Translate this page into:
Mental Health Orientation for Self-Help Group Members: A Feasibility Study
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Treatment gap for mental health care in low- and middle-income (LAMI) countries is very large, and building workforce using the locally available resources is very much essential in reducing this gap. The current study is a preliminary work toward this direction.
Materials and Methods:
A single group pre- and post-design was considered for assessing the feasibility of Mental Health Orientation (MHO) Program for Self-Help Group members. Assessment of participants’ MHO using Orientation Towards Mental Illness (OMI) scale was undertaken at three levels: Baseline assessment before the intervention, after completing 2 days orientation program, and 6 weeks later.
Results:
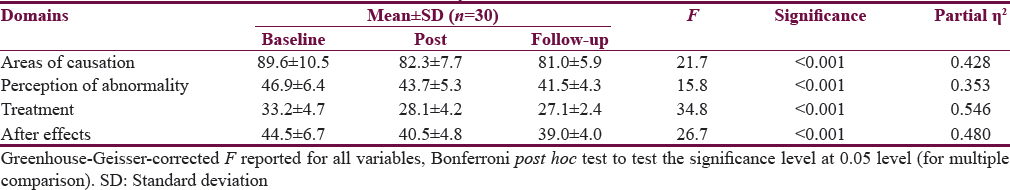
Analysis of data resulted in statistically significant mean scores in the domains of areas of causation (F[1.41, 40.7] = 21.7, P < 0.000, ηp2 = 0.428), perception of abnormality (F[1.27, 36.8] = 15.8, P < 0.000, ηp2 = 0.353), treatment (F[1.42, 41.3] = 34.8, P < 0.000, ηp2 = 0.546), and after effect (F[1.36,39.4] = 26.7, P < 0.000, ηp2 = 0.480). Although the overall mean scores of all the domains of OMI were found to be statistically significantly different, there was no significant difference in the mean scores between post and follow-up assessments on areas of causation (μd = 1.27, P = 0.440) and treatment (μd = 1.00, P = 0.156).
Conclusion:
Overall, the findings of our study demonstrate that brief MHO program can exert a beneficial effect on bringing about significant change in the orientation of the participants toward mental illness but need to be refreshed over time to make the impact of the program stay longer.
Keywords
Mental health
orientation
self-help group
training
INTRODUCTION
Mental health is a crucial aspect which greatly influences the overall well-being of individuals in particular and communities in large. Despite this, a holistic approach toward health is lacking and unlike the physical health, mental health has been largely ignored. As a result, only a small minority of the affected people receive the most basic treatment with treatment gap in low- and middle-income (LAMI) countries scoring as high as 90%.[12345] To meet the current and future needs toward bridging the treatment gap, the quality and quantity of mental health resources needs to be improved.[6]
Often, poor knowledge, negative attitude, and pervasive stigma toward mental illness prevailing within the community, grossly inadequate budgets for health care including mental health, and acute shortage of trained mental health personnel in the developing countries have resulted in neglect of mental disorders thus preventing people with mental illness and their families from seeking appropriate help.[78] In developing countries such as India, the lack of accessibility to mental health services and the nonavailability of professional mental health workers widely exist in peripheral areas. Considering this, the need for decentralization of the services and integrating it with the existing system of general health services has been emphasized in the National Mental Health Program (NMHP).[9] To accomplish the objectives of NMHP, participation of the community is absolutely necessary. It is also important to utilize the indigenous resources to help the beneficiaries to have a longer sustenance and easy accessibility.
