Translate this page into:
Ischemic stroke following abuse of Marijuana in a Nigerian adult male
Address for correspondence: Dr. Olalekan Oyinloye, Department of Radiology, University of Ilorin, Ilorin, Nigeria. E-mail: oyinbuk2001@yahoo.com
This is an open-access article distributed under the terms of the Creative Commons Attribution-Noncommercial-Share Alike 3.0 Unported, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Cannabis is the most widely used illicit drug among adolescents and young adults. Despite its widespread use, only a few reports exist on the association of cannabis use and stroke. A 26-year-old Nigerian male, developed right-sided ischemic stroke few hours after smoking three wraps of cannabis. He had smoked cannabis consistently for the past 4 years prior to the development of the stroke. Known stroke etiology and abuse of other illicit drugs were ruled out from history and investigations. Neuroimaging studies of the brain revealed infarcts in basal ganglia secondary to occlusion of blood flow in the left anterior and middle cerebral arteries. The mechanism of stroke in this patient was thought to be a cannabis-induced vasculopathy. Many cases of stroke in the young are increasingly being seen in hospitals in resource scarce countries. There seems to be a predilection for the basal ganglia in ischemic stroke following cannabis abuse. Therefore, cannabis abuse should be considered in young adults with basal ganglia infarcts, after excluding other known etiologies.
Keywords
Ischemic stroke
marijuana
neuroimaging
Introduction
The use of recreational drugs is a risk factor for cerebrovascular disease among young people.[1] Drug abuse has been implicated as the cause of stroke in 15-40% of stroke in the young.[2] Illicit substances such as opiates, cocaine, heroin amphetamine, Phencyclidine and marijuana have all been reported to predispose to strokes in young adults.[12] Cannabis is the most reported illicit drug worldwide[2] including Nigeria. A significant percentage of adolescent and young adults are engaged in the use of this substance.[3]
Case Report
A 26-year-old male presented with complaints of the sudden occurrence of slurred speech, weakness on the right half of the face, right upper limb with subsequent involvement of the right lower limb of 4 days duration. Three hours prior to the development of these symptoms he had smoked three wraps of street marijuana. He denied use of other street drugs and alcohol.
On examination, he was fully conscious and alert. Blood pressure was 120/70 mmHg and pulse rate 80 beats/minutes, regular with good volume. He had paralysis of right facial nerve upper motor neuron lesion type. There was complete motor paralysis (power 0) on the right upper and lower limbs and loss of sensation to pinprick and temperature. The pupils were normal bilaterally and react normally to light.
Fasting blood sugar was 97 mg/dl. All hematologic parameters were within normal values (full blood count, platelet count and prothrombin time and partial thromboplastin time). The serum chemistry and the lipid profile were also normal. The HIV screening test for type I and II was negative as well as VDRL test. No abnormality was detected on electrocardiogram and echocardiogram. There was no evidence of a patent foramen ovale. Urine toxicological screening on admission was positive for cannabis and negative for amphetamines, cocaine, methadone, opiates.
A computed tomography (CT) brain scan done 4 days after the onset of symptoms showed left basal ganglia infarct [Figure 1]. He subsequently had a magnetic resonance examination which showed a hypointense lesion in the left corpus striatum and insular cortex on T1W, [Figure 2a] and correspondingly high T2W consistent with infarcts [Figure 2b]. Magnetic resonance angiography (MRA) of the intracranial vasculature showed reduced flow in the left internal carotid artery and absence of flow in the left and anterior middle cerebral arteries consistent with his deficit [Figure 3].
Part of treatment, the patient received was aspirin therapy, vitamin E and physiotherapy. The patient made minimal improvement in his neurologic deficit and was discharged home after 2 weeks. He has since been lost to follow up, a common problem in developing countries.

- Contrast-enhanced CT, showing non-enhancing hypodense lesion in the left corpus striatum and insula cortex consistent with infarcts
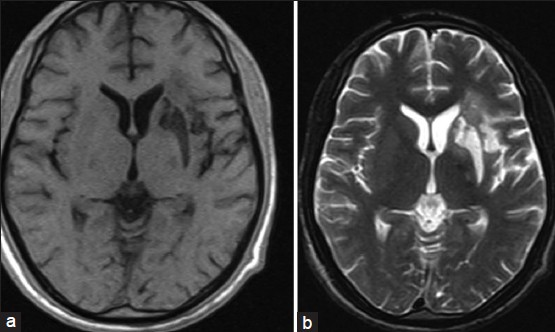
- (a) T1W axial MRI image showing hypoiintense lesion in the left corpus striatum and insula cortex (b) T2W axial MRI image showing hyperintense lesion in the left corpus striatum and insula cortex

- MRA showing marked reduction in the caliber of the left internal carotid artery, with occlusion of the left middle and anterior cerebral artery
Discussion
This illustrated case demonstrates an association between ischemic brain lesion and use of cannabis in a young Nigerian Adult. Usually, there is an antecedent history of heavy consumption of cannabis prior to the ischemic event as in this case report. This was well illustrated in a 36-year-old male who had three episodes of recurrent ischemic stroke over a two and half year interval, each episode occurring immediately after cannabis consumption.[4] More recently in a study involving a cohort of 17 patients who consumed cannabis, 5 patients had recurrent stroke with re-exposure to cannabis.[5] The absence of other vascular risk factors in most of the patients, the temporal relation of symptom onset to cannabis exposure, and the recurrence of symptoms in those patients with re-exposure suggest a causal role of cannabis in these cases of ischemic stroke.
