Translate this page into:
Impact of Road Traffic Injury to Pediatric Traumatic Brain Injury in Southern Thailand
This is an open access article distributed under the terms of the Creative Commons Attribution-NonCommercial-ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non-commercially, as long as the author is credited and the new creations are licensed under the identical terms.
This article was originally published by Medknow Publications & Media Pvt Ltd and was migrated to Scientific Scholar after the change of Publisher.
Abstract
Background:
Motor vehicle is a major transportation in Southern Thailand as the result of road traffic injury and death. Consequently, severe disability and mortality in pediatric traumatic brain injury (TBI) were observed from traffic accident, particularly motorcycle accident. To identify the risk of intracranial injury in children, the association of treatment outcome with various factors including mechanisms of injury, clinical characteristics, and intracranial pathology can be assessed.
Materials and Methods:
This was a retrospective study conducted on children, who were younger than 15 years old with TBI and were enrolled from 2004 to 2015. Several clinically relevant issues were reviewed and statistically analyzed.
Results:
A total of 948 casualties were enrolled. Compared with falling down, the motorcycle accident was significantly associated with intracranial injury (odds ratio 1.73, 95% confidence interval [CI] 1.08–2.76). Other factors associated with intracranial injury were hemiparesis (odds ratio 5.69, 95% CI 1.44–22.36), positive of basal skull fracture signs (odds ratio 15.66, 95% CI 3.44-71.28), and fixed reaction to light of both pupils (odds ratio 5.74, 95% CI 1.71–19.23). Mortality found in thirty cases (3.2%). Furthermore, the risk of death correlated with motorcycle accident (P = 0.02) and severe head injury (P < 0.001). Neurosurgical intervention was not associated with outcome, but severe head injury, hemorrhagic shock, epidural, and subdural hematoma were impact factors.
Conclusion:
The findings demonstrate road traffic injury, especially motorcycle accident leading to brain injury and death. Prevention program is a necessary key to decrease mortality and disability in pediatric TBI.
Keywords
Mechanism of injury
motorcycle accident
outcome
pediatric head injury
traffic injury
traumatic brain injury
INTRODUCTION
Traumatic brain injury (TBI) is the leading cause of death in all age group victims including children. As we know that injury in children tends to be more severe due to small body with large head, the mechanisms of injury are different among age group. TBI in infants will be from infliction and fall, but older children will be injured from road traffic injury.[12] World Health Organization (WHO) reported that road traffic mortality in children highly occurred in low-income and middle-income countries. Globally, road traffic death in children is 10.7 person per 100,000 population.[3]
The mechanisms of TBI in our country, especially in the southern part, differ from the well-developed country. In Thailand, motorcycles are used generally as a means of transportation due to lack of public transportation in all area. Hence, we here found most of TBIs caused by motorcycle crashes. Songklanakarind Hospital, the territory hospital and trauma level 1, services broadly in 14 provinces in the southern part of Thailand. More than two-thirds (69.6%–71.9%) of injuries related with motorcycle.[4] Our study was aimed to identify mechanisms of injury, especially road traffic injury and severity of TBI in children.
MATERIALS AND METHODS
All children admitted to Songklanakarind Hospital between 2004 and 2015. Inclusion criteria of this study were patients who were younger than 15 years and complete available medical records. A total of 996 patients were matched to our criteria, of which 48 patients were excluded because their medical records were inaccessible, patient who died before arrival at the emergency room, or 24 h after admission. Finally, 948 patients who matched the inclusion criteria were retrospectively analyzed.
This study was a retrospective review of the Hospital Information System. Reviewing medical records data included demographic data, mechanism of injury, intracranial injury, other associated injury, treatment, and outcome. In addition, severity of TBI categorized to mild, moderate, and severe group according to the Glasgow Coma Scale (GCS).[5] However, Pediatric GCS (PGCS) was used with children younger than 2 years.[6] GCS, PGCS, and pupil reactivity to light were documented when the patient had postresuscitated stable vital signs.
Neuroimaging described the type of intracranial injuries such as skull fracture, epidural hematoma, subdural hematoma, and cerebral contusion. Surgical treatment and outcome were reviewed. Appling King's Outcome Scale for Childhood Head Injury score evaluated the outcome at hospital discharge and last time follow-up.[7] Finally, outcome scores were dichotomized into favorable and unfavorable categories. The study was performed with the permission of the Ethical Committee of the Faculty of Medicine, Songklanagarind Hospital, Prince of Songkla University.
