Translate this page into:
Impact of fibromyalgia severity on patients mood, sleep quality, and quality of life
*Corresponding author: Ruchi Singh, Department of Physiology, All India Institute of Medical Sciences, Bhopal, Madhya Pradesh, India. ruchi.physiology@aiimsbhopal.edu.in
-
Received: ,
Accepted: ,
How to cite this article: Singh R, Rai NK, Pathak A, Rai J, Pakhare A, Kashyap PV, et al. Impact of fibromyalgia severity on patients’ mood, sleep quality, and quality of life. J Neurosci Rural Pract. 2024;15:320-6. doi: 10.25259/JNRP_14_2024
Abstract
Objectives:
Fibromyalgia syndrome (FMS) is characterized by persistent widespread pain which greatly impacts the quality of life (QOL). Pain not only limits patients’ daily activities but also restricts their social activities further leading to depression, anxiety, and stress. The present cross-sectional study elucidated the association of sleep quality and mood with increasing symptom severity of fibromyalgia and its impact on the QOL of fibromyalgia patients.
Materials and Methods:
Hundred adult fibromyalgia patients diagnosed by the American College of Rheumatology 2010 criteria were evaluated for: sleep – using the Pittsburgh sleep quality index, QOL by SF-36, pain-visual analog scales (VASs) and global pain scale (GPS), mood-depression, anxiety, stress scale-21, somatic symptoms, anxiety and depression – by patients health questionnaire somatic, anxiety, and depressive symptom scales (PHQ-SADS), and FMS severity was evaluated using fibromyalgia impact questionnaire (FIQR).
Results:
The mean pain score was 6.80 ± 1.58 on VAS and 54.10 ± 14.33 on GPS. FIQR score was 50.62 ± 13.68, mean sleep quality was poor (9.30 ± 3.88), and depression, anxiety, and stress scores were increased (10.04 ± 4.59, 8.33 ± 4.48, and 10.75 ± 4.66). An increasing trend of depression, anxiety, stress, and somatoform symptoms was observed with an increase in the severity of FMS when patients were compared according to FMS severity scores. Sleep also deteriorated with increasing severity of FMS from 5.66 ± 1.92 in mild FMS to 12.0 ± 3.41 in highly severe FMS patients. The QOL too deteriorated in all the domains with increasing severity.
Conclusion:
With the increasing severity of fibromyalgia, not only does the pain increase but mood and sleep quality also deteriorate, which further impacts the QOL of FMS patients. Thus, comorbid mood derangements must also be screened and addressed for maximum benefit of the patients.
Keywords
Fibromyalgia
Sleep
Quality of life
Depression
Chronic pain
Anxiety
INTRODUCTION
Chronic and widespread pain in fibromyalgia syndrome (FMS) is not only associated with lowered pain threshold, increased touch sensitivity and fatigue but has shown significant impact on sleep as well as mood of the patients.[1,2] Sleep disturbances informed as difficulty falling asleep, frequent night-time awakenings, and unrefreshing sleep have directly been associated with pain in FMS in several observational studies.[3] More than 90% of patients with FMS suffer from sleep problems with non-restorative sleep being a common complaint.[4]
Poor sleep not only leads to a reduction in pain threshold but even reduces cognitive skills and increases chances of depression, anxiety, and stress among affected individuals.[5] Depression and anxiety are bi-directionally associated with sleep problems.[6] Sleep disturbances along with chronic pain and depression further exacerbate somatic and psychological symptoms and impact the quality of life (QOL) of individuals.[2,7] These symptoms lead to social isolation and reduction of interest in day-to-day activity, which further increases the disability with time, consequently leading to economic as well as social burden.[8]
Although sleep disturbances and depression are included in the American College of Rheumatology (ACR) criteria, they are still underexplored and are given less attention in FMS patient care.[9] The present study elucidated the association of sleep quality and mood with increasing symptom severity (SS) of fibromyalgia and its impact on the QOL of fibromyalgia patients.
MATERIALS AND METHODS
Design and ethics statement
This cross-sectional study was conducted to assess the status of depression, anxiety, stress, and sleep in different severity of fibromyalgia and its impact on QOL. The study was conducted in agreement with the ethical guidelines of the Declaration of Helsinki and was approved by the ethics committee of the institute. All the participants were enrolled only after written informed consent from them.