Innovative solutions in community-based mental health care making the best use of the indigenous conditions are warranted considering the fact that existing large-size urban-centered institutions being the source of stigma, delay in seeking help, and prevailing treatment gap. Local community resources which are increasingly being recognized as a valuable part of the health system should also be appreciated in the medical model of care. Culture and traditional care, family and community structures need to be acknowledged as important elements in mental health care.[1011] In fact, the crucial role played by the family and community in the success or failures of any community mental health program (CMHP) was highlighted in a follow-up study conducted after 16 years of initiation of CMHP by Schizophrenia Research Foundation Chennai, South India.[12] Hence, without any doubt, successful management of mental illness in the community relies significantly on an informal network of caregivers.[13]
Mental health training programs were conducted for community health workers and doctors providing primary health care in India. Such studies used case vignettes to identify the signs and symptoms of psychiatric illness, relevant questionnaires to assess the knowledge, attitude, and perceived competence in providing mental health care. These studies demonstrated the potential to be an effective way to improve some aspects of mental health literacy and required skill building training programs for integrating mental health into primary health care.[1415] Similar study has been conducted among the members of the Chinese community in Melbourne, to investigate the impact of mental health first aid (MHFA) training on knowledge about mental disorders and on attitudes to people with mental illness using pre-post design. The MHFA training course resulted in a significant positive change in the level of mental health literacy and reductions in stigmatizing attitudes.[16]
Self-Help Groups (SHGs) are novel and innovative organizational set up in India for the upliftment and welfare of people from rural background and especially for women who are mostly invisible in the social structure. These are basically small informal groups, characterized by voluntary memberships, a democratic and consultative structure of governance, economic participation of members, autonomy, education and training, and concerns for the poor. The SHGs are increasingly accepted as a vehicle to reach the underprivileged sections of the society as group becomes the basis for any action and change. These groups enable them to come together for common objective and gain strength from each other to deal with several problems they are facing on day-to-day basis.[1718]
As mentioned earlier, there is a considerable lack of trained workforce in the field of mental health in India. Despite some studies conducted pertaining to mental health literacy or orientation programs for community health workers and primary health care physicians, etc., as part of capacity building programs in mental health, there is an apparent dearth of literature on such programs initiated for SHGs formed primarily for economic reason and other than those SHGs initiated and directed by people with mental illness or their family members. Hence, in this direction, the current study attempts to answer a very basic question: Is it feasible to orient such SHG members to mental health problems through an educational intervention program?
MATERIALS AND METHODS
Research design
The study considered single group pre- and post-design for assessing the feasibility of Mental Health Orientation (MHO) Program for SHG members. Assessment of participants’ MHO was undertaken at three levels. Baseline assessment was done before the intervention, followed by the intervention given over a period of 2 days. Post intervention assessments were carried out at the completion of the program and 6 weeks later.
Setting
Shri Kshetra Dharmasthala Rural Development Project (SKDRDP) is a charitable trust promoted by Dr. D. Veerendra Heggade, trustee of a renowned temple, Shri Kshetra Dharmasthala in the region of Dakshina Kannada district. The SKDRDP with its mission of sustainable inclusive rural development of poor and marginalized sections of society with special focus on empowerment of rural women has a wide array of programs encompassing all aspects of enriching the rural life such as financial, social, and intellectual upliftment of the people. For this, they organize SHGs on the lines of Joint Liability Groups of Bangladesh and provide infrastructure and finance through microcredit for the rural people. It is active throughout the state with its community development programs. During the financial year 2015–2016, SKDRDP has extended its area of operation to cover Karnataka fully with 3,32,000 active SHGs having total membership of 35,57,300.[19]
Participants
The participants were selected randomly, using lottery method from the Pandeshwara Federation of SHGs of Udupi district under SKDRDP, Karnataka, India. This Federation is having 17 SHGs with an approximate of 10–12 members in each group. Although the majority of the groups are with females, there are few groups with only male members. A total of 30 SHG members, aged above 18 years, being able to read and write the local vernacular language Kannada consented to be the participants for the study.
Ethical considerations
Formal permission from concerned authorities was obtained before approaching the participants. After explaining about the study, the written consent from the participants was taken. The participants had the option to opt out of the study at any time and confidentiality was ensured.
The intervention
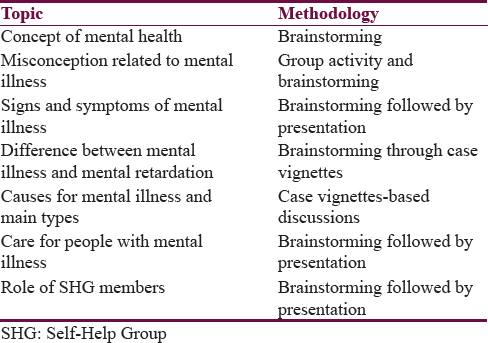
The 2-day MHO program aimed at assessing the feasibility of orienting SHG members toward mental health and illness. It was not intended as an in-depth training program but rather as an introduction on mental health to SHG members who never formally exposed to any such program. The design and content of the MHO program was informed by literature review conducted before the study, researchers’ experience in the field, and the needs of the target population generated through informal discussions. The content of 2-day program included understanding the concept of mental health, myths, misconception, general signs and symptoms of mental illness, caring mentally ill, and the role of SHG members [Table 1]. Participatory methodologies such as case vignettes-based discussion and group activities were adopted.
