Translate this page into:
M5 segment aneurysm presenting as “pure acute SDH”
Address for correspondence: Dr. Navneet Singla, Department of Neurosurgery, Postgraduate Institute of Medical Education and Research, Chandigarh, Punjab and Haryana, India. E-mail: drnavi2007@yahoo.co.in
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Spontaneous “pure acute subdural hematoma (SDH)” is arguably a rare condition. We report on a pregnant female patient presenting as spontaneous acute SDH without subarachnoid hemorrhage (SAH) due to rupture of distal (M5 segment) middle cerebral artery aneurysm. We hereby discuss the diagnostic dilemma of this rare condition, along with the need for watchful evaluation of acute SDH without preceding head injury presenting in emergency outpatient departments, especially when it is first encountered by a trainee resident.
Keywords
Acute subdural hematoma
aneurysm
subarachnoid hemorrhage
Introduction
Acute subdural hematoma (SDH) is a known complication of moderate to severe head injury. Sudden onset of loss of consciousness or development of neurological deficit in an otherwise healthy person is usually secondary to any cerebrovascular event. Spontaneous acute SDH is an uncommon manifestation of rupture of an intracranial aneurysm. Aneurysm of internal carotid artery (ICA)-posterior communicating artery (Pcom) is the most common site, followed by aneurysms of middle cerebral artery (MCA) and distal anterior cerebral artery (DACA). Reported incidence of acute aneurysmal SDH varies from 0.5 to 7.9%.[12] We report a rare case of M5 segment MCA aneurysm presenting as an acute SDH without accompanying detectable subarachnoid hemorrhage (SAH), a rare condition known as “pure SDH.”[3]
Case Report
A 25-year-old primigravida who was 2 months pregnant, with no history of any comorbid illness or trauma presented in emergency. Patient presented with decreased level of consciousness (E2V3M5) and right-sided hemiparesis of grade 3/5. There was no external mark of injury. Her history and systemic evaluation was negative for any cardiac anomaly. Hematological and biochemical parameters were within normal limits. Computed tomography (CT) revealed a spontaneous acute SDH in left frontotemporoparietal (FTP) region with thickness of 8 mm and midline shift toward the right side [Figure 1a]. There was no evidence of SAH. Magnetic resonance imaging (MRI) of brain was done to rule out any benign or malignant pathology leading to blood in subdural space [Figure 1b]. Digital subtraction angiography (DSA) of cerebral vasculature revealed a small aneurysm in the left side MCA peripheral branches (M5 segment), leading to acute SDH [Figure 2a–c]. Patient underwent left frontotemporal craniotomy with removal of acute SDH and clipping of aneurysm in the same sitting. She had uneventful recovery and was discharged in conscious state with subtle paresis on the right side. Patient is without any complication after 3 years of follow-up.
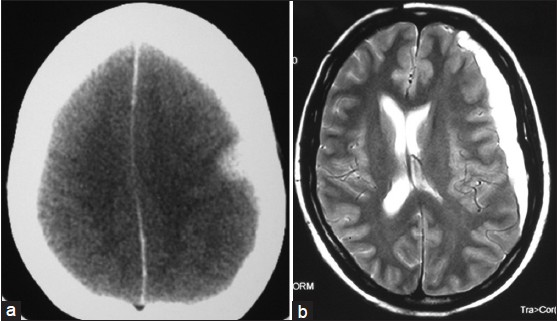
- (a) CT scan and (b) MRI T2-weighted images showing left FTP acute SDH with mass effect

- Digital subtraction angiography (DSA): (a) AP and (b, c) Lateral views showing aneurysm (arrow) at M5 segment
Discussion
The most common etiopathogenesis of acute SDH is traumatic disruption of a bridging vein draining into a venous sinus. Other less common etiologies include all conditions of nontraumatic acute SDH, among which are coagulopathies, vascular malformations, intracranial hypotension, cerebral sinovenous thrombosis, brain neoplasms, inflammatory conditions (certain vasculitis and vasculopathies involving the CNS, such as microscopic polyangitis), dissection of intraparenchymal hematomas into subdural space, and aneurysmal rupture.[3]
The various types of intracranial bleeding due to rupture of a cerebral aneurysm are SAH, intracerebral hematoma (30-40%), and intraventricular hematoma (12-17%).[4] Reported incidence of spontaneous SDH due to aneurysmal rupture varies from 0.5 to 7.9%. Pure aneurysmal SDH secondary to aneurysmal rupture is extremely rare. Fewer than 45 patients with pure aneurysmal SDH have been reported since 1855.[25]
Few mechanisms have been proposed to explain the causes of SDH after the rupture of saccular aneurysms: (1) successive small hemorrhages (sentinel hemorrhages) result in adhesions forming between the aneurysm and arachnoid, which create a path from dome to subdural space, and the final rupture occurs in the subdural space; (2) high pressure emanating from the ruptured aneurysm causes tearing of arachnoid through which blood extravasates into subdural space; (3) a massive hemorrhage results in rupture of cortex and arachnoid;[25] and (4) perianeurysmal environment (i.e., toward the cisternal space or parenchymal location of aneurysm) influences bleeding from the aneurysmal rupture. This might explain the rarity of acute SDH with vertebrobasilar aneurysms as the thick Liliequist membrane acts as a barrier for development of acute SDH.[6] Any of the above-mentioned factors might lead to an acute SDH formation due to an aneurysmal rupture, either alone or in combination.