Setting
Individuals with fibromyalgia (screened using 2010 ACR criteria) attending outpatient department of a tertiary care institute in Central India from July 2021 to October 2022 were enrolled in the study [Figure 1].[2] The ACR criteria use two clinician-rated measures: Widespread Pain Index (WPI) and SS scale. The WPI represents the number of areas in which the patient has had pain over the past week and ranges from 0 to 19 while the SS scale ranges from 0–12 and is the sum of the severity of three symptoms: Fatigue, unrefreshing sleep, and cognitive symptoms, plus the severity of somatic symptoms in general.
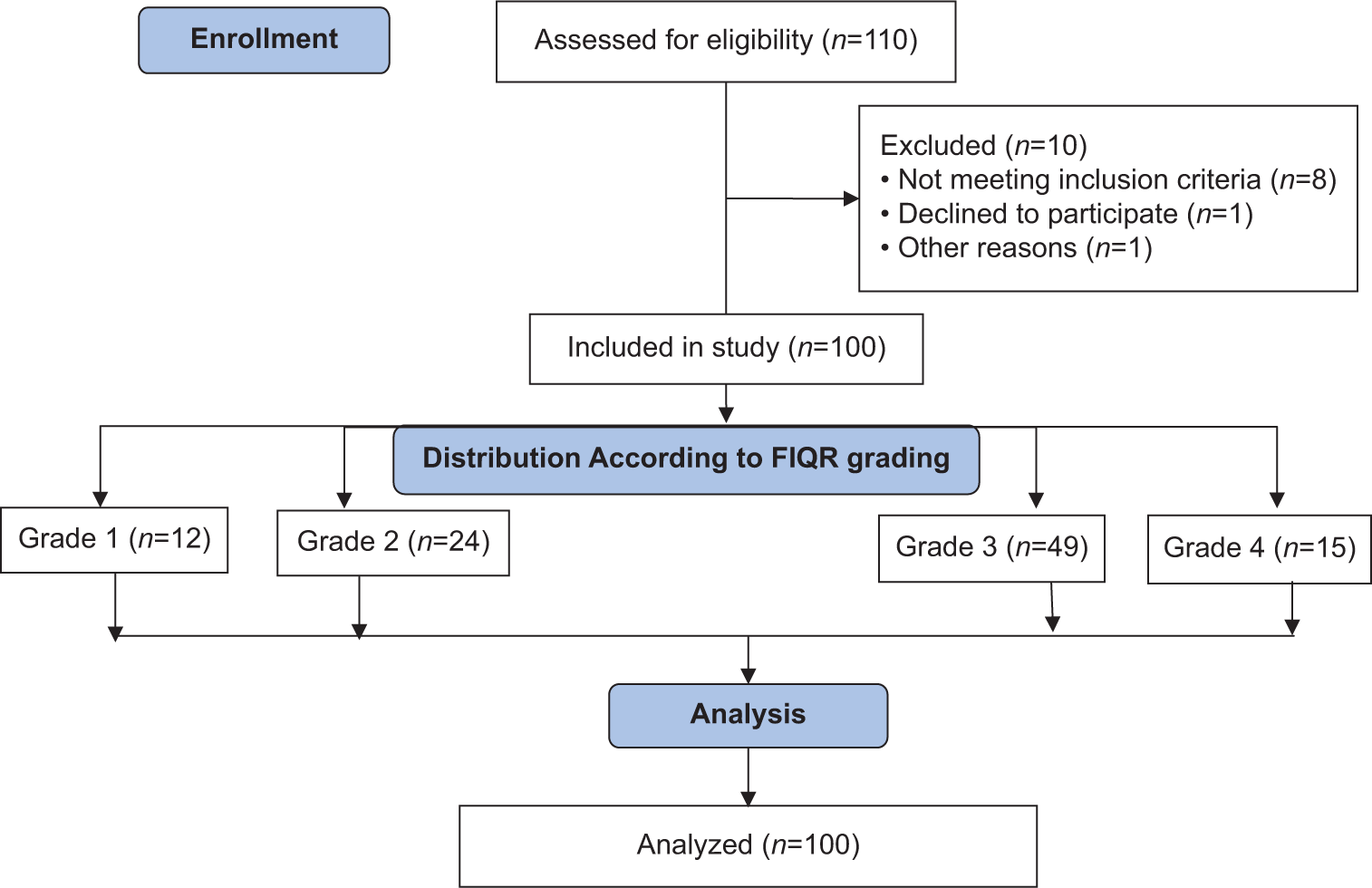
- Study flow diagram. FIQR: Fibromyalgia impact questionnaire.
