, more use of health services and more likely to require help with personal or instrumental activities of daily living in migraneurs with mood disorders similar to the results showing worse disability scores in our study.[123031] Studies from India are scarce, but Sharma et al.[32] have found using a case–control study on 71 consecutively diagnosed migraine patients that the health-related quality of life was significantly impaired in the migraine patients. The authors used Short Form-36 (SF-36) and MIDAS scale to assess disability. They also found that worse depressive and anxiety symptoms predicted increased disability as manifested by worse Mental Component Summary scores in the SF-36.
We would like to acknowledge the limitations of our study. Assessment of causality aspects of mood disorders in migraine is made best in longitudinal population based rather than hospital based cross sectional studies like the present one. Moreover, the latter are subject to the so-called Berkson's bias due to the fact that those individuals with more severe disease are more likely to seek help and also due to methodological artifacts.[3334] A case–control study utilizing appropriate age- and sex-matched controls would have been ideal in confirming whether the prevalence of mood disorders in migraineurs are higher than the general population in the geographical area. Similarly, the HADS though well validated is a screening rather than diagnostic instrument with a tendency to underestimate the prevalence of anxiety and depression.[35] Hence, the actual prevalence of mood disorders in our cohorts may well have been higher. Moreover, the relatively small sample size of individuals with both mood disorders and migraine may have caused some of the causative factors not to develop enough statistical strength to produce statistical relevance. This might explain why features such as migraine aura and vegetative symptoms such as nausea and vomiting were found not to be correlated with mood changes in our study. However, the unique point about our study is that we have carefully excluded other causes of headache especially tension type and medication overuse headaches which could potentially change the clinical and psychological picture of the individuals. Moreover, we have taken care to include only recent prophylactic drug naïve patients. Hence, we contend that this study provides a pure and undistorted clinical picture of mood disorders in migraineurs in our study population.
CONCLUSIONS
This study has revealed that mood disorders are comorbid with migraine at a rate comparable to or less than that described in many studies in international literature and the occurrence of comorbid mood disorders significantly contributes to migraine associated disability. Hence, routinely including questionnaires such as HADS in screening all patients with migraine may be warranted. No definite clinical features in migraineurs are associated specifically with mood disorders except duration and frequency of headache attacks which may indicate that possible prolonged trigeminovascular activation could in some way be associated with the occurrence of mood disorders in migraine.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23:455-68.
- [Google Scholar]
- Migraine and psychiatric comorbidity: A review of clinical findings. J Headache Pain. 2011;12:115-25.
- [Google Scholar]
- Chronic migraine: Risk factors, mechanisms and treatment. Nat Rev Neurol. 2016;12:455-64.
- [Google Scholar]
- Headache chronification: Screening and behavioral management of comorbid depressive and anxiety disorders. Headache. 2008;48:45-50.
- [Google Scholar]
- Development and testing of the migraine disability assessment (MIDAS) questionnaire to assess headache-related disability. Neurology. 2001;56:S20-8.
- [Google Scholar]
- Migraine, quality of life, and depression: A population-based case-control study. Neurology. 2000;55:629-35.
- [Google Scholar]
- Depression and anxiety disorders associated with headache frequency. The Nord-Trøndelag health study. Eur J Neurol. 2003;10:147-52.
- [Google Scholar]
- Migraine, physical health and psychiatric disorder: A prospective epidemiologic study in young adults. J Psychiatr Res. 1993;27:211-21.
- [Google Scholar]
- Migraine with and without aura: Association with depression and anxiety disorder in a population-based study. The HUNT study. Cephalalgia. 2006;26:1-6.
- [Google Scholar]
- Migraine and psychopathology. Results of the Zurich cohort study of young adults. Arch Gen Psychiatry. 1990;47:849-53.
- [Google Scholar]
- Migraine features in migraineurs with and without anxiety-depression symptoms: A hospital-based study. Clin Neurol Neurosurg. 2015;132:74-8.
- [Google Scholar]
- Panic disorder and migraine: Comorbidity, mechanisms, and clinical implications. Headache. 2013;53:23-45.
- [Google Scholar]
- The role of stressful life events in the persistence of primary headache: Major events vs.daily hassles. Pain. 1992;51:35-42.
- [Google Scholar]
- Personality traits and psychological reactions to mental stress of female migraine patients. Cephalalgia. 1999;19:566-74.
- [Google Scholar]
- Headache, depression and anxiety: Associations in the Eurolight project. J Headache Pain. 2016;17:59.
- [Google Scholar]
- From episodic to chronic migraine In “The migraine brain Vol 1.”. In: Borsook D, May A, Goadsby PJ, Hargreaves R, eds. The Migraine Brain-Imaging Structure and Function. Vol 1. Oxford University Press, University of OXford; 2012. p. :69.
- [Google Scholar]
- Sociodemographic and comorbidity profiles of chronic migraine and episodic migraine sufferers. J Neurol Neurosurg Psychiatry. 2010;81:428-32.
- [Google Scholar]
- Depression and risk of transformation of episodic to chronic migraine. J Headache Pain. 2012;13:615-24.
- [Google Scholar]
- Comorbidity of migraine and depression: Investigating potential etiology and prognosis. Neurology. 2003;60:1308-12.
- [Google Scholar]
- Clinical course in migraine: Conceptualizing migraine transformation. Neurology. 2008;71:848-55.
- [Google Scholar]
- Structural and functional neuroimaging in migraine: Insights from 3 decades of research. Headache. 2013;53:46-66.
- [Google Scholar]
- Projections of neurons in the periaqueductal gray to pontine and medullary catecholamine cell groups involved in the modulation of nociception. J Comp Neurol. 1999;405:359-79.
- [Google Scholar]
- Beyond neurovascular: Migraine as a dysfunctional neurolimbic pain network. Headache. 2012;52:1553-65.
- [Google Scholar]
- The prevalence and impact of migraine headache in bipolar disorder: Results from the Canadian community health survey. Headache. 2006;46:973-82.
- [Google Scholar]
- Comorbidity of migraine and psychiatric disorders – a national population-based study. Headache. 2008;48:501-16.
- [Google Scholar]
- Quality of life and psychiatric comorbidity in Indian migraine patients: A headache clinic sample. Neurol India. 2013;61:355-9.
- [Google Scholar]
- Psychiatric comorbidities of episodic and chronic migraine. J Neurol. 2013;260:1960-9.
- [Google Scholar]
- The global prevalence of common mental disorders: A systematic review and meta-analysis 1980-2013. Int J Epidemiol. 2014;43:476-93.
- [Google Scholar]






