Translate this page into:
Intra-Parenchymal Cerebellar Metastasis—A Rare Presentation of Castration-Resistant Prostate Cancer
Sufyan Ibrahim, MBBS Department of Neurosurgery, Kasturba Medical College, Manipal Academy of Higher Education Manipal 576104, Karnataka India sufyan.ibrahim2@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Abstract
Intracranial metastases from prostate carcinoma are uncommon and usually manifest as dural secondaries in the supratentorial compartment. We present an unusual case of intra-parenchymal posterior fossa prostatic metastasis in a 61-year-old gentleman and discuss the diagnostic and management challenges involved. A 61-year-old hypertensive, diabetic man presented with gait unsteadiness for 1-month duration and no other neurological deficits. He had previously undergone bilateral orchiectomy for prostate carcinoma with multiple osseous metastases. Magnetic resonance imaging showed a well-defined lobulated, intraventricular, peripherally enhancing lesion in the fourth ventricle with obstructive hydrocephalus. He underwent sub-occipital craniectomy and decompression, and histological examination was consistent with metastatic prostate adenocarcinoma. Although cerebellar secondaries are atypical, a suspicion of metastasis should be upheld in all patients with the history of prostate carcinoma, regardless of their location and radiological characteristics of the intracranial lesion.
Keywords
prostate
adenocarcinoma
cerebral metastases
dural secondaries
Introduction
Prostate carcinoma is the third most common cancer, accounting for over 7% of all cancers worldwide, and the sixth leading cause of cancer-related deaths occurring among men.1 Extra-prostatic spread of tumor is primarily in the form of metastasis to the regional lymph nodes, skeleton, and sometimes to liver, lungs, peritoneum, and adrenals.2 Intracranial metastasis associated with prostate carcinoma is rare and extremely uncommon.3 We herein describe an unusual case of symptomatic posterior fossa metastasis in a patient with prostate carcinoma and discuss the management dilemmas.
Case Report
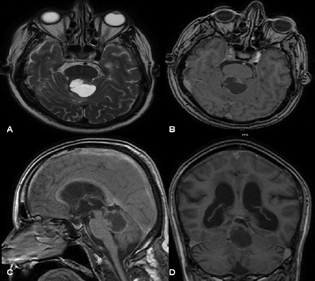
A 61-year-old male presented to the hospital with complaints of gait unsteadiness of 1-month duration with no features of raised intracranial pressure or any other neurological deficits. A known hypertensive and diabetic, he was diagnosed with adenocarcinoma of prostate, Gleason grade 3a + 3c, and multiple bony metastases, for which he underwent bilateral orchiectomy 4 years ago. Magnetic resonance imaging (MRI) of the brain revealed a well-defined lobulated, intraventricular, peripherally enhancing lesion in the fourth ventricle with obstructive hydrocephalus (Fig. 1). The radiological features were not suggestive of a metastatic lesion, and vermian astrocytoma was kept as the first diagnostic possibility. He underwent sub-occipital craniectomy with the decompression of the lesion in the posterior fossa. The lesion was vascular with attachment to the vermis and tectal plate. Histological examination showed malignant cuboidal cells in a cribriform pattern with evidence of anisonucleosis, frequent mitosis, and hemorrhage, suggestive of metastatic prostate carcinoma.
-
Fig. 1 (A) Axial T2 and (B) contrast images showing a hypointense rim enhancing lesion in the region of the superior vermis extending to the tectal plate. (C) Sagittal contrast and (D) coronal contrast images showing the rostrocaudal extent of the lesion extending from the level of the midbrain to the upper part of medulla.
Fig. 1 (A) Axial T2 and (B) contrast images showing a hypointense rim enhancing lesion in the region of the superior vermis extending to the tectal plate. (C) Sagittal contrast and (D) coronal contrast images showing the rostrocaudal extent of the lesion extending from the level of the midbrain to the upper part of medulla.