All the patients, who met the following three criteria, were diagnosed to have FMS:[2]
WPI ≥ 7 and SS ≥ 5 or WPI 3–6 and SS ≥ 9
Symptoms have been present at a similar level for at least three months.
The patient does not have a disorder that would otherwise explain the pain.
Participants
Considering the prevalence of fibromyalgia as 7% sample size was calculated by the formula n = Z2 P (1−P)/d2; Z = 1.96; P = 0.07, d = 0.05.[10] Hundred patients of FMS (according to the ACR criteria 2010) of age >18 years of either gender were included in the study for further evaluation. Pregnant ladies and patients with other chronic neurological diseases were excluded from the study.
Study procedures
All the participants were assessed for their level of pain by global pain scale (GPS) and visual analog scale (VAS), quality of sleep, Pittsburgh sleep quality index (PSQI), patients health questionnaire somatic, anxiety, and depressive symptom scales (PHQ-SADS), and depression, anxiety, stress scale-21 (DASS-21), and QOL (SF-36). A revised fibromyalgia impact questionnaire (FIQR) was used to grade the severity of fibromyalgia as remission ≤30, mild severity >30 and ≤45, moderate severity >46 and ≤65, and high severity >65.[11] Participants completed these self-administered questionnaires using a standardized procedure, and the same instructions were given to all the participants to avoid any potential bias.
Assessment of pain
Pain among the participants was assessed using GPS and VAS. The GPS measures the experience of chronic pain. It has four subscales: Individuals’ pain, feelings, clinical outcome, and activities.[12] Twenty items are rated on an 11-point Likert-type scale ranging from strongly disagree to strongly agree.[11] The VAS is a widely used measure using points along the line labeled with intensity-denoting numbers from 0 to 10 to assess the severity of pain.[13]
Assessment of sleep
The PSQI was used to evaluate the overall quality of sleep over the past month. It has 19 subject-rated items on a 0 to 3 Likert rating scale, which are further grouped into seven components. Total score ranges from 0 to 21, with higher scores indicating poorer sleep quality. The PSQI score >5 indicates poor sleep quality.[14]
Assessment of mood and somatization
The PHQ-SADS is a combination of PHQ-15 to evaluate somatic symptoms with generalized anxiety disorder-7 (GAD-7) for anxiety and PHQ-9 for depression. The PHQ-15 consists of 15 items, each rated from 0 to 2; thus, the total score may range between 0 and 30.[15] The GAD-7 has 7 items, each scored from 0 to 3 and a total score ranging from 0 to 27.[16] The PHQ-9 is a continuous measure with scores ranging from 0 to 27 and cut points of 5, 10, 15, and 20 representing mild, moderate, moderately severe, and severe levels of depressive symptoms.[17]
The DASS-21 is a widely used patient-reported scale to measure emotional disturbances such as depression, anxiety, and stress. It has 21 items, each rated on a Likert scale ranging from 0 to 3. Total score ranges from 0 to 63.[18]
Assessment of QOL and severity of symptoms
The SF-36 was used to assess QOL. It has eight scales including physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional, and mental health.[19] The score for each scale varies from 0 to 100, and a higher score suggests a better QOL. Two final measures, that is, physical health and mental health were derived.
The FIQR is used to evaluate the QOL in fibromyalgia patients. It includes three domains (function with nine questions, overall impact with two questions, and symptoms having ten questions). Thus, 21 items are rated on an 11-point Likert scale with a range 0–10. Further, the total of the function domain is divided by 3 and that of the symptoms domain is divided by 2, overall domain remains unchanged, and a total FIQR score is the sum of these three values obtained with the maximum score being 100.[20] Higher scores indicate worse symptoms.
Statistical analysis
Data was collected using Microsoft Excel and was checked for outliers and duplications. Analysis was done using the Statistics Package for the Social Sciences version 16. Shapiro-Wilk test was used to test for normality of distribution of data. As the data was not distributed normally, non-parametric tests were used for analysis; thus, group comparison was made using the Kruskal–Wallis test to measure the variance of the numerical variables. Continuous variables are expressed as mean±standard deviation, while categorical data is expressed in absolute numbers and percentage values (%). The relationship between the variables was assessed using the Spearman coefficient of correlation. A two-tailed confidence interval of 95% was used in all statistical tests, and a probability (P) value <0.05 was used to determine the statistical significance.