Statistical analysis
Patient characteristics, mechanism of injury, and intracranial injury were determined using descriptive analysis presented as proportions, mean ± standard deviation (SD). Therefore, correlation and magnitude of association between several factor and intracranial injury were demonstrated by binary logistic regression analysis. In multivariate analysis, stepwise regression was used to check whether variable deserves to be included in the model and stratification. A P < 0.05 was considered as statistically significant. Statistical analysis was performed using R program version 3.4.0.
RESULTS
The entire study population included 948 children. Table 1 shows the clinical characteristics of the entire study population. The two-thirds were male and mean age was 6.29 years ± SD 4.67, ranging from 1 month to 14 years 11 months. The most common mechanism of injury was road traffic injury (63.6%), especially motorcycle accident (43.5%), whereas falling observed in the one-third in this study. In motorcycle accident, the mean age was 13.5 ± 1.5 years and range of driver's age was between 7 years 10 months and 14 years 11 months. Most of the severity (84.4%) was mild head injury, and remaining was moderate-severe head injury. After postresuscitation, uncal herniation was observed in 2.3% while the absence pupil reaction was 4.2%. In this study, 71.2% of patients were investigated by computed tomography of the brain.

More than two-thirds (61.9%) of imaging study could found significant intracranial injury. Injured characteristics are demonstrated in Table 2. The most common finding was calvarial skull fracture (17.3%) and subdural hematoma (15.8%). Because developing skull is thinner, more pliable, ping-pong fracture which uniquely deformed skull could observed in 3.2% of cases. Diffuse brain injury such as subarachnoid, intraventricular, and brainstem hemorrhage could be observed in 9.2% of cases. Moreover, most extracranial-associated injury was long bone fracture (11.2%), maxillofacial injury (6.6%), and orbital injury (3.8%).
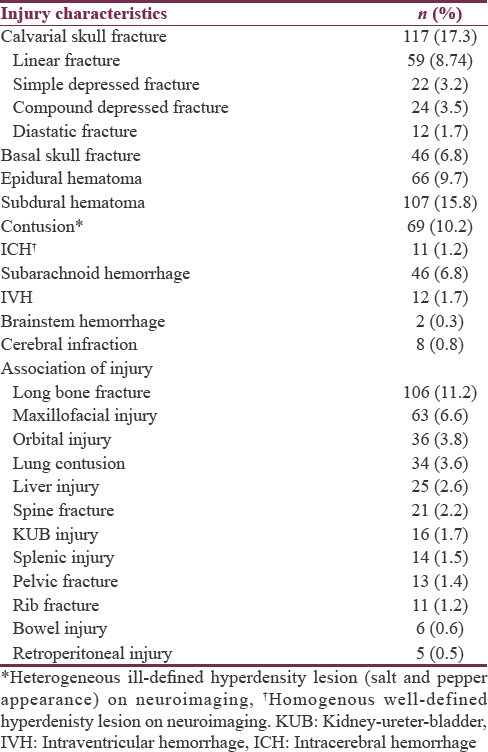
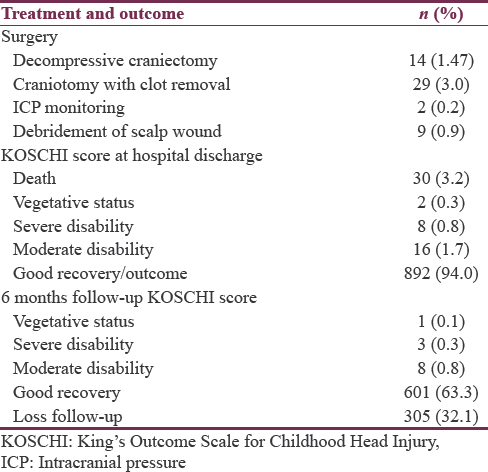
Table 3 summarizes the treatment and outcome of the present study. Most surgical treatment could found in moderate-severe head injury. 3.2% of mild head injury needed surgery while 15.7% and 22.7% of moderate and severe head injury, respectively, risk to neurosurgical intervention. Because of brain swelling, most decompressive craniectomy with clot removal operation (92.9%) approached in moderate and severe groups. All of two children received intraparenchymal intracranial pressure (ICP) monitoring had GCS score 3 and 7. Thirty cases (3.1%) in the present study died. Further, majority of mortality occurred in severe head injury (96.7%, P < 0.001 with Chi-square test) and motorcycle accident (46.7%, P = 0.02 with Chi-square test) while death from pedestrian injury, car accident, and fall was 6.7%, 10%, and 13.3%, respectively.