Instruments
Sociodemographic questionnaire
The sociodemographic questionnaire was prepared to elicit basic information regarding the personal, family, and sociodemographic details of participants. It had the details pertaining to age, gender, education, marital status, religion, occupation, and duration of the membership.
Orientation towards mental illness scale
The tool developed by Prabhu et al.[20] initially a 95-item scale aims at measuring the individual's degree of unfavorable orientation to mental illness. Here, we used modified version of this scale consisting of 67 items, which was equivalent to the original one in all respects and the score range falls between 67 and 335. The tool has been used extensively in research within the Indian context. The alpha coefficient of the Orientation Towards Mental Illness (OMI) in the present study is 0.93 indicating adequate reliability. It taps various aspects of orientation to mental illness providing scores on 13 factors, subsumed under 4 domains. The respondents are required to indicate the degree of his or her agreement or disagreement on a five-point Likert scale ranging from disagree (1) to completely agree (5). The scores of each item are summated and a total score on each factor is obtained; the higher total score indicating more unfavorable the orientation. There are no cutoff scores given by the author to decide on favorable or unfavorable OMI. Hence, it was decided based on the hypothetical mean which was calculated by adding the maximum scores that the respondent can get on a scale to the minimum scores divided by two.
Data analysis
Statistical data management and analyses of the data were carried out using Statistical Package for Social Sciences (SPSS) version 22 for Windows (IBM Corp; Armonk, New York, USA). Descriptive statistics such as frequency and percentage were used to explain the sociodemographic details of the participants. The domain-wise scores were analyzed using mean and standard deviation. As our data violated, the assumption of sphericity, repeated-measures analysis of variance (ANOVA) with a Greenhouse–Geisser correction was used to understand the diffeferences existed in four domains of the OMI scale over three time points: Baseline, immediately after the intervention, and at 6 weeks’ follow-up. Further, tests of within subjects were performed using Bonferroni post hoc test to understand the significance level (at 0.05 level) for diffeferences between the individual time points on the same domains.
RESULTS
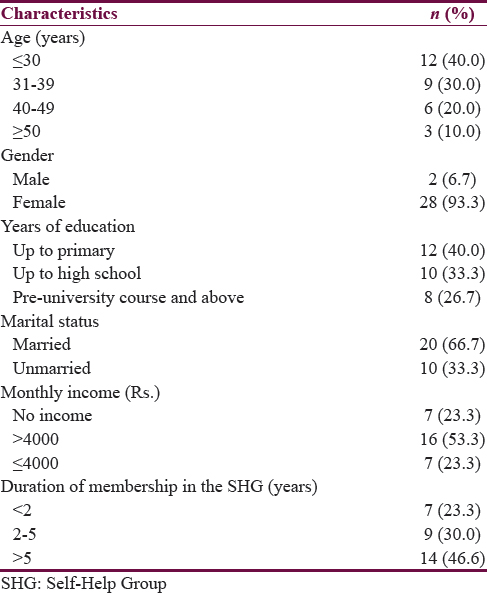
Table 2 provides the sociodemographic profile of the participants. The sample for the current study comprised 30 SHG members. Majority of the members participated in the study were below the age of 40 (n = 21), belonging to female gender (n = 28; 93.3%), studied up to high school education (n = 22; 73.3%). Among them, two-third (n = 20; 66.7%) were married. In the category of income, about 23.3% of them were not having any monthly income as they constituted the group of “not working” or “homemaker”. Among them, 16 of the participants were earning <4000/month and 7 of them earning more than 4000 on monthly basis. In terms of duration of membership in years, around 46.6% of the participants were members of the SHG for more than 5 years, 9 of them were in the criteria of 2–5 years duration of SHG membership, and 7 of them were members for <2 years.
Analysis of data on repeated-measures ANOVA resulted in statistically significant mean scores in the domains of areas of causation (F[1.41, 40.7] = 21.7, P < 0.000, ηp2 = 0.428), perception of abnormality (F[1.27, 36.8] = 15.8, P < 0.000, ηp2 = 0.353), treatment (F[1.42, 41.3] = 34.8, P < 0.000, ηp2 = 0.546), and after effect (F[1.36,39.4] =26.7, P < 0.000, ηp2 = 0.480). Although the overall mean scores of all the domains of OMI were found to be statistically significantly different, there was no significant difference in the mean scores between post and follow-up assessments on areas of causation (μd = 1.27, P = 0.440) and treatment (μd = 1.00, P = 0.156). The same has been depicted in Table 3.
