Translate this page into:
Metastatic sacrococcygeal yolk sac tumor: A misleading diagnosis
Address for correspondence: Dr. Atef Ben Nsir, Department of Neurological Surgery, Fattouma Bourguiba University Hospital, Monastir, Tunisia. E-mail: atefbn@hotmail.fr
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Sacrococcygeal yolk sac tumor (YST) is an extremely rare malignant extra-gonadal germ-cell tumor, which usually succeeds to the degeneration of more common benign teratoma. We describe here an unprecedented case of conus medullaris compression by a spinal metastasis from a pure sacrococcygeal YST in a 1½ years old girl, which was misdiagnosed initially as an anal fissure and stress the need of a meticulous clinical examination and further screening in young patients presenting with sphincter disturbances.
Keywords
Conus medullaris compression
extra-gonadal yolk sac tumor
prognosis
sacrococcygeal tumor
Introduction
Yolk sac tumor (YST) also known as endodermal sinus tumor or Teilum Tumor is a highly malignant and extremely rare germ cell tumor (GCT) that primarily occurs in the testis or ovary of young patients.[1] Its annual incidence has been estimated as <1/million/year[2] and 2–5% of these cases may arise in a variety of extra-gonadal sites that mostly display an axial distribution pattern.[3]
In the sacrococcygeal region, however, these tumors usually appear as a consequence of the degeneration of more common benign teratoma.[3]
To the best of our knowledge, a pure YST of the sacrococcygeal region in a 1½ years old girl presenting in the metastatic stage with signs of conus medullaris compression has never been previously reported.
The case is presented, and the literature is reviewed.
Case Report
An 18-month-old girl presented to the pediatric department of our institution in Mars 2014 for a 2 weeks history of constipation. Her medical history was consistent for normal gestation, no prior medication, and no prior surgery. Physical examination at that time found an anal fissure at 9.00 h, and the patient was treated medically with partial improvement.
Two months later, she presented to our emergencies with brutal onset of conus medullaris compression syndrome made of bilateral weakness in her both lower limbs, urinary retention and fecal incontinence.
On admission the patient's general status was altered and the neurological examination confirmed the functional sings with a symmetric and predominantly proximal paraplegia associated to bilateral sensory dissociation, perianal numbness, urinary retention and an atonic anal sphincter. The physical examination, notably involving detailed clinical examination of the trunk and the extremities found an indolent and endured 5 cm × 6 cm sacrococcygeal mass with abdominal bloating.
Magnetic resonance imaging (MRI) showed a 13 cm × 7 cm × 6 cm irregular and lobulated sacrococcygeal junction tumor with a large anterior pelvic expansion and tumoral invasion of T12, L1, and L2 vertebral bodies. A posterior extradural location at the level of L1 was responsible of a major conus medullaris compression [Figure 1]. Pulmonary and mediastinal secondary locations were also discovered as long as major bladder and urinary tract dilation causing hydronephrosis.
![T2-weighted magnetic resonance imaging in axial (a), sagittal (b) and coronal (c) views showing a huge tumor mass arising from the sacrococcygeal junction; occupying the pelvis, and reaching the subcutaneous tissue (the associated epidural metastatic location at the level of L1 causing important thecal sac compression [arrow])](/content/150/2015/6/3/img/JNRP-6-395-g001.png)
- T2-weighted magnetic resonance imaging in axial (a), sagittal (b) and coronal (c) views showing a huge tumor mass arising from the sacrococcygeal junction; occupying the pelvis, and reaching the subcutaneous tissue (the associated epidural metastatic location at the level of L1 causing important thecal sac compression [arrow])
Surgery was advised in emergency, and the patient was immediately transferred to the operative theater where A T12-L2 laminoplasty aiming for conus medullaris decompression and histological diagnosis was realized. During the surgery, the lesion was reddish grey and prone to bleeding. Meticulous dissection allowed for complete removal of the epidural portion.
Postoperative laboratory screening showed very high levels of alpha fetoprotein (AFP) at 1202 ng/ml (normal range: 0–10 ng/ml); β-human chorionic gonadotropin levels were within the normal range.
Histological analyses were realized on multiple tissue samples and showed flat or cuboidal tumor cells arranged in typical Schiller-duval bodies composed of a single layer of tumor cells surrounding papillary structures with central vessels [Figure 2]. Hyalinized areas were also present, and some myxomatous material was found adjacent to the vessels. The MIB-1 index was 23%, and immunohistochemical staining was strongly positive for AFP and negative for CD 30. A small localized positivity for placental alkaline phosphatase was also observed, and the final histological diagnosis was a pure YST.
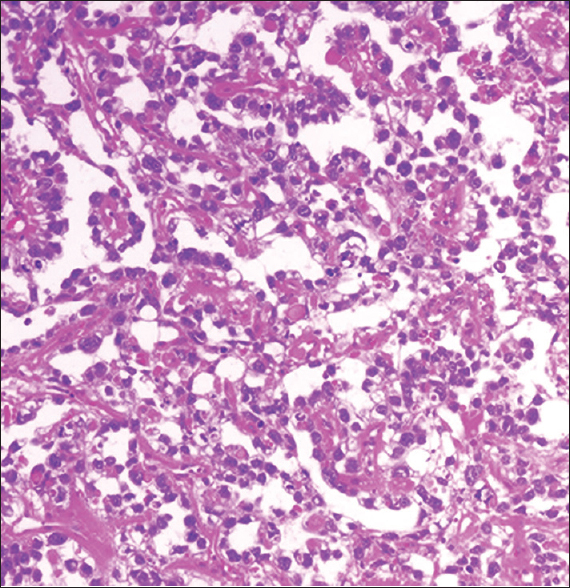
- Photomicrograph of the tumor specimen showing typical features of yolk sac tumor with Schiller–Duval bodies (H and E, original magnification ×100)
Adjuvant cisplatin-based high dose chemotherapy was administered, and the patient was enrolled under an intensive care and rehabilitation program. Her condition barely improved namely for the motor weakness, and AFP levels decreased to normal limits within 1-month of intensive chemotherapy.