RESULTS
As evident, our study also showed sexual dimorphism among the patients of FMS enrolled in this study, with 88% of patients being female. Participants were relatively young with a mean age of 38.58 ± 10.37 years. The mean VAS and GPS were 6.80 ± 1.58 and 54.10 ± 14.33, respectively, and the mean FIQR score was 50.62 ± 13.68 [Table 1]. To assess the status of different modalities among patients of different SS, they were grouped into four, based on their FIQR scores. Results show an increasing trend of all the mood disturbances, that is, depression, anxiety, stress, somatization, and deteriorating sleep quality with FMS SS.
| Variables (n=100) | Mean±SD; n(%) |
|---|---|
| Gender | |
| Males | 12 (12%) |
| Females | 88 (88%) |
| Age | 39.09±10.96 |
| SBP | 121.58±11.72 |
| DBP | 78.56±7.85 |
| Pulse rate | 74.06±10.87 |
| VAS | 6.80±1.58 |
| Global pain scale | 54.10±14.33 |
| PSQI | 9.30±3.88 |
| FIQR | 50.62±13.68 |
| PHQ-SADS (PHQ-15) | 11.94±4.03 |
| PHQ-SADS (GAD-7) | 11.38±4.09 |
| PHQ-SADS (PHQ-9) | 10.66±4.75 |
| Depression | 10.04±4.59 |
| Anxiety | 8.33±4.48 |
| Stress | 10.75±4.66 |
Data presented as n(%) and mean±SD: Standard deviation,SBP: Systolic blood pressure, DBP: Diastolic blood pressure, VAS: Visual analog scale for pain, PSQI: Pittsburgh sleep quality index, FIQR: Revised fibromyalgia impact questionnaire, PHQ-SADS: Patients health questionnaire somatic, anxiety, and depressive symptom scales, PHQ-15: Patients health questionnaire-15, GAD-7: Generalized anxiety disorder-7, PHQ-9: Patients health questionnaire-9 (PHQ-15, GAD-7, PHQ-9 explored by PHQ-SADS
Maximum patients had moderately severe FMS (n = 49), 15 had very severe grade FMS, 24 had mild, and the rest were in the remission group (n = 12). It was not only pain that increased significantly with increasing grade of FIQR, but all the psychological symptoms, including somatization, depression, anxiety, and stress, increased significantly (P = 0.0001). Sleep quality deteriorated from 5.66 ± 1.92 in the remission group to 12.0 ± 3.41 in the highly severe FMS group (P = 0.0001) [Table 2]. A significant positive correlation was observed between FMS severity on FIQR with the pain (VAS and GPS) deteriorating sleep quality (PSQI), somatization (PHQ-15), and mood, that is, depression, anxiety, and stress (GAD-7, PHQ-9, and DASS-21) as shown in Table 3.
| Variables | FIQR 1 (n=12) | FIQR 2 (n=24) | FIQR 3 (n=49) | FIQR 4 (n=15) | P-value | T statistics |
|---|---|---|---|---|---|---|
| ACR total | 13.58±1.24cd | 16.29±2.85 | 18.83±3.56a | 19.33±3.86b | <0.001* | 27.106 |
| VAS | 5.66±1.49cd | 6.45±1.35 | 7.02±1.65a | 7.53±1.30a | 0.007* | 12.210 |
| Global pain scale | 35.80±11.46cd | 45.50±13.78cd | 58.86±9.14ab | 66.93±8.99ab | <0.001* | 47.06 |
| PSQI | 5.66±1.92cd | 7.75±3.55d | 10.10±3.64a | 12.0±3.41ab | <0.001* | 25.96 |
| FIQR score | 27.76±3.84cd | 40.64±4.11cd | 54.99±6.26abd | 70.63±6.04abc | <0.001* | 85.24 |