There seems to be a predilection for the basal ganglia in strokes associated with cannabis consumption in young adults. Series of case reports, in which cannabis use was complicated by ischemic CVA, were demonstrated by neuroimaging to have lesions in the basal ganglia, as also seen in this patient.
Zachariah reported focal neurological deficit following cannabis use in two young male adults and in each case CT demonstrated basal ganglia infarction.[6]
Barnes et al. reported the case of a 30-year-old man presented with expressive dysphasia during cannabis use and magnetic resonance imaging (MRI) demonstrated striatocapsular infarction.[7]
In another report a 23-year-old man developed stroke after using large amounts of cannabis, and the brain CT showed a large subcortical infarction involving the striatum and internal capsule.[8] The posterior circulation in children and adolescent have also been reported as regions of predilection in stroke cases following abuse of cannabis. There are reported cases of cerebellar hemispheric infarction in four teenagers between age 15 and 17 years following heavy cannabis use.[9]
The active chemical in Marijuana called delta-9-tetrahyrdocannabinol (THC) is believed to exert these effects by binding to cannabinoid (CB) receptors located on several cell types in various organs. The cannaboid receptor CB1 and CB2 are most abundant in the basal ganglia and cerebellum. Activation of these receptors modulates the cellular activity of the vessel wall, which may contribute to the pathogenesis of atherosclerosis. This may perhaps be a possible explanation for the increased incidence of ischaemic stroke in the basal ganglia and cerebellum.[10] A concentration of Marijuana in urine exceeding 50 ng/mL is the suggested screening cut off for positive specimens set by the Substance Abuse and Mental Health Services Administration (SAMHSA, USA). This represents the level at which the urine strip test for marijuana becomes reactive.
Proposed mechanisms of stroke associated with cannabis use include postural hypotension cardioembolism, vasospasm, vasculitis and reversible cerebral vasoconstriction syndrome.[2] There was no evidence of postural hypotension in this patient. He was normotensive at presentation and subsequently after. The pulse rate, ECG and echocardiogram were also normal in this patient. Cannabis-induced arteritis of peripheral vessels have also been described.[411] Patients in which arteritis were found are regular users of cannabis and tobacco smokers.[411] Mateo et al.[4] described a mild decrease in the distal branches of the left MCA on MRA in a patient with recurrent stroke after cannabis abuse and suggested that the most likely mechanism was a vasculopathy, either toxic or immune inflammatory, elicited by cannabis. It is plausible that this might be the mechanisms for stroke in this illustrated case.
Recently there has been advocation for the use of Marijuana in treatment of medical ailments, especially in palliative health. There is no strong evidence that it has a definitive therapeutic benefit in any specific disease condition. Interestingly, the advocates of “medical marijuana” insist that the substance be smoked in order to receive maximal medicinal benefit. This exposes the individual to toxins associated with smoke inhalation.[10] The American Society of Addiction Medicine maintains that there is no entity known as “medical marijuana.” Moreover, the Society warns against the many serious, well-documented, negative health effects of this drug.[10]
Unfortunately, this patient was lost to follow up as the case in developing countries where patients seek alternatives to orthodox medical care since health seeking habit is often influenced by Sociocultural factor. It there was therefore impossible for us to ascertain the outcome in this young man.
In conclusion, cannabis use should be excluded in young adults with ischemic stroke, in which known etiologies have been excluded and have demonstrated lesions in the basal ganglia on neuroimaging.
Source of Support: Nil.
Conflict of Interest: None declared.
References
- Occurrence of stroke associated with use/abuse of drugs. Neurology. 1991;41:1358-64.
- [Google Scholar]
- Pattern of Marijuana use among male university students: A case study. J Med Sci. 2007;7:1068-72.
- [Google Scholar]
- Recurrent stroke associated with cannabis use. J Neurol Neursurg Psychiatry. 2005;76:435-7.
- [Google Scholar]
- Cannabis-related stroke: Case series and review of literature. J Stroke Cerebrovasc Dis. 2012;21:555-60.
- [Google Scholar]
- Cerebrovascular disease associated with marijuana abuse: A case report. Cerebrovasc Dis. 2001;11:284-5.
- [Google Scholar]
- Cerebellar infarction in adolescent males associated with acute marijuana use. Pediatrics. 2004;113:e365-70.
- [Google Scholar]
- 2013. Practical Neurology-Marijuana Use and Ischemic Stroke. Available from: https://webcache.googleusercontent.com/search






