Translate this page into:
Isolated hemimegalencephaly in an adult
Address for correspondence: Dr. Bhuma Vengamma, Department of Neurology, Sri Venkateswara Institute of Medical Sciences, Tirupati - 517 507, Andhra Pradesh, India. E-mail: bvengamma@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Sir,
There are a few reports of hemimegalencephaly (HME) in adults; we are reporting a case of isolated HME in a male adult.
A 30-year-old right-handed male patient presented 3 years back with complaints of recurrent episodes of seizures for the past 26 years. Seizures were right focal motor seizures with secondary generalization with a frequency of 10-15 episodes per month initially. There was a history of gradual onset of weakness in right upper and lower limbs. He also had intellectual disability. On examination, patient did not have any cutaneous markers to suggest of neurocutaneous syndrome. He had dysarthria, mini-mental state examination score was 13/30 and Addenbrooke's Cognitive Examination (52/100), right side upper motor neuron type facial nerve palsy, and mild right-sided spastic hemiparesis with extensor plantar response.
Electroencephalogram (EEG) was grossly abnormal, there was diffuse background slowing with theta and delta activity with almost continuous bursts of spike/polyspikes, sharp, and slow wave discharges over left hemisphere [Figure 1]. Magnetic resonance imaging (MRI) of brain [Figure 2] showed enlarged left frontoparietal lobe with smooth thickened cortex and pachygyria, indistinct grey/white differentiation, subcortical white matter showed hyperintensity on T2-weighted axial image [Figure 2a];, hypointensity on T1-weighted coronal image [Figure 2b], and hyperintensity on Fluid Atte nuated Inversion Recovery axial image [Figure 2c], straightening of the left frontal horn. He was treated with oral sodium valproate 10 mg/kg body weight initially, and gradually the dose was increased to 20 mg/kg body weight to control seizures. During the follow-up period of two and half years, there was no recurrence of seizures.
HME is a severe developmental malformation of the brain, remarkable for its extreme asymmetry.[1] Localized megalencephaly accounts for one quarter of all HME cases and predominantly seen on the left side (72.7%).[2] It is divided into three forms: (1) Isolated form, most common (66%); (2) syndromic form associated with several neurocutaneous syndromes; and (3) total HME, less common.[1] The classic neurological triad includes intractable seizures with onset typically within the first few months of life is the most common presenting symptom, contralateral hemiparesis, and severe psychomotor delays.[12] Causes of HME may be related to insults as early as the third week of gestation. One of the mechanisms of pathogenesis of HME is a disorder of cellular lineage and establishment of symmetry that occurs around the third week of gestation.[13] Recently, the etiology of HME was demonstrated as somatic mutation of AKT3.[45] The common EEG pattern is an asymmetrical background activity and sporadic wide spikes and/or spikes-waves complexes are usually confined to the malformed hemisphere. Other two less common patterns are the unilateral suppression burst and unilateral hypsarrhythmia over the abnormal hemisphere.[15] MRI of brain reveals the following: Unilateral enlargement of one or part of the cerebral hemispheres; with a thickened cortex; broad gyri, polymicrogyria, or agyria; shallow sulci; indistinct grey/white differentiation; increased volume and T2 signal of white matter; neuronal heterotopia; ipsilateral ventriculomegaly with straightening of the frontal horn; gliosis; and calcifications; basal ganglia and internal capsule abnormalities; and an “occipital sign” (displacement of the occipital lobe across the midline).[12] The goal of the treatment is to control epilepsy, which can be difficult to manage medically and epilepsy surgery is indicated in such severe refractory cases. Although this patient had recurrent seizures for the past 26 years, he responded to medical treatment recently. Based on clinical, EEG, and image findings, isolated localized form of HME in left fronto-parietal lobe was diagnosed. According to the literature, there are only a few reports of HME in adults.
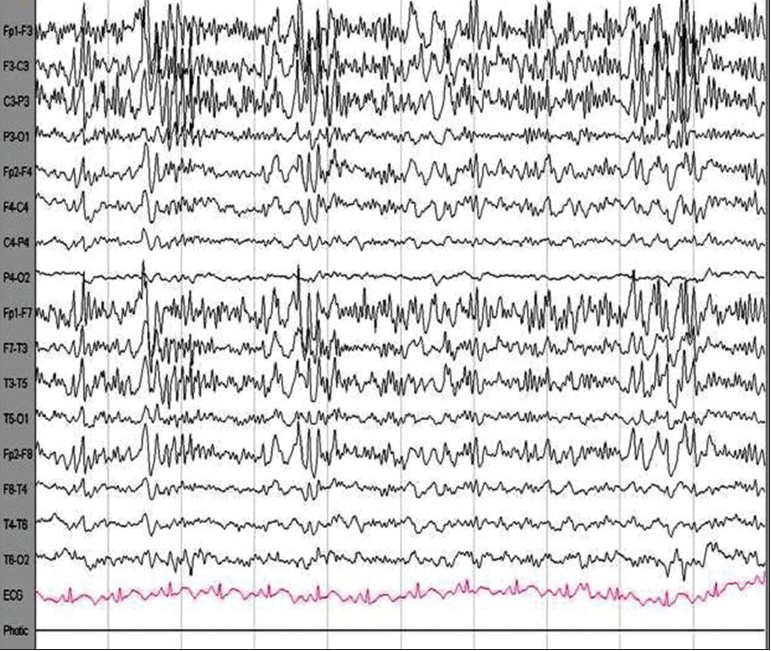
- Electroencephalogram was grossly abnormal showing diffuse background slowing with theta and delta activity on left side compared with right side with almost continuous bursts of spike/polyspikes, sharp and slow wave discharges over left hemisphere

- Magnetic resonance imaging of brain revealed enlarged left frontoparietal lobe with thickened cortex; pachygyria; indistinct grey/white matter differentiation; white matter (a) hyperintensity on T2-weighted axial, (b) hypointensity on T1-weighted coronal, and (c) hyperintensity on Fluid Attenuated Inversion Recovery axial; and straightening of the left frontal horn
References
- Hemimegalencephaly: Part 1.Genetic, clinical, and imaging aspects. J Child Neurol. 2002;17:373-84.
- [Google Scholar]
- Clinical and imaging characteristics of localized megalencephaly: A retrospective comparison of diffuse hemimegalencephaly and multilobar cortical dysplasia. Neuroradiology. 2009;51:821-30.
- [Google Scholar]
- Hemimegalencephaly: Part 2.Neuropathology suggests a disorder of cellular lineage. J Child Neurol. 2003;18:776-85.
- [Google Scholar]
- De novo somatic mutations in components of the PI3K-AKT3-mTOR pathway cause hemimegalencephaly. Nat Genet. 2012;44:941-5.
- [Google Scholar]
- Somatic activation of AKT3 causes hemispheric developmental brain malformations. Neuron. 2012;74:41-8.
- [Google Scholar]