| PHQ-15 | 8.33±3.17cd | 10.0±2.63cd | 13.18±4.20ab | 13.86±2.89ab | <0.001* | 23.26 |
| GAD-7 | 7.75±3.44cd | 9.66±3.69d | 12.08±3.55a | 14.73±3.71ab | <0.001* | 22.93 |
| PHQ-9 | 5.33±2.74cd | 7.95±3.80cd | 12.08±4.05ab | 14.60±3.62ab | <0.001* | 37.78 |
| Depression | 3.91±2.27cd | 8.29±3.40cd | 11.36±4.33ab | 13.40±2.52ab | <0.001* | 37.09 |
| Anxiety | 4.0±2.0cd | 6.04±3.98cd | 9.28±3.94ab | 12.33±3.75ab | <0.001* | 34.99 |
| Stress | 6.5±3.60cd | 8.33±4.65cd | 11.65±3.79ab | 15.06±3.17ab | <0.001* | 30.12 |
Kurskal–Wallis Test was applied as the data was non-parametric. Data presented as mean±standard deviation, df is 3, P<0.05 is significant “*”. ACR: American college of rheumatology, SBP: Systolic blood pressure, DBP: Diastolic blood pressure, VAS: Visual analog scale for pain, GPS: Global pain scale, PSQI: Pittsburgh sleep quality index, FIQR: Revised fibromyalgia impact questionnaire, PHQ-SADS: Patients health questionnaire somatic, anxiety, and depressive symptom scales, PHQ-15: Patients health questionnaire-15, GAD-7: Generalized anxiety disorder-7, PHQ-9: Patients health questionnaire-9 (PHQ-15, GAD-7, PHQ-9 explored by PHQ-SADS), DASS-21: Depression, anxiety, stress scale-21. aSignificant difference with FIQR-1 grade, bSignificant difference with FIQR-2 grade, cSignificant difference with FIQR-3 grade, dSignificant difference with FIQR4 grade
| Variables | R | P-value |
|---|---|---|
| VAS | 0.356 | <0.001* |
| Global pain scale | 0.733 | <0.001* |
| PSQI | 0.518 | <0.001* |
| PHQ-SADS (PHQ-15) | 0.508 | <0.001* |
| PHQ-SADS (GAD-7) | 0.488 | <0.001* |
| PHQ-SADS (PHQ-9) | 0.605 | <0.001* |
| Depression | 0.626 | <0.001* |
| Anxiety | 0.608 | <0.001* |
| Stress | 0.531 | <0.001* |
P<0.05 is significant “*”. Data presented as r: Spearman correlation coefficient, VAS: Visual analog scale for pain, GPS: Global pain scale, PSQI: Pittsburgh sleep quality index, FIQR: Revised fibromyalgia impact questionnaire, PHQ-SADS: Patients health questionnaire somatic, anxiety, and depressive symptom scales, PHQ-15: Patients health questionnaire-15, GAD-7: Generalized anxiety disorder-7, PHQ-9: Patients health questionnaire-9 (PHQ-15, GAD-7, and PHQ-9 explored by PHQ-SADS), DASS-21: Depression, anxiety, stress scale-21.
Health status measured by SF-36 showed that there was a significant difference in all the domains with poorer scores among the patients with higher FIQR grades [Figure 2]. The domain of emotional well-being did not reach statistical significance, and the scores were comparable among all four groups (FIQR1 = 48.33 ± 12.58; FIQR2 = 46.33 ± 11.55; FIQR3 = 43.75 ± 12.92), with the lowest among those with very severe FMS (FIQR4 = 37.60 ± 14.48). The domain of general health also registered poorer scores among all the four grades of FMS, with scores deteriorating with increasing severity (FIQR1 = 22.50 ± 9.65; FIQR2 = 18.95 ± 6.25; FIQR3 = 20.10 ± 11.79; and FIQR4 = 16.66 ± 17.99).
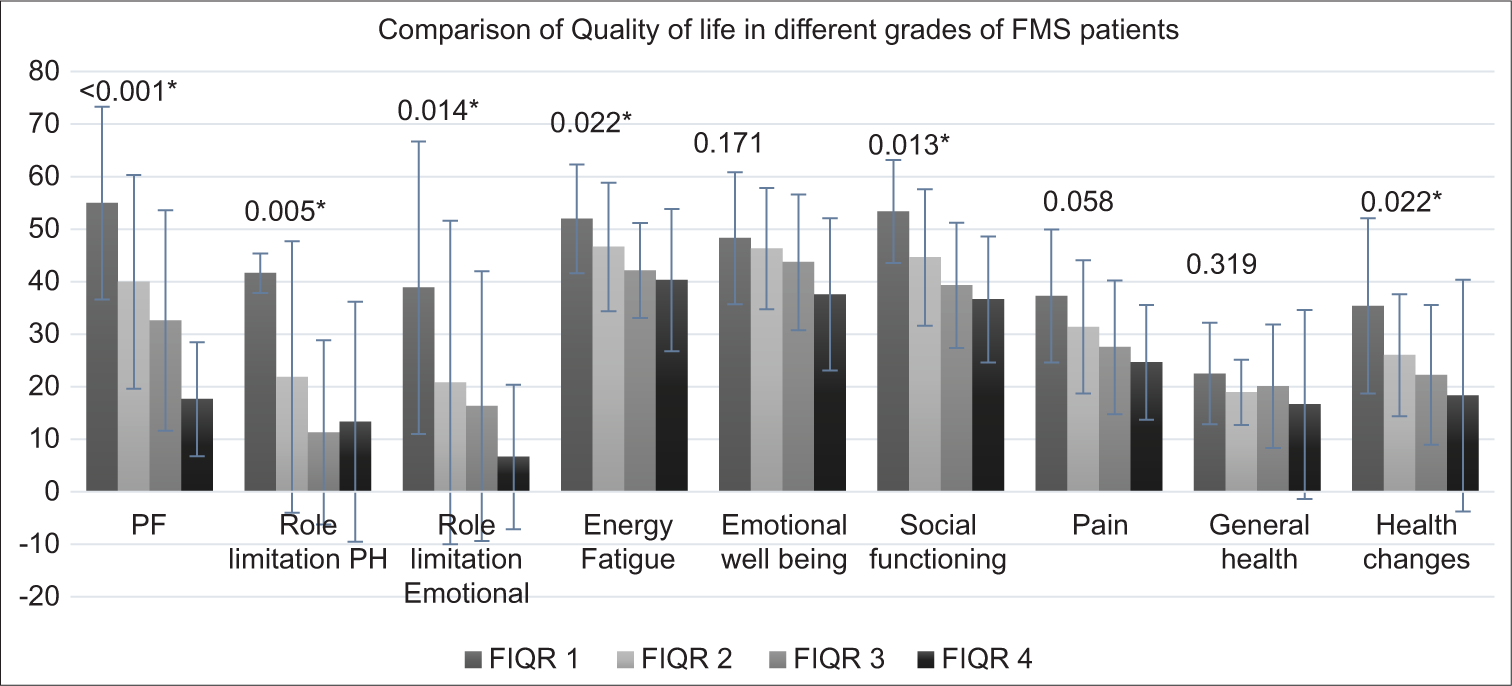