DISCUSSION
Quality mental health care relies on sufficiently trained professionals rather than advanced technology or equipment. One well-established barrier to scaling up of mental health services in most LAMI countries is the inadequate number of people who are trained to provide care and these inadequacies are likely to persist in the years to come.[421] Situation is no better in India when it comes to the scarcity of trained mental health professionals. This warrants for more action needed to ensure that nonprofessional community members take part in mental health programming. If nonprofessionals have to be successfully integrated into mental health programming, they need to acquire relevant knowledge and skills to recognize, refer, and support people experiencing mental health disorders. In this direction, as a preliminary step, the current study aimed to shed some light on the understanding/orientation of the SHG members on mental health and illness and the feasibility of orienting them through 2 days MHO program on the same area. For this purpose, a 2-day training program was organized for the SHG members covering varied aspects of mental health and illness from understanding mental health to caring mentally ill.
Overall, the findings of our study demonstrate that brief MHO program can exert a beneficial effect on bringing about significant change in the orientation of the participants toward mental illness which supports our study hypothesis. These findings related to bringing changes in the orientation of the participants are in consonance with previous reports demonstrating impact of educational campaigns, trainings, and orientation programs in bringing about substantial changes in the mental health knowledge, bringing down rejecting attitudes toward mentally ill, and encouraging social contact with persons affected with mental illness[222324] and maintaining the same over a period of time.[25]
These results are even more interesting and significant in the background that the mean score of the total participants (214.24 ± 37.9) on OMI scale at the baseline was above the cutoff score (201), indicating as a whole they were unfavorable in their OMI. These might be attributed to the lack of mental health initiatives in the place where the study was carried out and mental health issues not being given due importance like other economic empowerment or developmental activities of the SHGs.
However, though we got statistically significant difference in the overall MHO of the participants across time and in the domains of area of causation and treatment of mental illness of the OMI scale, there was no significant mean score difference between the post and follow-up assessment. Such a finding in the study can be attributed to the fact that these two domains of the scale basically deal with causation and management of mental illness which are largely likely to get influenced by the locally held beliefs of the participants about the same. Previous studies on explanatory models of mental illness among community health workers from Southern India also support this finding, which reveal that people seem to hold diverse and contradictory beliefs simultaneously which might be directly contradicting the biomedical model despite working in the health sector. The need to elicit and discuss such beliefs before providing an alternative biomedical was highlighted.[2627]
The limitations of this study need to be acknowledged. Some of the limitations of our study were the absence of control group limiting the power of evidence regarding the program's effectiveness though there were no obvious reasons to change the orientation of the participants over time significantly without having had the program. Along with control group, having a long-term follow-up assessment would have been helped know the retention of knowledge or changes in the attitude over longer period of time. Even an increase in the social desirable response following the program cannot be ruled out. Despite these limitations, the study has few things into its credit. To the best of our knowledge, this is the first study looking at the impact of MHO program on members of SHGs formed primarily for the purpose of economic empowerment. Although there were some studies carried out earlier on SHG members, the purpose of them coming together and forming such group was different (some of the reasons being the support group for people with mental health issues or for the caregivers of persons with mental illness) and the main objective of those studies was to see how exactly being in such groups has an influence on the mental health outcomes of its members.[2829] Participants for the study were recruited randomly which avoided the selection bias in the study. Along with the changes seen in the OMI soon after intervention, retention of the received knowledge over a period of time was assessed over 6 weeks of time. Another highlight of the study was that there was no drop out of participants at any point of assessment. The intervention program used participatory methodologies such as using audio-visual aids and case vignette-based discussions.
Implications
The current study limits its purview to assess the feasibility of training and bringing change in their MHO rather than investigating and evaluating how participants used their acquired knowledge. The evidence from this study clearly indicated that it is possible to change the orientation of people toward mental illness through educative programs. However, it is worth evaluating the actual impact of orientation program on participants in terms of identifying the mentally ill and referring them appropriately. This kind of educative approaches should be scaled up to a larger level rather than limiting to participants from small geographical area and such an attempt should be evaluated over time for the substantial changes it had brought about in the attitudes and behaviors of the participants.
