Translate this page into:
Idiopathic Hypoparathyroidism Presenting As New Onset Refractory Status Epilepticus
Divya M. Radhakrishnan, MD, DM Department of Neurology Room No 602, 6th floor, CN center, All India Institute of Medical Sciences, New Delhi 110029 India dr.divyamr@gmail.com
This article was originally published by Thieme Medical and Scientific Publishers Pvt. Ltd. and was migrated to Scientific Scholar after the change of Publisher.
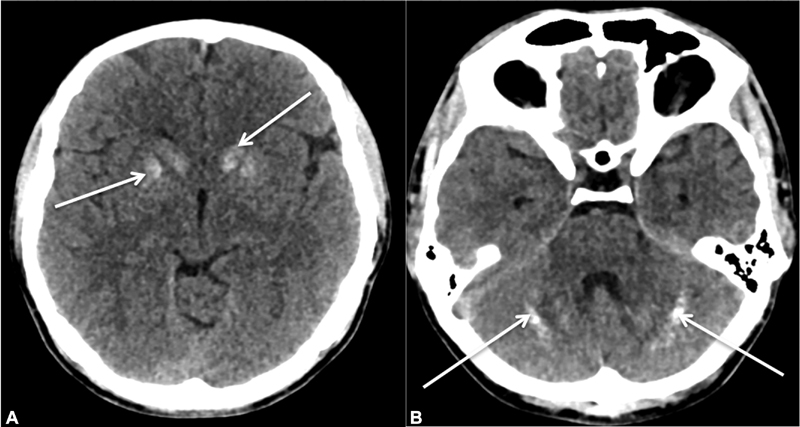
A 23-year-old male, presented with a flurry of new onset generalized tonic clonic seizures and impaired sensorium. He was intubated and managed as a case of status epilepticus with intravenous lorazepam followed by multiple anti seizure medications (ASM) and midazolam infusion. His initial laboratory reports revealed hypocalcemia (4.8 mg/dL) (ref range: 8–11 mg/dL) with normal sodium, potassium, magnesium, and phosphorus levels. His blood sugar, renal, and liver function tests were also within normal limits. Further evaluation showed low intact parathyroid hormone <3 pg/mL (ref range: 15–68.3 pg/mL) and Vitamin D3 (22 ng/mL) (ref range 30–100 ng/mL) levels. Computed tomography (CT) of brain showed calcifications in bilateral caudate, lentiform nucleus, and cerebellar hemispheres (Fig. 1A, B). Ultrasound abdomen and CT scan of neck were normal. With the diagnosis of idiopathic hypoparathyroidism, he was treated with parenteral and oral calcium preparations, along with Vitamin D3 under cardiac monitoring. With correction of hypocalcemia his seizures got controlled; he was extubated and ASM were tapered. He was discharged on oral calcium (1,000 mg/d) with calcitriol (0.5 µg/d) supplementation and was seizure free at 3 months follow-up.
-
Fig. 1 (A) Non–contrast computed tomography (NCCT) head axial view showing bilateral calcification of caudate nucleus and putamen (white arrows). (B) NCCT head axial view showing cerebellar calcification (white arrows).
Fig. 1 (A) Non–contrast computed tomography (NCCT) head axial view showing bilateral calcification of caudate nucleus and putamen (white arrows). (B) NCCT head axial view showing cerebellar calcification (white arrows).
Hypoparathyroidism is one of the most common cause of intracranial calcification (IC). Basal ganglia is the usual site and calcification beyond extrapyramidal system (cerebellum, thalamus, or subcortical white matter) is infrequent.1 Though seizures are noted in 30 to 70% of patients, new onset refractory status epilepticus as the presenting symptom of idiopathic hypoparathyroidism is extremely rare.2 3 Seizures are attributed to hypocalcemia and IC in vascular and perivascular area.4 Treatment of seizures includes prompt administration of high dose intravenous calcium followed by long-term oral supplementation of calcium and calcitriol.5 ASM that induce cytochrome P450 (CYP) isoenzymes can worsen hypocalcemia and should preferably be avoided in these patients. Hypocalcemia with IC can be a diagnostic clue for hypoparathyroidism; prompt treatment with calcium and vitamin D results in seizure freedom and prevents further neurological complications.
Acknowledgment
The authors acknowledge gratitude to their patient and family.
Conflict of Interest
None declared.
Funding None.
References
- Neurological picture. Extensive brain calcification in idiopathic hypoparathyroidism. J Neurol Neurosurg Psychiatry. 2006;77(12):1328.
- [Google Scholar]
- Epileptic seizure, as the first symptom of hypoparathyroidism in children, does not require antiepileptic drugs. Childs Nerv Syst. 2017;33(2):297-305.
- [Google Scholar]
- Acute symptomatic seizures caused by electrolyte disturbances. J Clin Neurol. 2016;12(1):21-33.
- [Google Scholar]
- Widespread intracranial calcification, seizures and extrapyramidal manifestations in a case of hypoparathyroidism. N Am J Med Sci. 2012;4(8):369-372.
- [Google Scholar]