- FMS: Fibromyalgia syndrome, PF: Physical functioning, Role limitation PH: Role limitation physical health. The status of quality of life in different domains of quality of life among the patients with different grades of severity of fibromyalgia is shown with the comparative bar graph. The p-value of the comparative status is mentioned at the top of each domain bar graph. ”*” signifies statistically significant differences among patients with different grades of FMS severity, especially between grade1, 2 with grade 3, 4.
DISCUSSION
The present study explored the association of various physical as well as psychological symptoms with increasing fibromyalgia severity and assessed its impact on their QOL. This cross-sectional study enrolled 100 patients of FMS with different grades of severity, and it shows that it is not only pain that increases with the severity of the disease, but there is an overall deterioration in mood and quality of sleep, which further impacts their QOL.
Comorbidities such as sleep disturbances, depression, and anxiety have been suggested to facilitate the central nervous system in enhancing the sensitivity to pain.[21,22] A few of the suggested etiological factors for central sensitivity of pain include a temporal summation of noxious stimuli labeled as “Wind up” and/or inflammatory response (glial cell activation).[23,24] Studies have concluded that sleep deprivation causes alteration in descending pain inhibition, decreasing their effect, and thus leading to hyperalgesia.[25] Although the exact mechanism between sleep and the descending pain inhibitory system is still unknown, the most common areas affected in nociception, sleep deprivation, and descending pain inhibition are periaqueductal gray matter and raphe nuclei.[26,27] Repetitive stressful events and sleep deprivation may also cause glial cell overactivation. This inflammatory response affects brain function, increasing sensitivity to painful stimuli.[24] In the present study also, we observed that all the mood parameters, somatization, as well as sleep deteriorated in a graded fashion along with the increasing severity of pain, further deteriorating the QOL of FMS patients. Although sleep and depression have been shown to have a bidirectional association, the origin of the vicious cycle of depression, deteriorated sleep, and enhanced pain sensitivity remains obscure. A study by Rodero et al. on 326 FMS individuals evaluated pain severity according to stages of chronicity of fibromyalgia (according to the duration of the condition).[28] They concluded that psychological parameters change over time. They also suggested that these parameters are predictors for marking the stages of chronicity and change with respect to the duration of the condition. However, they too were unclear whether the duration of fibromyalgia enhances the comorbidities or it is the comorbidities that increase the severity of the disease.