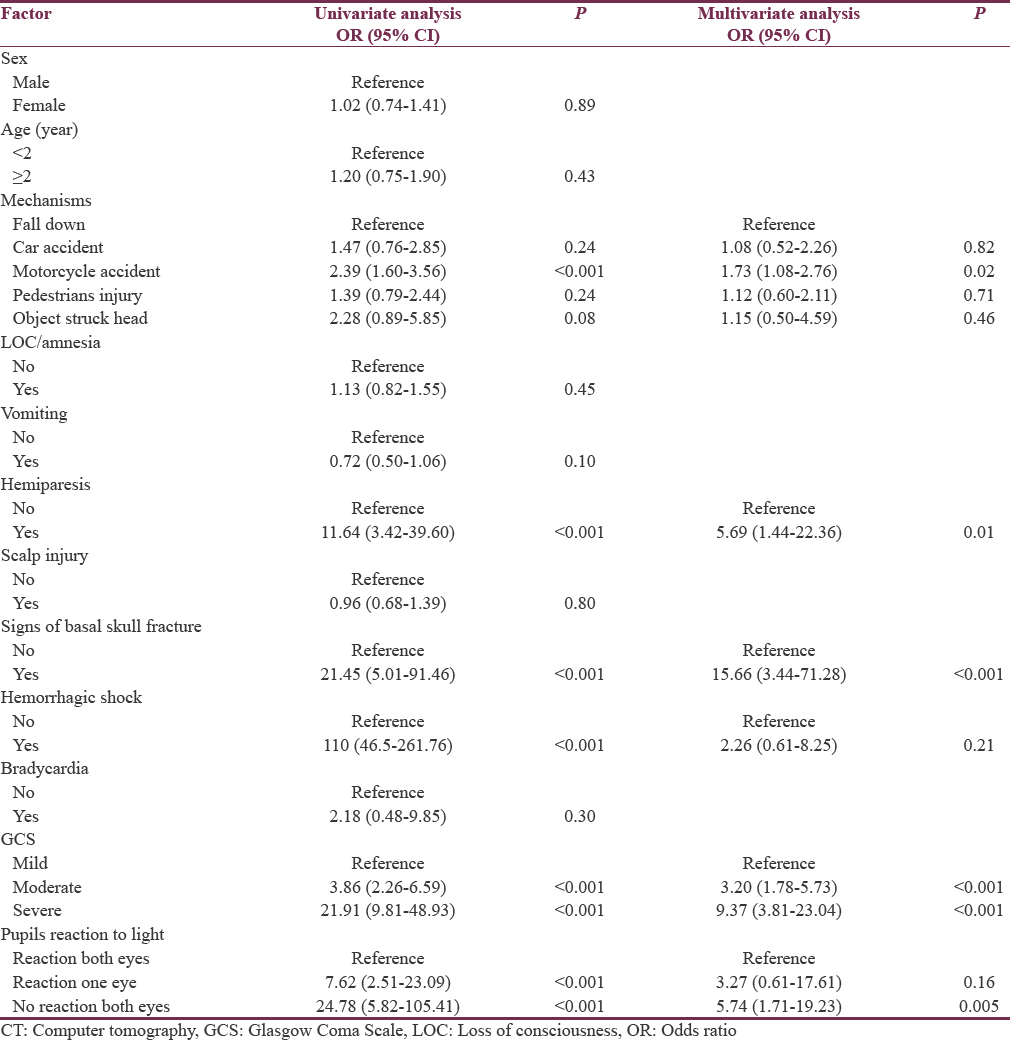
According to the aim of the study, binary logistic regression was used to analyze factors predicting for the intracranial injury. In univariate analysis, significant factors were motorcycle accident mechanism, hemiparesis, positive for basal skull fracture sign (periorbital or postauricular ecchymosis), hemorrhagic shock, moderate-severe head injury, and no reaction of pupil/pupils. Likewise, when multivariate analysis was used, motorcycle crash mechanism, hemiparesis, positive of basal skull fracture sign, moderate-severe head injury, and no reaction of pupils were still significant in the model as we can see in Table 4. Comparing with falling, motorcycle crash had significant risk to intracranial injury 1.73 times (95% confidence interval [CI] 1.08–2.76). The relevant clinical characteristics were hemiparesis (odds ratio 5.69, 95% CI 1.44–22.36), positive for basal skull fracture signs (odds ratio 15.66, 95% CI 3.44–71.28), and no reaction to light of both pupils (odds ratio 5.74, 95% CI 1.71–19.23). In addition, severe and moderate head injury significantly predicted intracranial pathology when compared with mild head injury (odds ratio 9.37, 95% CI 3.81–23.04 and 3.20, 95% CI 1.78–5.73, respectively).