Aneurysmal SDH is a diagnostic dilemma, especially in cases with trivial head injury. In such situations, patients may be brought to emergency room with history of “head injury,” and differentiation between SDH due to head trauma and SDH due to aneurysmal rupture may be virtually impossible.[7] In most of the cases, aneurysmal SDH is associated with SAH. In rare circumstances, aneurysmal SDH may be present in the absence of SAH, which may lead to inappropriate diagnosis and management. Emergency care physicians should be reminded of this rare entity and keep in mind that an aneurysmal SDH may present without accompanying SAH with any history of preceding head injury.
In emergency settings, most of the causes for acute SDH can be ruled out by an emergency contrast-enhanced CT or MRI.[3] Still the gold standard to rule out any aneurysmal pathology is conventional angiography, but for emergency settings, 3D CT angiography is an acceptable alternative as it is less time consuming. For patients presenting with suspected history, 3D CT angiography is recommended, as it is useful in patients with (1) acute SDH and no history of head trauma, (2) SDH and a history of probable sentinel bleeding, (3) rapidly progressing symptoms and sings that suggest bleeding of arterial origin, or (4) mild head trauma whose CT findings show disproportionately massive SDH with or without SAH.[8]
Outcome of these patients is usually poor because of poor grade at the time of presentation and delay in diagnosis. Poor outcome appeared to be associated with worse SAH grade at the time of admission, a greater midline shift, and greater SDH volume.[79] The presence of acute SDH in patients with aneurysmal SAH has been identified as an independent risk factor for poor outcome at discharge and at 3 months follow-up.[910] Usually patients present in a poor Hunt and Hess scale and overall the most common grade is grade IV or V. Once diagnosis is confirmed, a single-stage operation with evacuation of SDH and clipping of aneurysm has been shown to be superior to staged operation.[1]
Conclusion
Spontaneous arterial SDH due to an M5 segment aneurysm has never been reported earlier. This case highlights the need for watchful evaluation of acute SDH presenting in emergency, especially in nontraumatic settings or when the degree of impact to head seems disproportionately mild for CT findings of massive SDH and SAH. These cases are frequently delayed because of missed diagnosis due to complexity of presentations. As findings can be missed on conventional CT scans, an angiographic imaging (preferably 3D CT angiography) must be included in the diagnostic workup of patients with nontraumatic acute SDH.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Management of acute subdural hematomas from aneurysmal rupture. Can J Neurol Sci. 1984;11:371-6.
- [Google Scholar]
- Acute subdural haematoma secondary to ruptured intracranial aneurysm: Diagnosis and management. Br J Neurosurg. 1994;8:439-45.
- [Google Scholar]
- Pure subdural hematoma due to cerebral aneurysmal rupture: An often delayed diagnosis. Cardiovasc Intervent Radiol. 2010;33:870-3.
- [Google Scholar]
- Intracranial aneurysms causing spontaneous acute subdural hematoma. Neurol India. 2003;51:422-4.
- [Google Scholar]
- Pure acute subdural haematoma without subarachnoid haemorrhage caused by rupture of internal carotid artery aneurysm. Acta Neurochir (Wien). 2000;142:941-4.
- [Google Scholar]
- Aneurysm-related subarachnoid hemorrhage and acute subdural hematoma: Single-center series and systematic review. J Neurosurg. 2013;118:984-90.
- [Google Scholar]
- Acute subdural hematoma caused by ruptured cerebral aneurysms: Diagnostic and therapeutic pitfalls. Resuscitation. 2002;52:71-6.
- [Google Scholar]
- Acute Aneurysmal Subdural Hematoma: Clinical and Radiological Characteristics. J Korean Neurosurg Soc. 2005;37:329-5.
- [Google Scholar]
- Prognosis of acute subdural haematoma from intracranial aneurysm rupture. J Neurol Neurosurg Psychiatry. 2013;84:254-7.
- [Google Scholar]
- Risk factors for acute subdural hematoma from intracranial aneurysm rupture. Neurosurgery. 2012;71:264-9.
- [Google Scholar]