Bigatti et al.[29] reported that sleep is a core symptom of fibromyalgia and plays a crucial role in exacerbating symptoms such as pain, depression, and anxiety. However, Alok et al.[30] have shown that the negative effects (depression, stress, and anxiety) are also associated with severity of FMS, and the magnitude of the results is correlated with the FIQR score. However, they did not comment on the association of sleep with FMS severity. Singh et al.[31] also reported that patients of FMS have poorer sleep quality as well as QOL compared to healthy participants. However, they did not comment on the mood as well as its association with sleep in FMS.[31] Although, they indicated that poorer sleep quality could be one of the predictors of FMS severity, the sample size in their study was quite small. The present study also correlated with OMERACT (Outcome Measures in Rheumatology Clinical Trials) FMS domain, that is, pain, sleep, cognitive dysfunction, and anxiety, but it concluded that the hierarchy of the core domains may be different in patients with high severity as compared to those with low severity.[32]
Türkoğlu and Selvi[33] and Theadom et al.[34] have concluded that the standard forms of treatment approaches might not be effective enough if sleep and other psychological symptoms are not taken into consideration.[33,34] Secondary analysis of four randomized control trials, including 1332 FMS patients by Marangell et al.[35] showed that direct therapy for chronic pain rehabilitation was responsible for almost 70% of pain relief. However, the rest 30% relief in pain was due to improvement in mood due to indirect effect. Thus, the focus on domains other than pain is also important to enhance the recovery with the downstream severity of the disease.
With the present study, the status of comorbidities in FMS was recorded, and it showed that greater severity of FMS was associated with a higher grade of mood derangements, somatization, and sleep disturbances. The limitation of this study was that it was a cross-sectional study; thus, the direction of association of these comorbidities with pain in FMS could not be commented on.
CONCLUSION
With increasing FMS severity, not only pain increased but sleep, depression, anxiety, somatization, and QOL also deteriorated. Further, these symptoms correlated significantly with each other. Since FMS is associated with increased pain perception and worsened QOL, comorbid mood derangements too, must also be properly screened and addressed for the maximum benefit of the patients. As available treatments are mainly oriented toward pain, they can reach a limit of benefit to these FMS patients. The well-being of these patients could be maximized by additionally addressing these comorbidities as well. A holistic treatment approach addressing both physical as well as psychological improvement of FMS patients could be beneficial for FMS patients.
Ethical approval
The research/study approved by the Institutional Review Board at AIIMS BHOPAL, number IHEC-LOP/2020/EF0148, dated May 7, 2020.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
DST –Satyam.
References
- Influence of stress systems and physical activity on different dimensions of fatigue in female fibromyalgia patients. J Psychosom Res. 2017;93:55-61.
- [CrossRef] [PubMed] [Google Scholar]
- The American College of Rheumatology preliminary diagnostic criteria for fibromyalgia and measurement of symptom severity. Arthritis Care Res. 2010;62:600-10.
- [CrossRef] [PubMed] [Google Scholar]
- Patient perspectives on the impact of fibromyalgia. Patient Educ Couns. 2008;73:114-20.
- [CrossRef] [PubMed] [Google Scholar]
- The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum. 1995;38:19-28.
- [CrossRef] [PubMed] [Google Scholar]
- The association between pain and sleep in fibromyalgia. Saudi Med J. 2017;38:465-75.
- [CrossRef] [PubMed] [Google Scholar]
- The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 2015;11:513-20.
- [CrossRef] [PubMed] [Google Scholar]
- Catastrophizing and pain in arthritis, fibromyalgia, and other rheumatic diseases. Arthritis Rheum. 2006;55:325-32.
- [CrossRef] [PubMed] [Google Scholar]
- Societal and patient burden of fibromyalgia syndrome. Pharmacoeconomics. 2009;27:547-59.
- [CrossRef] [PubMed] [Google Scholar]
- Screening and management of sleep disorders in patients with fibromyalgia syndrome: A French multicentred, prospective, observational study protocol (FIBOBS) BMJ Open. 2022;12:e062549.
- [CrossRef] [PubMed] [Google Scholar]
- Prevalence of fibromyalgia: Literature review update. Rev Bras Reumatol Engl Ed. 2017;57:356-63.
- [CrossRef] [PubMed] [Google Scholar]
- Definition of fibromyalgia severity: Findings from a cross-sectional survey of 2339 Italian patients. Rheumatology (Oxford). 2021;60:728-36.