Discussion
Cerebral metastasis reportedly occurs in 10 to 40% of all malignant neoplasms and accounts for more than 50% of all brain tumors in adults.3 Prostate cancer is the second most common malignancy in males and usually metastasizes to the spine and lung via hematogenous or lymphatic route. Spinal epidural compression secondary to vertebral involvement is the most common indirect central nervous system manifestation of prostatic carcinoma.3 Cerebral metastasis is, however, unusual from prostatic primary and ranges from 0.6 to 4.4%. When seen within the brain, prostatic metastasis occurs in the leptomeninges (67%), cerebrum (25%), followed by the brainstem and pituitary gland. The involvement of the posterior fossa is extremely rare, and cerebellar metastasis accounts for less than 8% of all patients.
Ganou et al have attempted to classify cerebral metastasis from a prostatic primary into four sub-types—(1) pure subdural space lesions, (2) dural-based lesions, (3) extradural/bony lesions, and (4) pure intra-parenchymal lesions. The dura mater, which usually acts as a barrier to metastatic penetration, appears to be the prime target in cases of prostatic secondary. The typical localization in the dural layers or subdural space suggests a compromised blood–brain barrier or a depressed immune function which typically happens in the late stages of the disease. Dural metastasis is known to mimic a subdural hematoma or an abscess, and interesting case reports of metastatic spread to the membranes of a true chronic subdural hematoma have been described.4 Thus, in the differential diagnosis of subdural collections, without any history of recent head injuries, prostatic metastasis needs to be considered. The osteoblastic changes induced on the dural layers can at times mimic a meningioma too.3 Pure parenchymal intra-axial metastatic lesions especially in the cerebellum are extremely uncommon. Our case is, thus, unique in that it highlights the importance of maintaining a strong suspicion of metastasis in any intracerebral pathology detected in a patient with the history of prostatic carcinoma.
Patients with cerebral metastasis commonly present with headaches, giddiness, confusion, and location-specific neurological deficits. Gadolinium-enhanced MRI is the investigation of choice for better delineation of the metastatic foci and their true extent.1 Available treatment options include surgical debulking, radiotherapy, and radiosurgery, as well as the usage of chemotherapeutical agents.3 Surgery should be offered as the treatment of choice for solitary, accessible lesions, in patients having good functional status as it has shown to increase the quality of life remarkably in such patients. Radiosurgery is a valuable alternative for inaccessible or eloquent area lesions. Whole-brain radiotherapy must be considered if there are numerous lesions or in the presence of carcinomatous meningitis. The combination of chemotherapy (docetaxel and cabazitaxel) and second-generation hormonal therapies (enzalutamide and abiraterone) is proven to be effective during the castration-resistant phase. Although docetaxel is considered as the drug of choice, cabazitaxel can cross blood–brain barrier but its efficacy remains unproven.5
With newer treatment adjuncts, prognosis following prostatic carcinoma has improved considerably. This increase in longevity, however, is associated with an increase in the incidence of cerebral metastasis. Cerebral metastases from prostate carcinoma used to be considered as terminal events, with an estimated median of survival of 3.5 months. Negative prognosticators include age less than 55 years, prostate-specific antigen titers greater than 4 ng/mL, and presence of subdural metastasis.3 Prognosis for isolated intra-parenchymal lesions might not be as dismal as previously thought. Total surgical excision and tailored adjuvant radiation therapy may add to the overall survival.3
Conclusion
Cerebellar metastases are uncommon and radiologically different from dural secondaries that are more often associated with prostate carcinoma. A strong suspicion of metastasis needs to be maintained in all patients with the history of prostatic cancer presenting with intracranial lesions irrespective of their location and radiological features.
Conflict of Interest
None declared.
References
- Brain metastases from prostate cancer: an 11-year analysis in the MRI era with emphasis on imaging characteristics, incidence, and prognosis. J Neuroimaging. 2014;24(2):161-166.
- [Google Scholar]
- intracranial metastases from prostate carcinoma: classification, management, and prognostication. World Neurosurg. 2020;134:e559-e565.
- [Google Scholar]
- Brain metastasis from prostate carcinoma: the M. D. Anderson Cancer Center experience. Cancer. 2003;98(2):363-368.
- [Google Scholar]
- Frequency of brain metastases from prostate cancer: an 18-year single-institution experience. J Neurooncol. 2013;111(2):163-167.
- [Google Scholar]