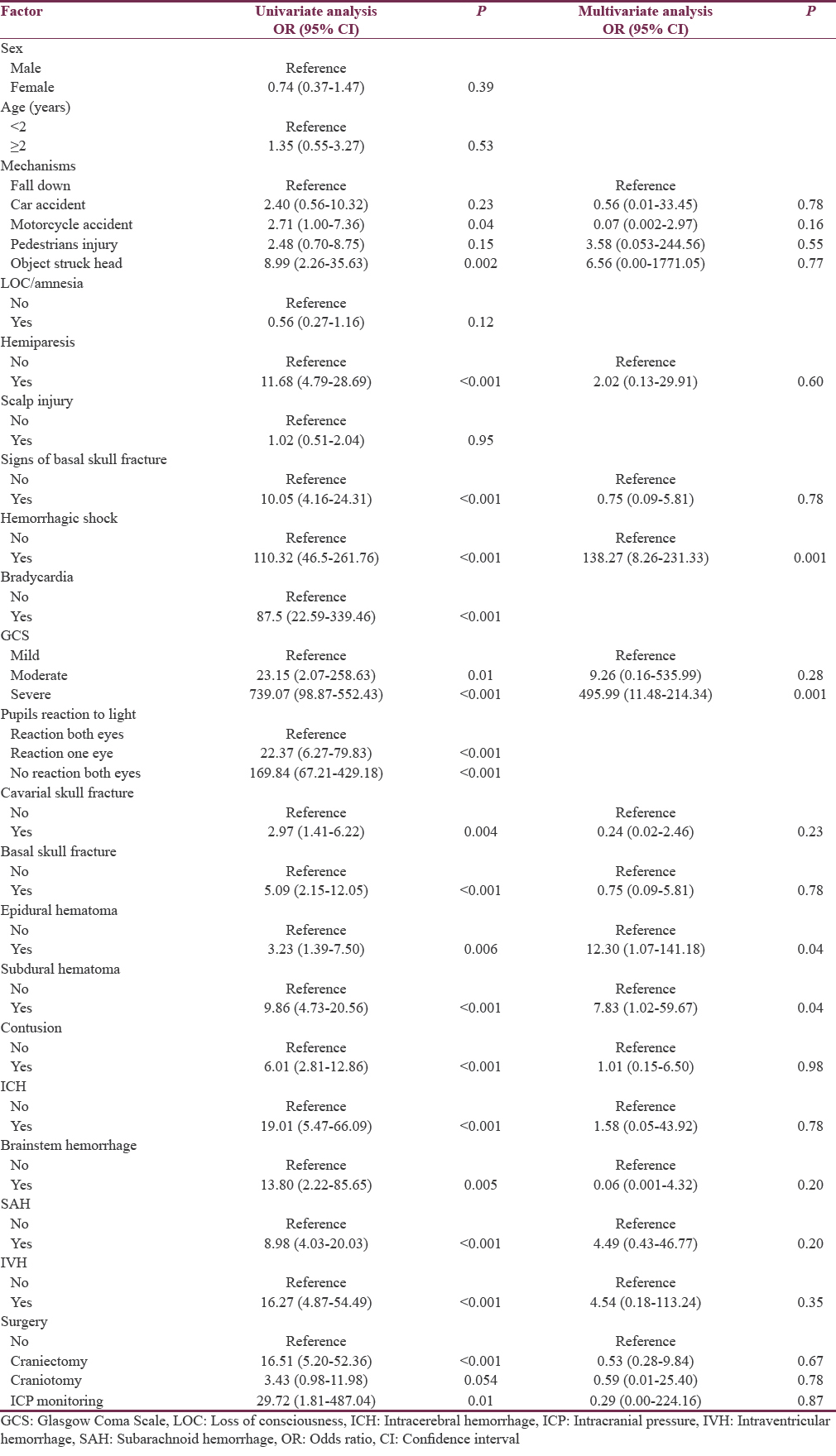
Outcome score was measured into two categories. Table 5 shows the factors associated with unfavorable outcome. Motorcycle crash and object hit head were the significant factors initially; however, these were insignificant in multivariate analysis. The relevant patient's characteristics predicted outcome was 8–3 score of GCS (odds ratio 495.99, 95% CI 11.48–214.34) and hypotension episode (odds ratio 138.27 95% CI 8.26–231.33). Finally, significant intracranial injury criticized to outcome was epidural hematoma (odds ratio 12.30, 95% CI 1.07–141.18) and subdural hematoma (odds ratio 7.83, 95% CI 1.02–59.67) while surgical treatment was inconsequential effect to outcome.
DISCUSSION
This present study demonstrated significant factors which associated with intracranial injury in Southern Thailand. Common intracranial pathology has been subdural hematoma (0.7%–2.6%), epidural hematoma (0.9%–2.3%), and contusion (0.7%–0.9%), while skull fracture could found <1%.[89]
We found that several intracranial injury was more frequent and serious than other studies. For example, traumatic focal brainstem hematoma is rare entitle and very poor prognosis. Based on the forensic study, pathophysiology of fatal brainstem hemorrhage occurred from loading at the back of the head or stretching loading at the brainstem. Patient characteristics usually immediately unconsciousness and 75% of cases died within a day.[10] We observed two patients with traumatic focal brainstem hematoma. Fifty percent of mortality rate of brainstem hemorrhage observed, but remaining patients had moderate disability at hospital discharge and good recovery when 6-month follow-up visit. As mentioned above, TBI in the present study revealed more severe than previous studies.
