Translate this page into:
Intracranial Ossified Metaplastic Meningioma: Unusual Cause of Headache
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
A 33-year-old female presented with history of headache for 6 months. There was no history of seizures. Plain and contrast-enhanced computed tomography showed a large extraaxial completely ossified lesion with lobulated margins in the left frontal region with extension across the diploic space, into overlying scalp [Figure 1 and Video 1]. There was no enhancing soft tissue component. There was no perilesional edema. Craniotomy and near total excision of the tumor were done. Histopathological examination revealed metaplastic meningioma of ossific subtype. Meningiomas, the most common benign intracranial tumors, arise from arachnoid cap cells. They are also the most common nonglial primary tumor and most common extraaxial neoplasm. Meningiomas classically appear as hyperdense homogeneously enhancing mass. Calcification seen in 20%–27% of meningiomas is usually punctuate but may be large.[1] Ossified meningioma, classified histologically as a phenotype of metaplastic meningioma, is extremely rare and belongs to WHO Grade I. Other histological phenotypes of metaplastic meningioma include cartilaginous, lipomatous, myxoid, xanthomatous, and cartilaginous tissue. The majority of ossific meningiomas are spinal in location with <20 cases of intracranial ossified meningioma reported so far.[23] Clinical symptoms include headache, dizziness, seizure, blurred vision, and weakness of lower limbs. Surgical removal is the ideal treatment option, with radiotherapy being useful in recurrent cases. Although not extensively studied, overall prognosis of metaplastic meningiomas is good.[3]
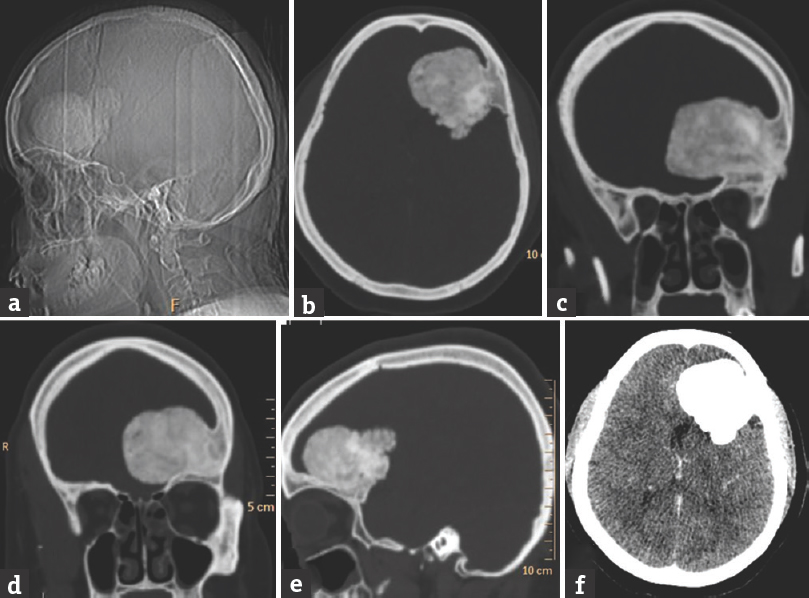
- Computed tomography (a) scanogram and (b-e) sections in bone window show a large well-defined extraaxial ossified lesion with lobulated margins lesion in the left frontal region with extension across the diploic space, into the overlying scalp tissue. (f) The same lesion in brain window
Video available on: www.ruralneuropractice.com
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Incidence and clinicopathological features of meningioma. J Neurosurg. 1989;71(5 Pt 1):665-72.
- [Google Scholar]
- Ossified metaplastic meningioma with intratumoral hemorrhage. J Cytol Histol. 2010;1:102.
- [Google Scholar]
- Clinicopathological analysis of metaplastic meningioma: Report of 15 cases in Huashan Hospital. Chin J Cancer Res. 2013;25:112-8.
- [Google Scholar]