CONCLUSION
The utility of the program in terms of better orientation was very evident though we have not assessed the kind of change which program had brought in referral system. Despite the existence of cost-effective interventions in mental health care, vast gap between the need for and availability of workforce to address psychiatric conditions acts as a major barrier in closing the treatment gap, particularly in the LAMI countries among many other reasons. The result of this preliminary work strongly advocates for the use of locally available resources in identification of persons with possible mental health issues, to make appropriate referrals, and for task shifting of mental health interventions to nonspecialists.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We wish to thank our colleagues at Translational Psychiatry Laboratory and Department of Psychiatric Social Work at NIMHANS, Bengaluru, India, for their valuable suggestions at different stages of the study and the members and officials of the SHGs under Pandeshwara Federation of SKDRDP, Sasthan, Udupi, India.
REFERENCES
- The mental health workforce gap in low- and middle-income countries: A needs-based approach. Bull World Health Organ. 2011;89:184-94.
- [Google Scholar]
- Resources for mental health: Scarcity, inequity, and inefficiency. Lancet. 2007;370:878-89.
- [Google Scholar]
- WHO. The World Health Report 2001: Mental Health: New Understanding, New Hope. Geneva: World Health Organization; 2001.
- WHO. Atlas of Mental Health Resources in the World 2001. Geneva: World Health Organisation; 2001.
- Community study of knowledge of and attitude to mental illness in Nigeria. Br J Psychiatry. 2005;186:436-41.
- [Google Scholar]
- National Mental Health Programme: Time for a re-appraisal. In: Kulhara P, Avasthi A, Thirunavukarasu M, eds. Themes and Issues in Contemporary Indian Psychiatry. New Delhi: Indian Psychiatric Society; 2011. p. :2-26.
- [Google Scholar]
- Integrating mental health into public health: The community mental health development project in India. Indian J Psychiatry. 2014;56:215-20.
- [Google Scholar]
- A mental health training program for community health workers in India: Impact on knowledge and attitudes. Int J Ment Health Syst. 2011;5:17.
- [Google Scholar]
- Knowledge and attitudes of doctors regarding the provision of mental health care in Doddaballapur Taluk, Bangalore Rural district, Karnataka. Int J Ment Health Syst. 2012;6:21.
- [Google Scholar]
- Research mental health first aid training for the Chinese community in Melbourne, Australia: Effects on knowledge about and attitudes toward people with mental illness. Int J Ment Health Syst. 2010;4:1-7.
- [Google Scholar]
- NABARD. Status of micro finance in India (2007-2008). Mumbai: NABARD; 2008.
- Banking on Self-Help Groups: Twenty Years On. New Delhi: SAGE Publications India; 2012.
- SKDRDP. About SKDRDP. Available from: http://www.skdrdpindia.org/content/about/about.html
- Barriers to improvement of mental health services in low-income and middle-income countries. Lancet. 2007;370:1164-74.
- [Google Scholar]
- Mental health training program for community mental health staff in Guangzhou, China: Effects on knowledge of mental illness and stigma. Int J Ment Health Syst. 2014;8:49.
- [Google Scholar]
- Education in mental health promotion and its impact on the participants’ attitudes and perceived mental health. Ann Gen Psychiatry. 2011;10:33.
- [Google Scholar]
- Public education for community care. A new approach. Br J Psychiatry. 1996;168:441-7.
- [Google Scholar]
- Sustained improvements in students’ mental health literacy with use of a mental health curriculum in Canadian schools. BMC Psychiatry. 2014;14:379.
- [Google Scholar]
- Explanatory models of psychosis among community health workers in South India. Acta Psychiatr Scand. 2003;108:66-9.
- [Google Scholar]
- Community beliefs about causes and risks for mental disorders: A mental health literacy survey in a rural area of Maharashtra, India. Int J Soc Psychiatry. 2010;56:606-22.
- [Google Scholar]
- The impact of self-help groups on the mental health of widows and widowers. Am J Orthopsychiatry. 1986;56:435-49.
- [Google Scholar]
- Community-based mental health intervention for underprivileged women in rural India: An experiential report. Int J Family Med 2011 2011 621426
- [Google Scholar]