In literature review, the most mechanisms of pediatric TBI were fall from standing and fall from height between 17% and 68%, while traffic injury had been reported <5%.[1211121314] Although the most common cause of TBI is fall in younger than 2 years, more than one-thirds of TBI in this group occurred from motorcycle crash in the present study.
The road traffic injury mechanism showed that significant risk to brain injury than fall down and associated with mortality in this study. Concordance with the previous studies, Haider et al. reported traffic injury had risk to disability compared with fall and high-level fall mechanism (odds ratio 1.82, 95% CI 1.66–1.98).[15] Marlow et al. reported traffic accidents were common cause of death in children.[16] Reith et al. studied that pedestrians injury had mortality rate higher than motor vehicle occupants (13.2% vs. 7.0%).[17] However, motorcycle occupants had poor prognosis than pedestrians injury in the present study.
In Southern Thailand, motorcycle is widely used in daily carriage because public transportation has been limited. Data from Thailand Transport Portal in 2015, a total number of new registered motorcycle were 1,815,000 unit and average of each part of country was 400,000–100,000 unit.[18] In details, most crashes are usually caused by harmful traffic behaviors observed in daily at these regions, for example, nonhelmet usage, over number of passengers on motorcycle, and young rider. Surprisingly, the youngest motorcycle driver had 7 years 10 months in this present study. As the results, numerous injuries from accident are preventable when traffic law and prevention campaign are more concerned. Although most outcome was good, victims should not be suffered from disability. Consequently, morbidity and mortality directly impact to burden of the country.