- [CrossRef] [PubMed] [Google Scholar]
- A longitudinal analysis of total pain scores for a panel of patients treated by pain clinics. Health Serv Res Manag Epidemiol. 2019;6:2333392818788420.
- [CrossRef] [PubMed] [Google Scholar]
- Analysis of outcome measures for persons with patellofemoral pain: Which are reliable and valid? Arch Phys Med Rehabil. 2004;85:815-22.
- [CrossRef] [PubMed] [Google Scholar]
- The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193-213.
- [CrossRef] [PubMed] [Google Scholar]
- Detecting somatoform disorders in primary care with the PHQ-15. Ann Fam Med. 2009;7:232-8.
- [CrossRef] [PubMed] [Google Scholar]
- A brief measure for assessing generalized anxiety disorder: The GAD-7. Arch Intern Med. 2006;166:1092-7.
- [CrossRef] [PubMed] [Google Scholar]
- The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606-13.
- [CrossRef] [PubMed] [Google Scholar]
- Psychometric properties of the Depression Anxiety Stress Scales (DASS) in clinical samples. Behavi Res Ther. 1997;35:79-89.
- [CrossRef] [PubMed] [Google Scholar]
- Quality of life and discriminating power of two questionnaires in fibromyalgia patients: Fibromyalgia impact questionnaire and medical outcomes study 36-item short-form health survey. Rev Bras Fisioter. 2010;14:284-9.
- [CrossRef] [PubMed] [Google Scholar]
- The revised fibromyalgia impact questionnaire (FIQR): Validation and psychometric properties. Arthritis Res Ther. 2009;11:R120.
- [CrossRef] [PubMed] [Google Scholar]
- Depression and the long-term risk of pain, fatigue, and disability in patients with rheumatoid arthritis. Arthritis Rheum. 1998;41:1851-7.
- [CrossRef] [PubMed] [Google Scholar]
- Symptoms of depression predict the trajectory of pain among patients with early inflammatory arthritis: A path analysis approach to assessing change. J Rheumatol. 2009;36:231-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evoked pain measures in fibromyalgia. Best Pract Res Clin Rheumatol. 2003;17:593-609.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep disturbances and severe stress as glial activators: Key targets for treating central sensitization in chronic pain patients? Expert Opin Ther Targets. 2017;21:817-26.
- [CrossRef] [PubMed] [Google Scholar]
- One night of total sleep deprivation promotes a state of generalized hyperalgesia: A surrogate pain model to study the relationship of insomnia and pain. Pain. 2013;154:1613-21.
- [CrossRef] [PubMed] [Google Scholar]
- Identification of wake-active dopaminergic neurons in the ventral periaqueductal gray matter. J Neurosci. 2006;26:193-202.
- [CrossRef] [PubMed] [Google Scholar]
- Brainstem modulation of pain during sleep and waking. Sleep Med Rev. 2003;7:145-54.
- [CrossRef] [PubMed] [Google Scholar]
- Stages of chronicity in fibromyalgia and pain catastrophising: A cross-sectional study. BMC Musculoskelet Disord. 2010;11:251.
- [CrossRef] [PubMed] [Google Scholar]
- Sleep disturbances in fibromyalgia syndrome: Relationship to pain and depression. Arthritis Rheum. 2008;59:961-7.
- [CrossRef] [PubMed] [Google Scholar]
- Relationship of severity of depression, anxiety and stress with severity of fibromyalgia. Clin Exp Rheumatol. 2011;29:S70-2.
- [Google Scholar]
- Impact of sleep disturbances and autonomic dysfunction on the quality of life of patients with fibromyalgia. J Basic Clin Physiol Pharmacol. 2021;32:1021-9.
- [CrossRef] [PubMed] [Google Scholar]
- Fibromyalgia syndrome module at OMERACT 9: Domain construct. J Rheumatol. 2009;36:2318-29.
- [CrossRef] [PubMed] [Google Scholar]
- The relationship between chronotype, sleep disturbance, severity of fibromyalgia, and quality of life in patients with fibromyalgia. Chronobiol Int. 2020;37:68-81.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the role of sleep and coping in quality of life in fibromyalgia. J Psychosom Res. 2007;62:145-51.
- [CrossRef] [PubMed] [Google Scholar]
- Comparative pain and mood effects in patients with comorbid fibromyalgia and major depressive disorder: Secondary analyses of four pooled randomized controlled trials of duloxetine. Pain. 2011;152:31-7.
- [CrossRef] [PubMed] [Google Scholar]