The patient's status remained unchanged till the most recent follow-up examination, 5 months after surgery.
Discussion
In 1976, Brown hypothesized that germ cells in the developing embryo arise in the yolk sac, migrate around the hinder end of the primitive gut to the genital ridge on the posterior abdominal wall, and are finally absorbed into the developing gonads.[4]
It is suggested that during this migration, some germ cells may get left behind or stay too far and rest at various sites along the dorsal wall of the embryo near the midline. The primordial germ cells give rise to an undifferentiated germ cell line. The undifferentiated germ cells undergo differentiation into embryonic or extra-embryonic cells like YST cells.[3]
Malignant GCT account for about 3% of neoplasms in children, and YST is the most common histological subtype with a high degree of malignancy.[5]
The majority of pediatric sacrococcygeal tumors are benign teratomas.[6] These tumors, however, have the potential for malignant degeneration and malignancy is usually limited to a single element, a YST.[3] In fact, reports of primary and pure YST of the sacrococcygeal region are extremely scarce with only 18 cases already reported in the literature.[3456]
Sacrococcygeal YST develops exclusively in children <3 years of age[456] with complaints of constipation or buttock swelling[5] and since it usually shows high malignancy; the duration from the onset of symptoms to the admission is always short and metastasis may already exist at the time of the patient's admission, primarily pulmonary.[5]
A primary pure YST of the sacrococcygeal region presenting in the metastatic stage with a conus medullaris compression due to spinal metastasis has never been previously reported.
In fact, Colak et al. in 1991[7] and Lee et al.[8] in 2002 reported the two single literature cases of spinal cord compression due to spinal metastases of YST, but in these two reports the primary tumor was the testis.
What is more interesting in our case is that the tumor initially caused constipation and the combination of the presence of an anal fissure with a remarkable normal physical examination at that time resulted in a 2 months diagnostic delay with consequent general status aggravation and neurologic compromise; which stresses the need for a meticulous clinical examination and further investigation of young patients presenting with vague symptoms like constipation.
The computed tomography and MRI are the preferred radiological examinations in the diagnosis of these tumors. Each child with a sacrococcygeal GCT should also be studied for AFP. Its determination is useful in the diagnosis, to monitor the results of therapy and detect metastases and recurrence after therapy. The production and release of AFP is not limited to YSTs but an extremely high AFP level may be a clue for making the diagnosis of YST, which was observed in the present case.
Unlike their intracranial counterparts, no consensus regarding the treatment of primary spinal GCT has been achieved.
Their management can become a challenge depending on their location; and because patients exclusively present with clinical findings related to spinal cord or nerve root compression and it is often impossible to distinguish between GCT and other spinal tumors on imaging; the first aim should be the preservation of the neurologic function and the second the observation of the histologic specimen.
Traditionally, the treatment of YST causing spinal cord compression has been laminectomy with or without radiation, followed-up by chemotherapy.[19]
Pashankar et al. in 2001,[9] successfully treated a spinal cord compression due to an epidural extension of a para-spinal YST using chemotherapy only. However, such an approach is not suitable in emergency cases like ours presenting with acute onset of conus medullaris compression syndrome.
Chemotherapy has greatly improved the survival of patients with YST as the combination of modern surgical treatment and adjuvant cisplatin-based chemotherapy leads to a 5-year survival rate as high as 90% in children with gonadal YST; however, the prognosis differs considerably in spinal cases as these tumors may be unresectable and still remains poor if there is metastasis.[10]
The place of radiation therapy in the therapeutic arsenal of YST still needs to be assessed, and we believe that it should be avoided in young patients due to its serious side effects.
Finally, the degree of AFP elevation has also been shown to correlate with prognosis and levels <1000 ng/mL are in the good prognostic category. Although our patient responded remarkably to chemotherapy with a rapid normalization of her AFP serum levels, it appears reasonable in our case to expect tumor progression early.
Conclusion
A pure YST of the sacrococcygeal region can present in the metastatic stage with brutal onset of conus medullaris compression syndrome.
The diagnostic delay observed in the present case and its hazardous consequences are of great value for reminding physicians to be aware of the diagnosis of YST when a child presents with constipation especially if there is an anal fissure; which underscores the need of a meticulous clinical examination and further investigation.
As the management guidelines are still pending, we believe that rapid neural decompression associated to platin-based chemotherapy can be actually considered as preferential management policy.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Primary endodermal sinus tumor presenting with spinal cord compression. Case report. J Neurosurg. 1997;86:151-3.
- [Google Scholar]
- Sacrococcygeal yolk sac tumor presenting as subcutaneous fluid collection initially treated as abscess. South Med J. 2010;103:1068-70.
- [Google Scholar]
- Epidural metastasis of testicular yolk sac tumor: An unusual cause of spinal cord compression. Case report. Pediatr Neurosurg. 1991;17:139-41.
- [Google Scholar]
- Metastatic spinal cord compression of testicular yolk sac tumor. Childs Nerv Syst. 2002;18:171-4.
- [Google Scholar]
- Successful chemotherapeutic decompression of primary endodermal sinus tumor presenting with severe spinal cord compression. J Pediatr Hematol Oncol. 2001;23:170-3.
- [Google Scholar]
- Extragonadal and pediatric germ cell tumors. Hematol Oncol Clin North Am. 1991;5:1189-209.
- [Google Scholar]