Intracranial hemorrhage hematoma is usually preferred neurosurgical intervention in moderate-severe head injury in children.[19] However, neurosurgical treatment had less impact than clinical symptoms and mechanism.[20] For intracranial hypertension, decompressive craniectomy in the setting of pediatric TBI has been debated. The operation may be considered in children who have signs of brain herniation or neurological deterioration or persistent intracranial hypertension refractory to medication.[21]
Since the severity of brain injury is potential influence to outcome than standard treatment, primary prevention before accident event should be intensively considered as the same of WHO recognition. National policies and advocacy to prevent violence and injuries have been acknowledged.[22]
The study was limited by retrospective methodology. Clinical characteristic's patients may be incompletely assessed such as ICP which assumed correlation with outcome. However, the strengths of the study are number of study population that was sufficient to identify association. Moreover, the results in present study clarify the “real world” problem in our regions.
CONCLUSION
In Southern Thailand, motorcycle accident are common cause of serious intracranial pathologies and poor outcome. Any neurosurgical intervention was less effect than serious brain injuries. Resolving morbidity and mortality from TBI in the children should directly prevent harmful traffic behaviors.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- Brain injuries among infants, children, adolescents, and young adults. Am J Dis Child. 1990;144:684-91.
- [Google Scholar]
- Comparison of PECARN, CATCH, and CHALICE rules for children with minor head injury: A prospective cohort study. Ann Emerg Med. 2014;64:145-52.
- [Google Scholar]
- World Report on Child Injury Prevention. Geneva: World Health Organization; 2008.
- Assessment of coma and impaired consciousness. A practical scale. Lancet. 1974;2:81-4.
- [Google Scholar]
- Neurologic evaluation and support in the child with an acute brain insult. Pediatr Ann. 1986;15:16-22.
- [Google Scholar]
- Comparison of accidental and nonaccidental traumatic brain injuries in infants and toddlers: Demographics, neurosurgical interventions, and outcomes. J Neurosurg Pediatr. 2009;4:414-9.
- [Google Scholar]
- Association of traumatic brain injuries with vomiting in children with blunt head trauma. Ann Emerg Med. 2014;63:657-65.
- [Google Scholar]
- Risk of traumatic brain injuries in children younger than 24 months with isolated scalp hematomas. Ann Emerg Med. 2014;64:153-62.
- [Google Scholar]
- Focal traumatic brain stem injury is a rare type of head injury resulting from assault: A forensic neuropathological study. J Forensic Leg Med. 2012;19:144-51.
- [Google Scholar]
- Epidemiology of children with head injury: A national overview. Arch Dis Child. 2016;101:527-32.
- [Google Scholar]
- Infant head injury in falls and nonaccidental trauma: Does injury pattern correlate with mechanism? Pediatr Emerg Care. 2014;30:677-9.
- [Google Scholar]
- Identification of children at very low risk of clinically-important brain injuries after head trauma: A prospective cohort study. Lancet. 2009;374:1160-70.
- [Google Scholar]
- CATCH: A clinical decision rule for the use of computed tomography in children with minor head injury. CMAJ. 2010;182:341-8.
- [Google Scholar]
- Mechanism of injury predicts case fatality and functional outcomes in pediatric trauma patients: The case for its use in trauma outcomes studies. J Pediatr Surg. 2011;46:1557-63.
- [Google Scholar]
- Trends in admission and death rates due to paediatric head injury in England, 2000-2011. Arch Dis Child. 2015;100:1136-40.
- [Google Scholar]
- Injury pattern, outcome and characteristics of severely injured pedestrian. Scand J Trauma Resusc Emerg Med. 2015;23:56.
- [Google Scholar]
- 2015. Thailand Transport Portal. Number of New Registered Vehicles. Available from: http://www.apps.dlt.go.th/statistics_web/brochure/newcar15.pdf
- National variability in intracranial pressure monitoring and craniotomy for children with moderate to severe traumatic brain injury. Neurosurgery. 2013;73:746-52.
- [Google Scholar]
- Analysis of long-term (median 10.5 years) outcomes in children presenting with traumatic brain injury and an initial Glasgow Coma Scale score of 3 or 4. J Neurosurg Pediatr. 2015;16:410-9.
- [Google Scholar]
- Guidelines for the acute medical management of severe traumatic brain injury in infants, children, and adolescents – Second edition. Pediatr Crit Care Med. 2012;13(Suppl 1):S1-82.
- [Google Scholar]
- 2016. World Health Organization Violence Injury Prevention. Available from: http://www.who.int/violence_injury_prevention/policy/en/






